Keywords
Immunosuppression, Nocardia cyriacigeorgica, Asperigillus
Abstract
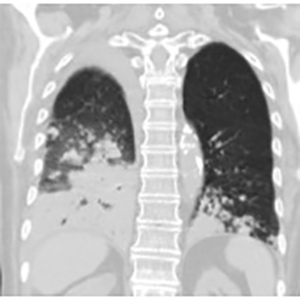
Immunosuppressed patients are at greater risk of unusual infections. The authors present the case of a woman with giant-cell arteritis, on oral steroids, who developed cavitating pneumonia due to co-infection with Asperigillus and Nocardia. Reports of such co-infection are rare in the literature. This case highlights the importance of considering rare pathogens in immunosuppressed patients who present with non-specific symptoms, as well as the impact of such pathogens on clinical management. Another important issue is the need for prophylaxis against Nocardia spp. in immunocompromised patients.
References