ABSTRACT
Acute non-rheumatic streptococcal myopericarditis (ANRSM) is a rare complication of an upper airway infection by streptococcus group A in developed countries. Cardiac involvement in bacterial infections must be adequately treated because it can lead to long-term complications. This case report describes recurrent ANRSM in an 18-year-old man, which illustrates how difficult and challenging the diagnosis of this disease can be.
LEARNING POINTS
- In developed countries, acute non-rheumatic streptococcal myopericarditis is a rare complication of an upper airway infection by streptococcus group A and can mimic acute myocardial infection with ST elevation.
- The diagnosis is made on the basis of a recent upper airway infection by streptococcus group A in the absence of a rheumatic setting.
- Cardiac imaging (mainly ultrasound and magnetic resonance) plays a major role in making the diagnosis.
- Prognosis is very good when appropriate treatment with antibiotics and non-steroidal inflammatory drugs is provided.
KEYWORDS
Acute non-rheumatic myopericarditis, Streptococcus group a, cardiac magnetic resonance, upper airway infection
INTRODUCTION
Acute non-rheumatic streptococcal myopericarditis (ANRSM) is a rare complication of an upper airway infection by streptococcus group A (GAS), appearing 2–5 days after the initial respiratory symptoms. ANRSM presentation may be identical to that of acute myocardial infarction (AMI), with sudden chest pain with ST elevation on electrocardiogram[1] The incidence, aetiology and pathology of ANRSM are still uncertain[2], with a suggestion that myopericardial inflammation and damage is caused by IgG-binding proteins produced by GAS antigens that cross-react with cardiac myosin[3]. As ANRSM and AMI share the same electrocardiographic and laboratory findings, coronary angiography is mandatory in the acute setting. Younger age, no previous cardiovascular risk factors and recent upper airway infection should alert the clinician to the possibility of ANRSM; however, in cases of doubt the patient should be treated as if they have AMI with ST elevation[4]. Non-rheumatic streptococcal disease is increasingly recognized as a cause of myopericarditis, in part due to the expanding availability of rapid diagnostic testing for both acute streptococcal disease (rapid streptococcal antigen tests) and acute myocardial injury (sensitive troponin assays)[2].
CASE REPORT
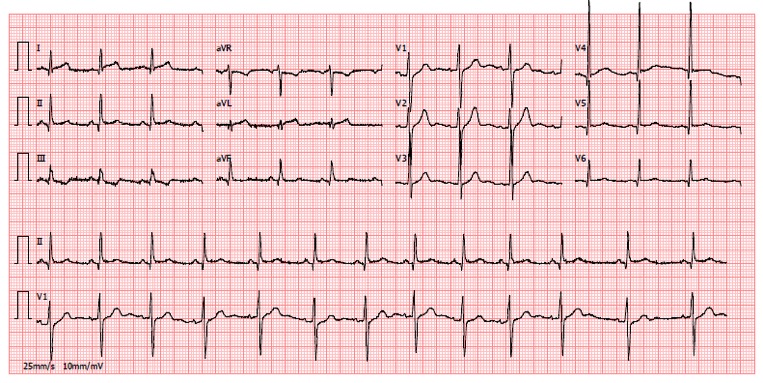
The authors present the case of an 18-year-old man with no previous medical history and not taking chronic medication. He worked at his parent’s bar, and was a social smoker and drinker with no other known cardiovascular risk factors. He was referred to our hospital for suspected ST-elevation AMI. He had a stabbing chest pain lasting for 6 hours that did not improve with a single dose of ibuprofen 400 mg. The ECG showed a slight ST elevation on V4–V6, DI, aVL and DII (Fig. 1). Blood analysis showed leucocytosis of 15.40×103/µl (normal range 4–10×103/µl), an elevated C-reactive protein (CRP) of 1.3 mg/dl (normal range <0.8 mg/dl) and a very high troponin I value of 15.80 ng/ml (normal range <0.034 ng/ml).
Figure 1. ECG recorded on admission for the first episode of chest pain showing ST elevation on V4–V6, DI and aVL
An echocardiogram showed normal left ventricular function with no valvular disease or pericardial effusion, but due to the abrupt onset of symptoms and elevated troponin, the patient was submitted to urgent coronary angiography that revealed normal coronary arteries. The patient was put on 24-hour ECG recording that did not reveal any pathological dysrhythmias. Therefore, the diagnosis of myopericarditis of viral aetiology was presumed on the basis of the history of an upper airway infection in the previous week. Treatment with acetylsalicylic acid 1 g three times a day and colchicine 0.5 mg two times a day was started. The patient was discharged on the third day after resolution of the chest pain, with a scheduled follow-up consultation 21 days later.
