Keywords
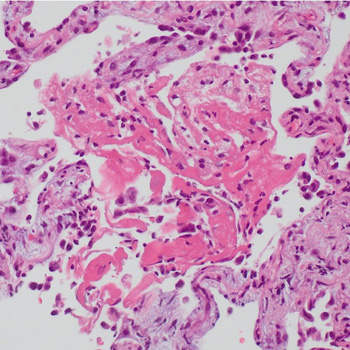
Pulmonary aspergillosis, pulmonary infarction, organising pneumonia
Abstract
A patient initially treated with corticosteroids for cryptogenic organising pneumonia following pulmonary infarction, developed a worsening condition with progressive cavitary formations in both lower lung lobes. Contrast-enhanced chest computed tomography revealed a pulmonary embolism, and serum anti-Aspergillus IgG antibody analysis yielded a strong positive result. Consequently, the patient was diagnosed with pulmonary infarction with Aspergillus infection; organising pneumonia in surrounding areas reflected the repair process. Following treatment with anticoagulants and antifungal agents, the patient was successfully discharged. Hence, pulmonary infarction should be considered in cases of refractory lung lesions.
References
Views: 43
HTML downloads: 3
PDF downloads: 26
Published:
2024-04-22
Issue:
2024: LATEST ONLINE
(view)