Keywords
Anterior ischaemic optic neuropathy, eosinophilia, eosinophilic granulomatosis with polyangiitis, vasculitis, visual loss
Abstract
Background: eosinophilic granulomatosis with polyangiitis (EGPA) is a rare multisystem inflammatory disease characterized by asthma, eosinophilia and granulomatous or vasculitic involvement of various organs. While the eye is uncommonly affected in patients with EGPA, multiple ophthalmic manifestations have been reported, which can result in serious visual impairment without timely treatment.
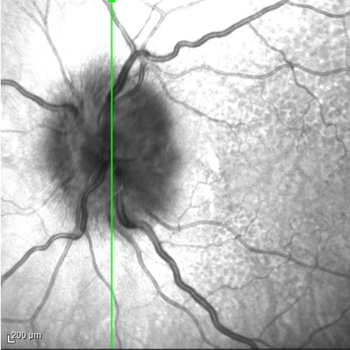
Case report: we report the case of a 79-year-old woman with a history of asthma and nasal polyps who presented with low-grade fever, mild alteration of mental status, and fatigue. Chest X-ray revealed bilateral interstitial infiltrates. Lab tests showed elevated C-reactive protein level and eosinophilia (eosinophil count, 4.6 x109 cells/l); blood cultures and parasitological examination of stools tested negative. Four days after presentation, the patient reported sudden and severe blurring of vision in her left eye. Ophthalmological examination revealed bilateral swollen optic disc and visual field loss, more severe in the left eye. A diagnosis of EGPA complicated by arteritic anterior ischaemic optic neuropathy (A-AION) was proposed, while an alternative or concurrent diagnosis of giant cell arteritis was ruled out based on clinical picture.
Immunosuppressive treatment with high-dose intravenous glucocorticoids was promptly started. The patient’s visual defect did not improve; however, two months later, no worsening was registered on ophthalmic reassessment.
Conclusions: A-AION is an infrequent but severe manifestation of EGPA, requiring prompt diagnosis and emergency-level glucocorticoid therapy to prevent any further vision loss. Disease awareness and a multidisciplinary approach are crucial to expedite diagnostic work-up and effective management of EGPA-related ocular complications.
References
Views: 124
HTML downloads: 36
PDF downloads: 94
Published:
2024-03-21
Issue:
2024: Vol 11 No 4
(view)