ABSTRACT
Introduction: Primary squamous cell carcinoma of the liver (SCC) is a rare and challenging pathology. As an aggressive cancer, the prognosis is extremely poor with less than 12 months overall survival. In view of its low prevalence, we report the case of an elderly patient with primary squamous cell carcinoma of the liver.
Case description: A 74-year-old female, with no pathological history, presented with acute right hypochondrium pain associated with shivering, asthenia and weight loss. We diagnosed primary hepatic squamous cell carcinoma by pathological analysis.
Conclusion: Primary hepatic squamous cell carcinoma represents a rare malignant tumour with extremely poor prognosis. There is no established treatment protocol for this disease and a multidisciplinary approach is needed to choose the best therapeutic option.
KEYWORDS
Squamous, cell carcinoma, liver
LEARNING POINTS
- Primary squamous cell carcinoma of the liver (SCC) is extremely rare, making each case report valuable to the medical community. Documentation and analysis of these cases are crucial to enriching knowledge of this rare disease.
- The absence of established treatment protocols for primary SCC of the liver highlights the need for a multidisciplinary approach to determine the best therapeutic options, which could include innovative treatments and clinical trials.
- The importance of documenting cases like this can help build a knowledge database. This can help identify trends, improve diagnostic and treatment strategies, and potentially lead to standardized treatment protocols.
INTRODUCTION
Primary squamous cell carcinoma of the liver (SCC) is a rare and challenging pathology. It usually results from malignant transformation of squamous cells in organs with squamous epithelium such as the skin, distal oesophagus, lungs, urinary tract, cervix and rectum[1]. Most hepatic SCCs are metastatic in nature from