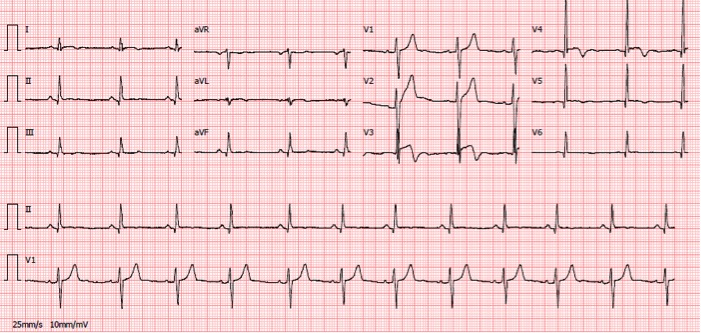
One week before the scheduled consultation, the patient had another episode of sudden chest pain with the same characteristics. Simultaneously he had complaints of odynophagia and tonsillitis which was treated with azithromycin 500 mg a day Physical examination was unremarkable except for the oropharynx which showed inflammatory signs with bilateral tonsillar oedema and a purulent plaque. The ECG at admission showed ST elevation from V3 to V5 and T wave inversion on DI, aVL, V3 and V4 (Fig. 2).
Figure 2. ECG recorded on admission for the second episode of chest pain showing ST elevation on V3–V5 and T wave inversion on DI, aVL, V3, V4 and V5
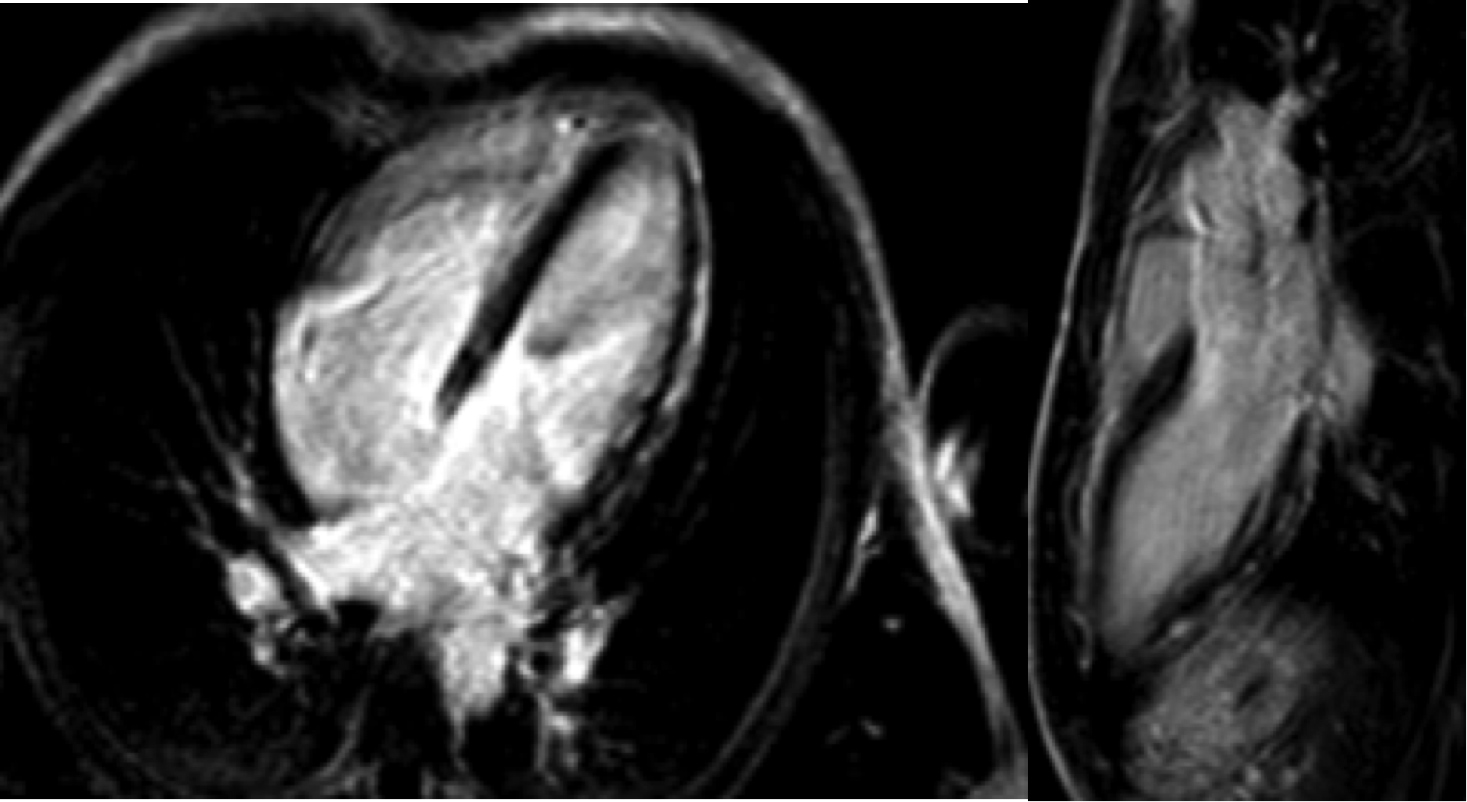
Blood analysis showed an elevated troponin I of 5.87 ng/ml, leucocytosis of 10.40×103/µl with 68.7% neutrophils, and a C-reactive protein of 9.7 mg/dl. The diagnosis was recurrent myopericarditis of unknown aetiology, which led to a wider search for the cause. Serology tests for HIV, HCV, HBV, EBV, CMV, herpes virus, adenovirus, Coxsackie virus and syphilis were all negative. Autoimmune pathology was also excluded. As the aetiology was still unknown, cardiac magnetic resonance imaging was performed and showed subepicardial enhancement in the inferolateral wall in the late enhancement sequence, suggestive of myocarditis/myopericarditis (Figs. 3-4). The association between the two respiratory infections and both episodes of chest pain led us to consider a possible pathological connection. Therefore, a rheumatic factor rapid antigen swab test and an antistreptolysin O titre test were performed; the first was negative but the latter was positive with an antistreptolysin O of 2,110 IU/ml (normal range <200 IU/ml). Antibiotic therapy was changed to amoxicillin 500 mg three times a day, and the diagnosis of ANRSM was made based on the clinical presentation, time line since the pharyngitis/tonsillitis caused by GAS, and cardiac MRI images. The patient was also referred for otolaryngologist evaluation for tonsillectomy due to the high risk of recurrence of myopericarditis associated with another upper airway infection.
Figure 3. Cardiac MRI late gadolinium enhancement study showing foci of subepicardial enhancement in the inferolateral wall
