Keywords
Septic thrombophlebitis, Lemierre, Rickettsia, Thrombophilia, Streptococcus gordonii
Abstract
Aims: Lemierre syndrome is a life-threating condition characterized by recent oropharyngeal infection, internal jugular vein thrombosis, and anaerobic septicemia. It is usually caused by Fusobacterium necrophorum.
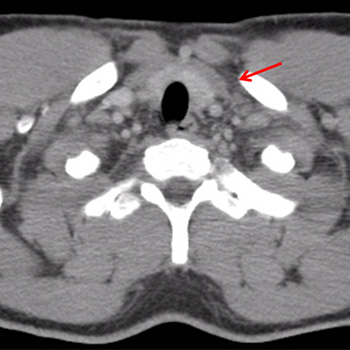
Methods: A young Romanian male presented with fever and rigors, mild tachypnea, hypoxia, sore throat, decayed teeth, and tenderness of the left carotid triangle. Laboratory examination indicated severe sepsis with disseminated intravascular coagulation, acute renal failure, and acute respiratory distress syndrome while the Doppler ultrasonography of the carotids revealed left internal jugular venous thrombosis. The patient was administered piperacillin/tazobactam and vancomycin intravenously, doxycycline orally, and anti-coagulation by enoxaparin based on the diagnosis of Lemierre syndrome. Meanwhile, he was complicated by bilateral diffuse pulmonary cavities and encapsulated pleural effusions and so transcutaneous drainage was performed. The patient was discharged after a month and continued his treatment with oral phenoxypenicillin and doxycycline until full radiographic improvement. He was switched to oral anti-coagulation by vitamin-K antagonists and was referred to a hematologist, a vascular-surgeon, and a dentist.
Results: Streptococcus gordonii was isolated from the patient’s blood and pleural fluid cultures and serology for Rickettsial spp. IgM was positive. Thrombophilia genetic tests revealed three minor mutations for fibrinogen-455, plasminogen activator inhibitor-1, and methylenetetrahydrofolate reductase. According to the literature, S. gordonii is not usually a causative agent and Rickettsial spp. have as yet not been correlated with Lemierre syndrome. The failure of left jugular vein recanalization shows a possible causative role of the underlying thrombophilic predisposition.
Discussion: Because of the syndrome’s rarity and the atypical microorganisms isolated in this case, increased awareness is advised for its diagnosis and the underlying mechanisms involved in its genesis. The role of anti-coagulation is debatable.
References
Views: 1479
HTML downloads: 317
PDF downloads: 451
Untitled downloads: 0
Figures downloads: 0
Published:
2017-06-29
Issue:
Vol. 4 No. 5
(view)