ABSTRACT
Introduction: In-situ right atrial (RA) thrombus is a rare occurrence typically associated with heightened inflammatory or hypercoagulable states. Here, we present a case of in-situ RA thrombus mimicking atrial myxoma in a patient with sepsis and bacteraemia.
Case description: A 41-year-old man presented with septic arthritis and bacteraemia caused by methicillin-resistant Staphylococcus aureus (MRSA). A transoesophageal echocardiogram revealed a large pediculated mass resembling atrial myxoma, which was not visible on transthoracic echocardiography performed four days earlier. Cardiac magnetic resonance (CMR) imaging strongly suggested a thrombus, leading to the patient undergoing transcatheter aspiration. Subsequent pathology confirmed an organised fibrin thrombus without evidence of infection.
Discussion: The patient’s in-situ RA thrombus likely developed in response to a heightened inflammatory state associated with sepsis. Limited data exist on in-situ RA thrombi in the absence of atrial fibrillation, though some reports suggest a correlation between heightened inflammation and a hypercoagulable state.
Conclusion: CMR imaging is invaluable for characterising such masses and can aid in distinguishing a thrombus from a myxoma.
KEYWORDS
Right atrial thrombus, cardiac mass, transcutaneous aspiration
LEARNING POINTS
- Differentiating right atrial (RA) thrombus from myxoma: cardiac magnetic resonance imaging is essential for distinguishing RA thrombus from myxoma, preventing unnecessary surgeries.
- Hypercoagulable and inflammatory states: spontaneous in-situ RA thrombi can occur without deep vein thrombosis (DVT) or atrial fibrillation, especially in hypercoagulable and inflammatory conditions.
- Transcatheter aspiration: this less invasive alternative to surgery is effective for large, mobile RA thrombi, reducing embolisation risk.
INTRODUCTION
An in-situ right atrial (RA) thrombus is a rare occurrence and can masquerade as other cardiac tumours, notably cardiac myxoma[1]. The connection between a free-floating thrombus and deep vein thrombosis (DVT) is well-documented[2], alongside the association of atrial fibrillation with the RA or RA appendage thrombi[3,4], and the catheter-related RA thrombi. However, spontaneous in-situ RA thrombi aetiology is unclear. Nonetheless, emerging evidence from case reports suggests a correlation between a hypercoagulable and inflammatory state and an in-situ RA thrombus[5,6].