primary sites such as the lung, thyroid or gastrointestinal tract[1]. Pathogenesis remains unclear, but usually this disease is associated with a hepatic cyst, hepatolithiasis or hepatic teratoma[2]. As an aggressive cancer, the prognosis is extremely poor with less than 12 months overall survival[3]. In view of its low prevalence, we report the case of an elderly patient with primary squamous cell carcinoma of the liver.
CASE DESCRIPTION
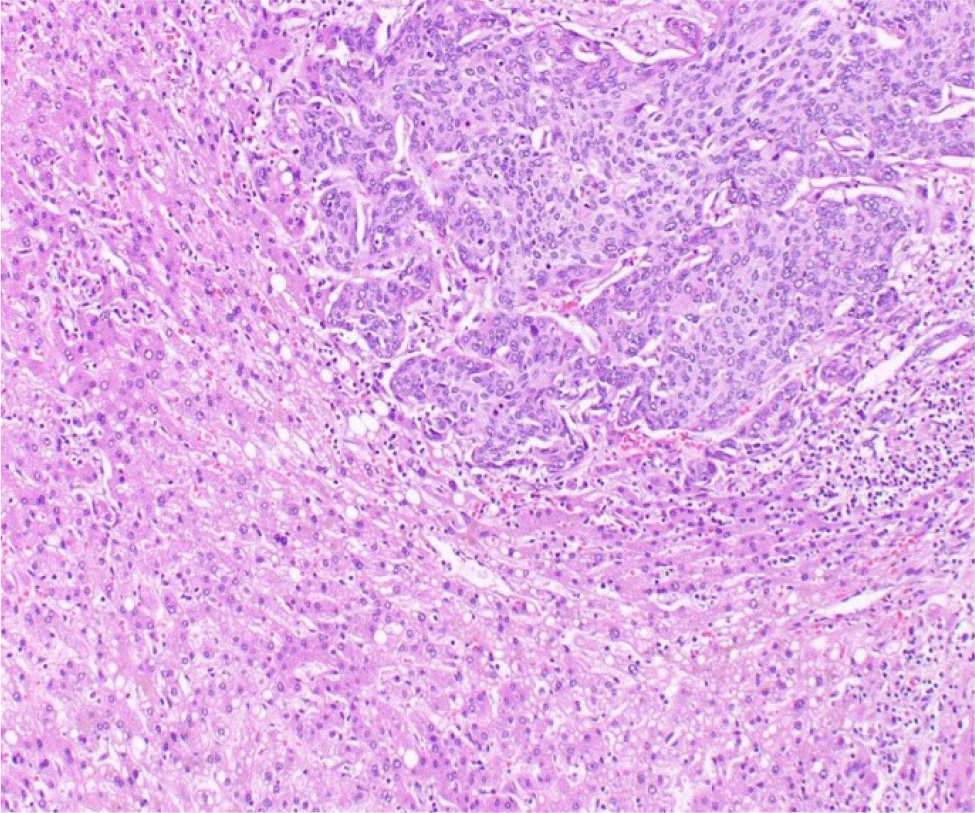
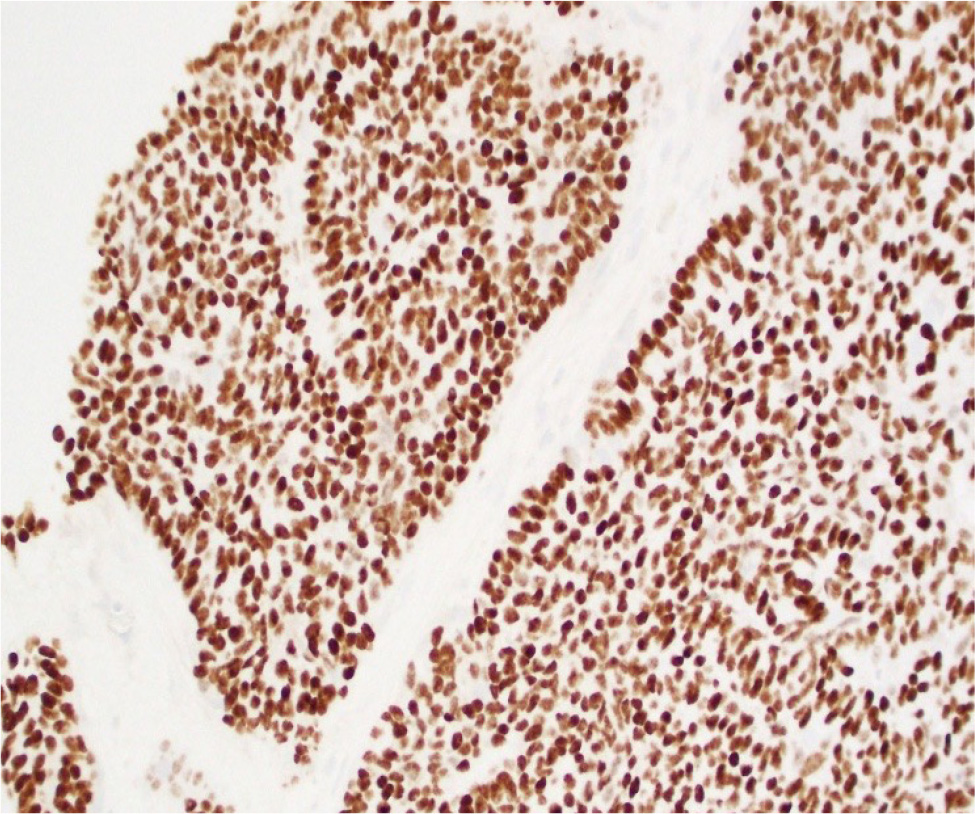
A 74-year-old female, with no pathological history, presented with acute right hypochondrium pain associated with shivering, asthenia and weight loss. Physical examination revealed an altered, febrile patient with right hypochondrial tenderness. Neither the liver nor spleen were palpable, and no cervical, axillary or inguinal lymphadenopathy were found. Blood tests showed normocytic normochromic anaemia at 10.8 g/dl, an elevation of C-reactive protein to 74 mg/l and the tumour marker CA 19-9 to 158 U/ml; an ionogram, liver function tests and renal function were normal. An abdominal CT scan demonstrated peripherally enhanced collections with perihepatic infiltration in segments VI and VII of the liver, suggestive of abscesses, associated with multiple simple biliary cysts. An additional hepatic MRI concluded that the liver abscess was in the pre-suppurative stage, measuring 8 × 5 cm. We initiated a large-spectrum antibiotic therapy (ceftriaxone, metronidazole and gentamicin) and the lesion was brought under control after one week. Morphological imaging by CT and MRI showed regression of contrast and perihepatic infiltration, but an unchanged tissue component. Histopathological analysis of the liver mass showed a low-differentiated carcinomatous process (Fig. 1). Immunohistochemistry suggested the tumour as primary or metastatic squamous cell carcinoma of the liver (Fig. 2).
