ABSTRACT
Background: Chylothorax can be classified into traumatic and nontraumatic based on the etiology. Nephrotic syndrome is a very rare cause of nontraumatic chylothorax in adults.
Case presentation: A 66-year-old woman with membranous nephropathy who was non-compliant with her management, presented with dyspnea, and was found to have a large right sided chylothorax. Her chylothorax was secondary to membranous nephropathy after excluding other causes, which has been rarely reported in literature.
Conclusion: This case highlights the possibility of nephrotic syndrome causing chylothorax, especially in patients with undiagnosed nephrotic syndrome or patients non-compliant with their management. When evaluating a patient with chylothorax, providers should consider nephrotic syndrome in the differential diagnosis.
KEYWORDS
Membranous nephropathy, nephrotic syndrome, chylothorax
LEARNING POINTS
- Chylothorax can be secondary to nephrotic syndrome which has been rarely reported in literature.
- Providers should be aware of nephrotic syndrome as a cause of chylothorax especially in patients with undiagnosed nephrotic syndrome or non-compliance with their management.
- Treatment of underlying cause is usually sufficient for spontaneous resolution of chylothorax with or without pleural fluid evacuation.
INTRODUCTION
Nephrotic syndrome typically presents with heavy proteinuria, hypoalbuminemia, edema, hypertension, hyperlipidemia and hypercoagulability. Membranous nephropathy is the most common nephrotic syndrome in adults[1]. Chylothorax refers to the presence of milky fluid composed of fat particles in the pleural space. There are several different etiologies that can cause chylothorax, however, chylothorax associated with nephrotic syndrome has been rarely reported in adults[2]. Herein, we report the case of a 66-year-old woman with primary membranous nephropathy, non-compliant with her management who presented with dyspnea, was found to have a right sided chylothorax.
CASE PRESENTATION
A 66-year-old woman with a past medical history of hypertension was admitted 9 months ago because of a large left renal vein thrombosis; mechanical thrombectomy was done and warfarin was started. Within the same admission, she had complaints of edema of bilateral lower extremities, high blood pressure, hypoproteinemia, hyperlipidemia and proteinuria. Laboratory tests revealed total serum protein 5 g/dl (normal range 6.4 – 8.4 g/dl), albumin level 2.7 g/dl (normal range 3.6 – 5.1 g/dl), 24-hour urine protein 6.7 g/24 hours (normal range 0 – 0.15 g/24 hours), creatinine 0.6 mg/dl (normal range 0.5 – 1 mg/dl), total cholesterol 344 mg/dl (normal range 125 – 200 mg/dl) and triglycerides 180 mg/dl (normal range 0 – 150 mg/dl). A renal biopsy showed membranous nephropathy, anti-phospholipase A2 receptor (anti-PLA2R) antibodies level was elevated 45 RU/ml (reference range <20 RU/ml). Rituximab was prescribed for treatment; however, she declined continuous treatment because of insurance issues.