CASE DESCRIPTION
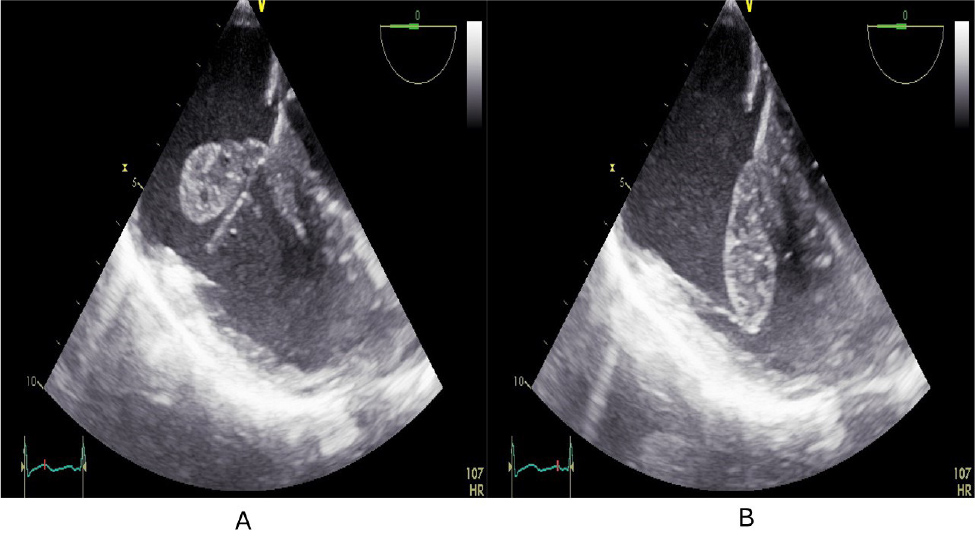
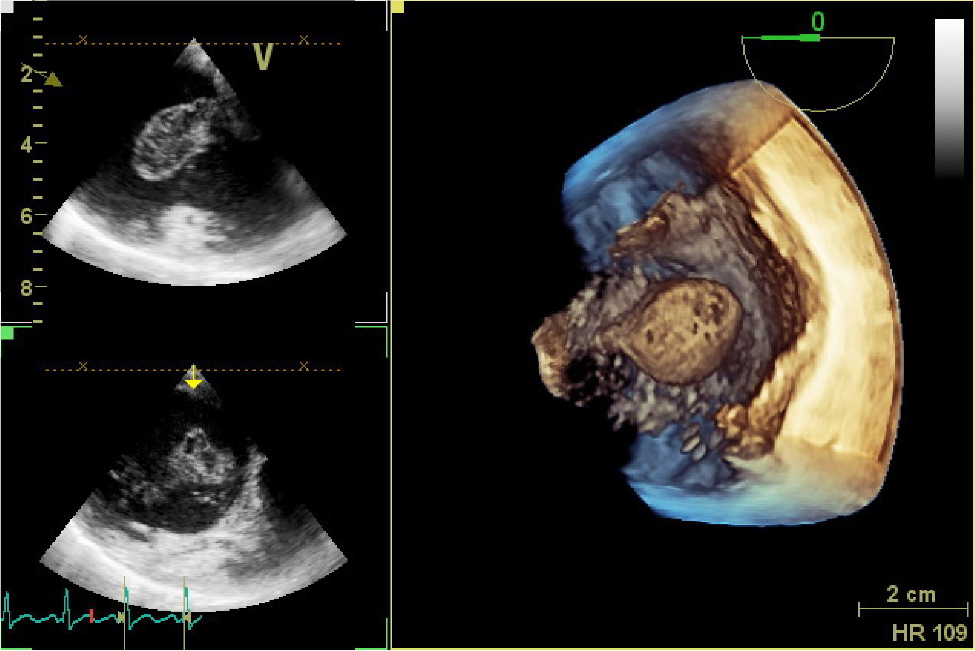
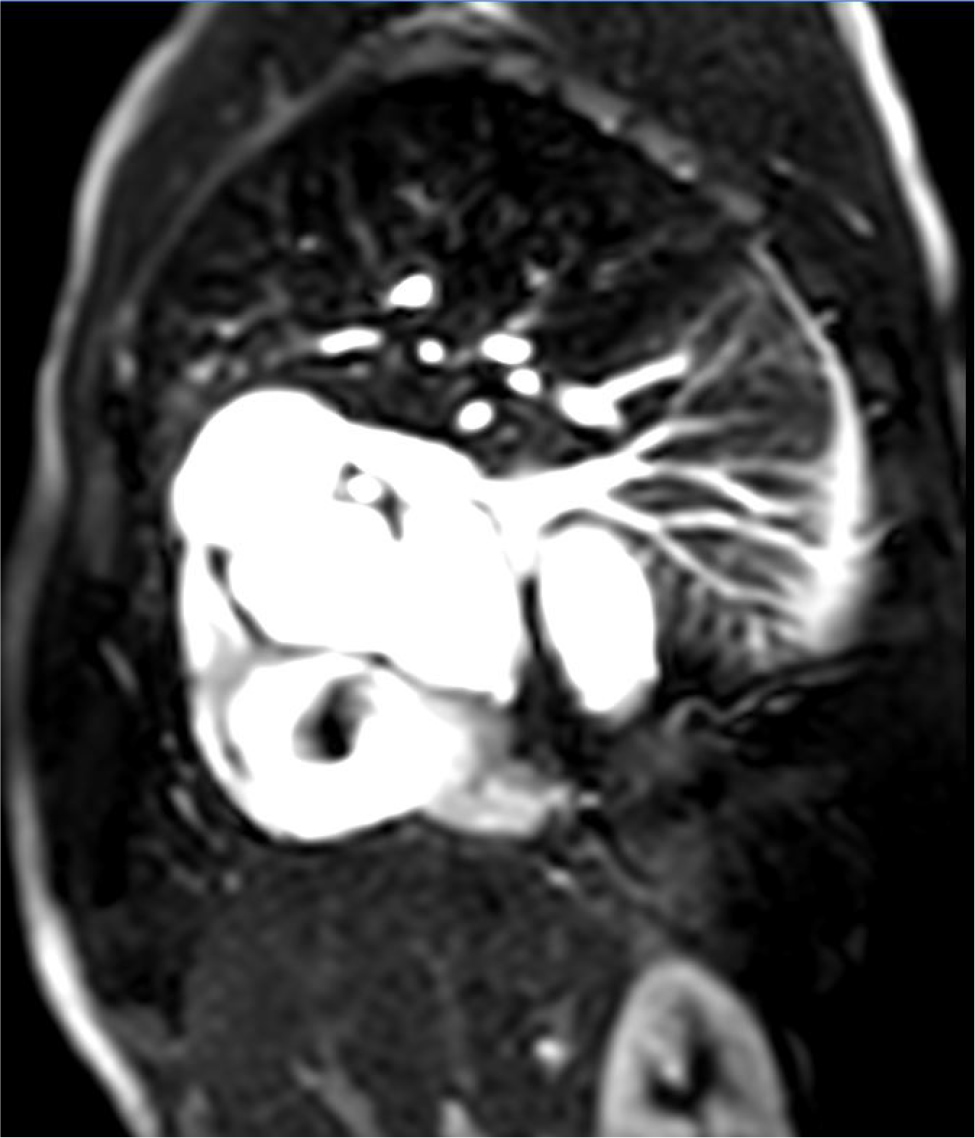
A 41-year-old man with a past medical history including intravenous drug use, HIV, hepatitis C and tobacco use disorder presented with acute, excruciating right hip pain accompanied by swelling, which had started three days prior and hindered his mobility. Arthrocentesis revealed turbid, brown fluid with a white blood cell count of 50,795 (95% neutrophils), and a culture developed a heavy growth of methicillin-resistant S. aureus (MRSA). Initiated on vancomycin, the patient underwent a hip joint washout. Blood cultures upon admission demonstrated MRSA growth, persisting even after four days of vancomycin therapy and joint washout. Initially, findings from a transthoracic echocardiogram (TTE) on admission did not indicate vegetation or masses. However, a subsequent transoesophageal echocardiogram (TEE), performed four days after admission, revealed a sizeable spherical, smoothly contoured and pedunculated mass. This measured up to 2.8 cm with a stalk of 1.3 cm, attached to the septal segment of the tricuspid valve (TV) annulus, extending into the right ventricle during diastole (Fig. 1 and 2). Notably, the TV leaflets were unaffected, and valve function remained unaltered. While the mass’s appearance aligned with myxoma characteristics on TEE, the onset of bacteraemia within days of a TEE and the fact that the mass was not seen on TTE at admission rendered bacterial vegetation more probable. Consequently, CMR imaging was pursued for further characterisation. CMR revealed a 2.5 × 1.8 cm pedunculated mass in the RA, emanating from a 1.1 cm stalk at the atrial aspect of the TV annulus, devoid of early enhancement (Fig. 3) and lack of perfusion (Fig. 4), indicative of thrombus formation. Given the mass’s significant size, transcatheter aspiration was deemed necessary. Subsequently, the patient underwent successful transcatheter mass debulking, with histopathology revealing organising fibrin clots and negative cultures.