Figure 4. Figure 4 T2-weighted sequence showing signal hyperintensity in the middle segment of the inferolateral wall
DISCUSSION
This case discusses a rare presentation of myopericarditis, which is sometimes overlooked due to the decreasing incidence of complications associated with infections by GAS in developed countries[5]. Nonetheless, we should keep in mind complications such as rheumatic fever and ANRSM, as the first is associated with valvular damage and life-long complications that negatively impact quality of life. ANRSM has a more benign course, without chronic damage to the heart if antibiotic and non-steroidal inflammatory drugs (NSAIDs) are started at the appropriated time. The true incidence of ANRSM is not known because the diagnosis is often missed and an idiopathic diagnosis made. Clinicians must be alert when a young patient without cardiovascular risk factors experiences sudden-onset chest pain with ST segment elevation on ECG. After acute coronary syndrome is excluded, the possible association between an upper airway infection that appeared 3–7 days previously and an acute episode of chest pain should be considered[6]. If the diagnosis is suspected, a rapid antigen test and antistreptolysin O test should be requested, while cardiac MRI is recommended to confirm the characteristic findings of late gadolinium enhancement.
This case is especially interesting because the patient experienced two episodes of ANRSM in a short period of time, as confirmed by the presence of very high antistreptolysin O titres suggesting a recent infection (first episode), and a positive rapid antigen test indicating an acute infection (second episode). This is not the first case of recurrent ANRSM described in the literature[2], indicating that this patient may experience more episodes if he develops tonsillitis in the future. In such cases tonsillectomy is strongly recommended.
CONCLUSION
ANRSM is rare condition that is underdiagnosed. We should be alert to this diagnosis when a young healthy person presents with acute chest pain with ST elevation and AMI is excluded. The diagnosis is based on a clinical history of upper airway infection by GAS that precedes the chest pain and cardiac MRI findings. The prognosis is good when appropriate therapy is provided.