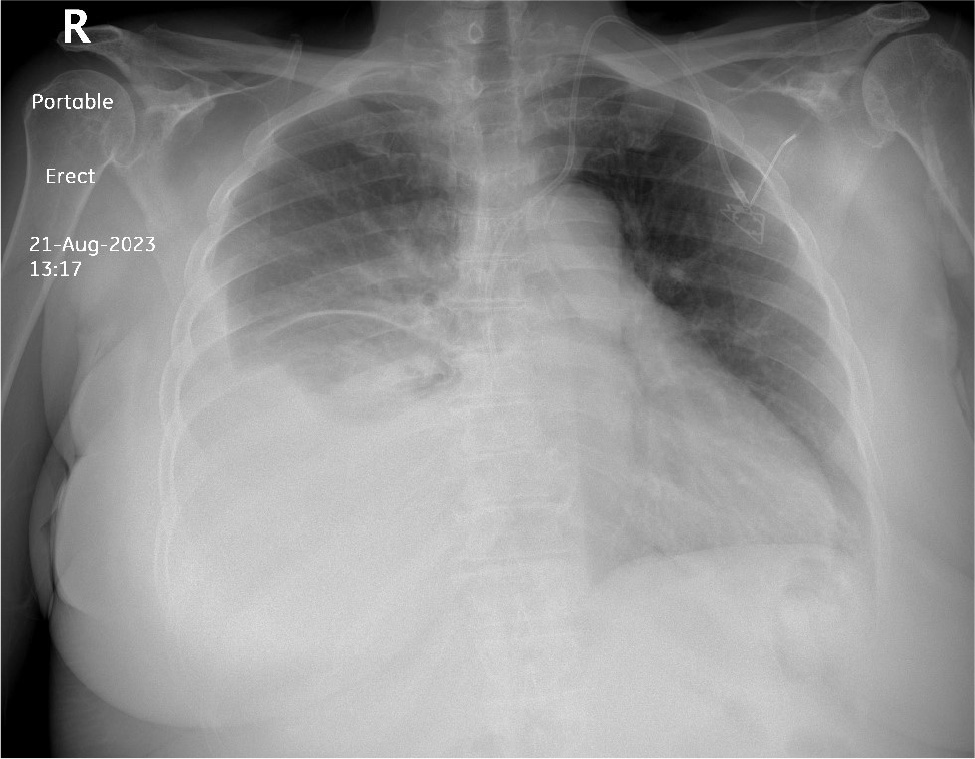
The patient presented recently to the emergency department complaining of shortness of breath and exacerbation of bilateral lower limb edema. On initial evaluation, she was afebrile, tachypneic with respiratory rate of 24 breaths per minute, oxygen saturation (SpO2) of 87% on room air and 94% on 2l O2/min, heart rate of 110 beats per minute and blood pressure of 160/90 mmHg. On physical examination, she was alert and oriented, chest auscultation showed absent air entry on right lung base with dullness to percussion as well as bilateral pitting edema of lower extremities. Chest X-ray revealed a moderate to large right pleural effusion (Fig. 1).
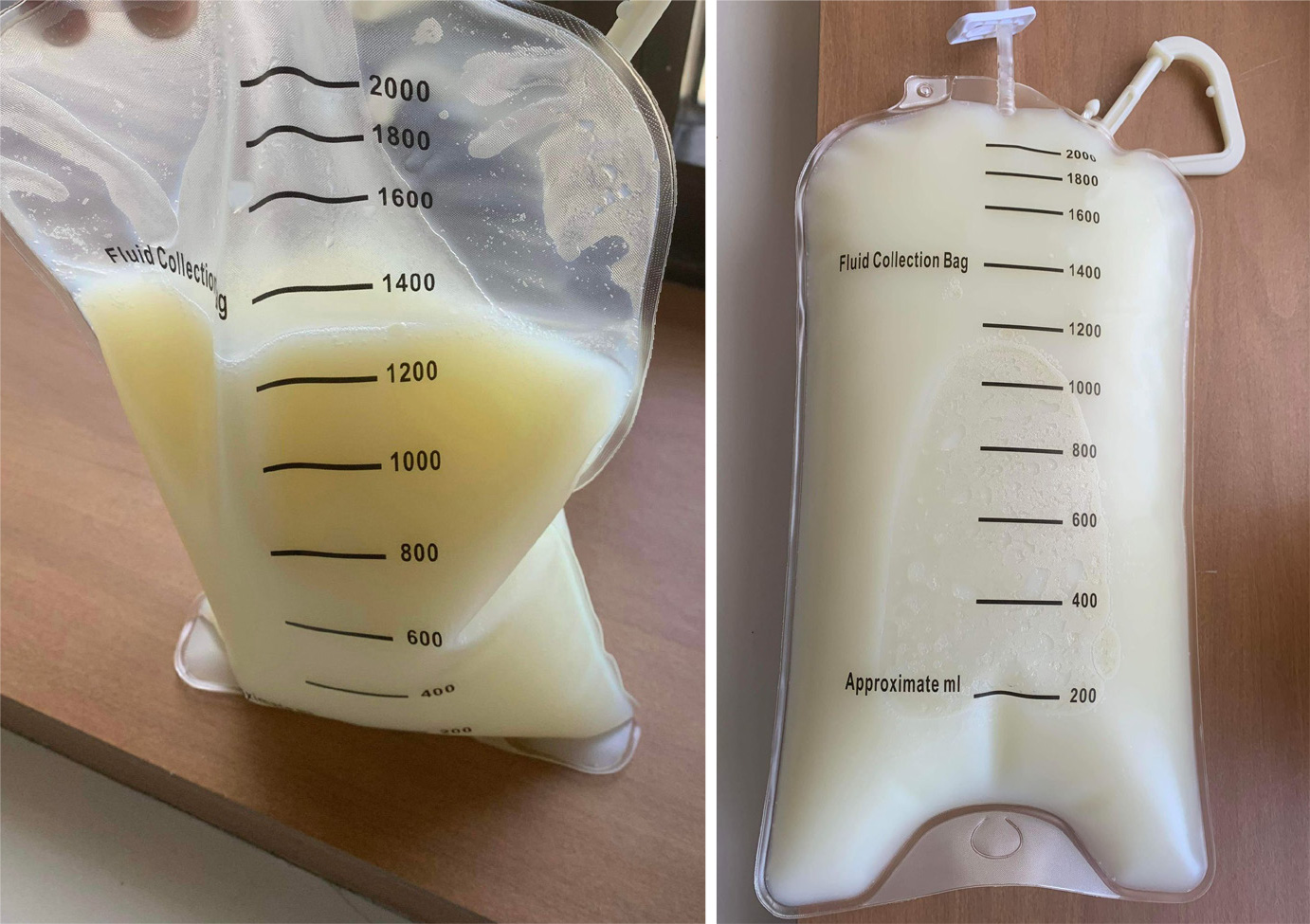
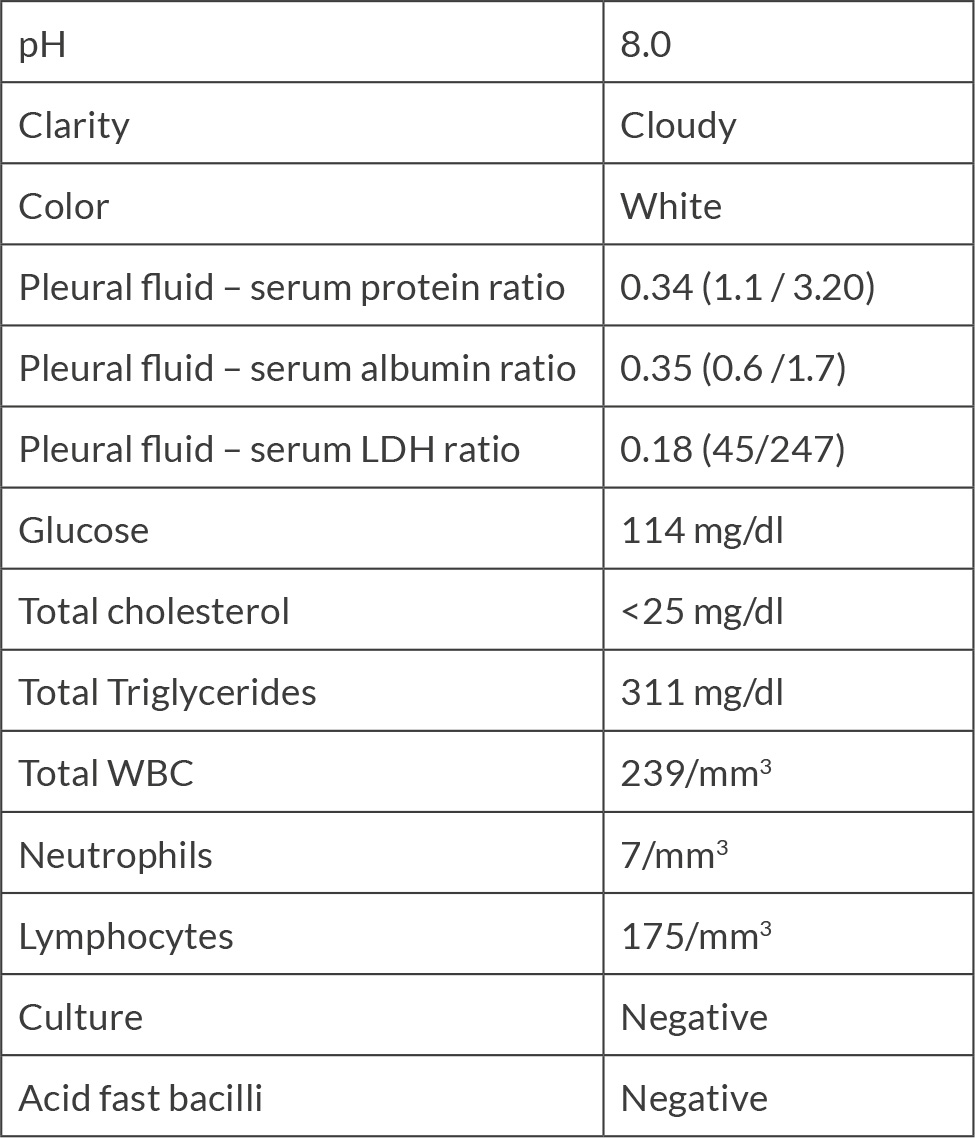
Diagnostic and therapeutic thoracentesis was done with removal of 1300 ml of milky white fluid (Fig. 2). Biochemical analysis of the pleural fluid was consistent with chylous pleural effusion (Table 1). Further examination and analysis ruled out tumors, tuberculosis and other infectious and connective tissue diseases. Based on these findings, a diagnosis of chylothorax secondary to membranous nephropathy was made. The patient was managed by total parenteral nutrition (TPN), octreotide, steroids and rituximab. Under this management for 20 days, she improved significantly and was discharged for outpatient nephrology follow up to continue her membranous nephropathy management.
