Keywords
Pulmonary embolism, alteplase, pericardiocentesis, pericardial effusion, thrombolytic therapy
Abstract
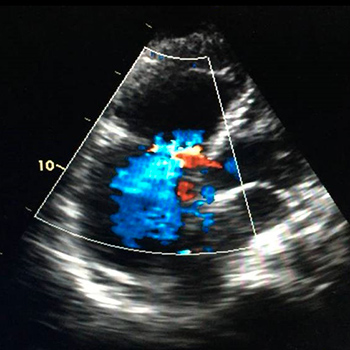
Background: The occurrence of a high-risk pulmonary embolism (PE) within 48 hours of a complicated pericardiocentesis to remove a haemorrhagic pericardial effusion, is an uncommon clinical challenge.
Case summary: The authors report the case of a 75-year-old woman who presented with signs of imminent cardiac tamponade due to recurring idiopathic pericardial effusion. The patient underwent pericardiocentesis that was complicated by the loss of 1.5 litres of blood. Within 48 hours, the patient had collapsed with clear signs of obstructive shock. This was a life-threating situation so alteplase was administered after cardiac tamponade and hypertensive pneumothorax had been excluded. CT chest angiography later confirmed bilateral PE. The patient achieved haemodynamic stability less than an hour after receiving the alteplase. However, due to the high risk of bleeding, the medical team suspended the thrombolysis protocol and switched to unfractionated heparin within the hour. The cause of the PE was not identified despite extensive study, but after 1 year of follow-up the patient remained asymptomatic.
Discussion: Despite the presence of a contraindication, the use of thrombolytic therapy in obstructive shock after exclusion of hypertensive pneumothorax can be life-saving, and low-dose thrombolytic therapy may be a valid option in such cases.
References
Views: 1014
HTML downloads: 147
PDF downloads: 412
Published:
2019-07-15
Issue:
Vol 6 No 7
(view)