Figure 1. A) TEE displaying a spherical mass connected to the septal segment of the tricuspid valve annulus via a stalk; B) The mass protrudes into the right ventricle during diastole.
Figure 4. MRI perfusion image demonstrating the absence of blood flow perfusion in the mass.
DISCUSSION
The detection of RA thrombi is increasing, primarily attributed to the widespread availability of echocardiography and an increased awareness of its association with pulmonary embolism (PE). Classifying RA thrombi involves considering factors such as their mobility, shape and attachment presence[4].
In a study conducted over three decades ago[1], RA thrombi were categorised into three types: highly mobile and worm-like thrombi associated with DVT and PE; immobile attached thrombi, akin to those found on the left side; and less frequent thrombi sharing features of the previous two types, often resembling myxoma. However, data on the latter type are scarce, with reports mostly emerging in cases linked to autoimmune conditions causing heightened inflammatory or a hypercoagulable state[5,6].
In our patient’s case, the mass resembled a large RA myxoma; however, its rapid growth amid bacteraemia favoured bacterial vegetation. For better characterisation, CMR was performed, which strongly suggested a thrombus rather than a solid mass. Consequently, we opted for transcatheter aspiration over high-risk surgery. Despite limited data on the risk of embolisation associated with this type of RA thrombus, given its size and mobility, transcatheter aspiration was deemed the appropriate intervention.
Pathological examination and culture results revealed an organised fibrin thrombus without infection. The thrombus was likely to the high inflammatory state due to sepsis and bacteraemia.
CONCLUSION
RA thrombi can mimic the presentation of myxoma. Utilising CMR aids in distinguishing between these entities, thereby averting unnecessary surgical interventions. Moreover, it is crucial to acknowledge that spontaneously attached RA thrombi can develop in the absence of DVT or atrial fibrillation, particularly in contexts of heightened inflammation and hypercoagulability. Lastly, transcatheter aspiration emerges as a less invasive alternative to surgery, offering a promising avenue for managing such cases effectively.