DISCUSSION
Chylothorax is the presence of chyle in the pleural space, which is composed of triglycerides in the form of chylomicrons and very-low-density lipoproteins, T lymphocytes, proteins, electrolytes, immunoglobulins and fat-soluble vitamins. The thoracic duct carries the chyle from the cisterna chyli and drains into the left subclavian vein. Any disruption or dysfunction of the flow through the thoracic duct can cause chylothorax[3]. There are several etiologies of chylothorax that can be broadly categorized into traumatic and nontraumatic. Malignancy is the most common cause of nontraumatic chylothorax with lymphoma accounting for 37% of the cases, while thoracic surgery is the leading cause of traumatic chylothorax[3].
Chylothorax associated with nephrotic syndrome has been rarely reported in the literature. The mechanism by which nephrotic syndrome can cause chylothorax remains unclear yet could be explained by the following hypothesis. Nephrotic syndrome causes hypercoagulability by loss of antithrombin III through the urine, which may cause thrombosis in the superior vena cava or subclavian vein, impeding the centripetal flow of the chyle from the thoracic duct resulting in chylothorax formation[2]. Hypoalbuminemia associated with nephrotic syndrome can cause bowel edema, which increases the permeability of lymphatic vessels in the intestinal mucosa, leading to the leakage of chyle from the lymphatic and the thoracic duct, resulting in chylothorax and/or chyloascites formation[2].
Analysis of pleural fluid is the best initial diagnostic test for chylothorax, especially the triglyceride and cholesterol levels. Chylous effusion is classically exudative with high lymphocyte count, a low lactate dehydrogenase (LDH), a cholesterol level less than 200 mg/dl and a normal glucose level[3]. Triglyceride level greater than 110 mg/dl and cholesterol level less than 50 mg/dl, is highly suggestive of a chylothorax. If the triglyceride level is less than 50 mg/dl and the patient is on enteral feeding, chylothorax can be ruled out. On the other hand, patients with pleural fluid triglyceride levels between 50 – 110 mg/dl, diagnosis can be confirmed or excluded by lipoprotein analysis. The chylomicrons detection by lipoprotein analysis is the definitive diagnostic test for chylothorax however it is an expensive test[3].
When the diagnosis of chylothorax has been established, additional laboratory tests and imaging studies may need to be performed to determine the cause. Examples of these laboratory tests are liver function tests for patients with suspected cirrhosis and eosinophilic count for patients with suspected filariasis[4]. Most patients should undergo computed tomography (CT) scan of the chest, abdomen and pelvis to assess for mediastinal masses or lymphadenopathy, thoracic duct leak, abdominal accumulation of chyle and thoracic duct and lymphatic abnormalities[5]. More advanced imaging of the lymphatics such as contrast-enhanced or magnetic resonance (MR) lymphangiography is indicated in a smaller proportion of patients such as those in whom the site of chyle leak cannot be determined by CT scan or those with suspected anatomical abnormalities or conduction disorders of the lymphatic system[5].
Treatment of the underlying cause is the mainstay of chylothorax management. However, while addressing the underlying cause, conservative therapy is recommended. These conservative therapies include pleural drainage for symptom relief such as thoracentesis, dietary modification (low-fat diet or TPN) and octreotide injection[4]. In our case, we used all of these conservative therapies while addressing the nephrotic syndrome by diuresis, steroids and rituximab. If the chylous drainage is high-output, meaning more than 1 liter per day or the drainage persists more than 2 weeks despite medical therapy or the patient’s nutritional status deteriorates rapidly during the conservative treatment; surgical therapy is recommended[4].
CONCLUSION
Although chylothorax is very rare, healthcare providers should consider nephrotic syndrome as a cause of chylothorax especially in patients with undiagnosed nephrotic syndrome or patients non-compliant with their management. Understanding the characteristics of pleural fluid analysis in patients with chylothorax can aid in prompt diagnosis and treatment. Once the diagnosis of chylothorax has been established, treatment of underlying cause is usually sufficient for spontaneous resolution of chylothorax with or without pleural fluid evacuation.