Based on these findings, other examinations included a positron emission tomography (PET) scan, which demonstrated no pathological metabolic fixations outside the liver tumour, except for a node in the left pulmonary hilum with an inflammatory appearance (Fig. 3). Therefore, the diagnosis of primary squamous cell carcinoma of the liver was confirmed. Considering the patient’s advanced age, general condition, the tumour size and its aggressive nature, the decision was to start palliative chemotherapy. Following severe sepsis, she passed away after two months of follow-up.
DISCUSSION
Primary hepatic squamous cell carcinoma is very rare and has a poor prognosis, with average survival of less than one year[3]. The main risk factors are male gender, hepatic cysts, hepatolithiasis and liver cirrhosis[4]. However, its pathogenesis still remains unclear. Various aetiopathogenic theories have been proposed including chronic inflammation of the bile duct, congenital cysts of the biliary tract or hepatic cysts associated with infection and/or stones. Continued irritation due to chronic inflammation may promote squamous metaplasia and subsequent malignant transformation[5]. Other studies have also reported a possible association with hepatic teratoma[6]. Our patient had no risk factors associated with primary squamous cell carcinoma of liver and notably no liver cirrhosis but had simple biliary cysts. We suggested the possibility of transformation of the cyst epithelium to squamous cell carcinoma. However, the causes of carcinogenesis need to be further investigated.
Clinical presentation of primary hepatic squamous cell carcinoma is non-specific. Commonly, it manifests as pain in the abdominal right upper quadrant and might be associated with jaundice, anorexia and weight loss[7]. In contrast to hepatocellular carcinoma, there is currently no specific serum marker for primary squamous cell carcinoma of the liver[1]. Most patients present with elevated aspartate transferase, alanine transaminase and bilirubin values, which are explained by the chronic inflammation of the bile ducts, the liver cyst and the tumour invasion[8].
In the present study, our patient did not develop jaundice and showed normal liver function tests. Primary SCC is a diagnosis of exclusion, as metastatic SCC remains the most common liver disease. A primary origin such as lung, thyroid, oesophagus, gastrointestinal tract or ENT must be excluded. In our case, other possible sites were eliminated by additional investigations such as PET scans. Regarding imaging, CT is the most useful preoperative examination[8]. Most patients have a low-density mass, and enhanced imaging shows irregular or mild enhancement, or marginal enhancement of the lesion during the arterial phase. The portal and delayed phases were similarly enhanced. Some patients also had intrahepatic bile duct stones, intrahepatic bile duct dilatation and liver cysts[7].
Liver biopsy remains the confirmatory diagnostic test. Immunohistochemically, the strong positive staining for CK14 and CK56 suggests that the cancer cells originated from basal cells of squamous keratinised epithelium. Additionally, the positive expression of CK19 confirms the biliary ontogeny of the neoplastic cells[4].
There is still no clear protocol for the treatment of primary liver SCC unlike other primitive liver tumours, for which clear scientific recommendations exist[9]. Therapeutic options include surgical resection, chemotherapy and radiation therapy. Previous data showed a better prognosis for radical surgery compared with palliative treatment, with a mean survival of 17 months versus 5 months[8]. Systemic or intra-arterial chemotherapy may be useful in patients who are not candidates for surgery[6,7]. In addition, transcatheter arterial chemoembolisation and radiotherapy may be offered as an adjuvant to surgery, or in inoperable patients[8]. Although prognosis is poor overall, patients with bile duct stones appeared to have a better prognosis compared to patients with hepatic cysts[8]. In our case, surgery was not an option given the patient’s advanced age, tumour size and aggressive nature, and she was treated by palliative chemotherapy. As an aggressive cancer, the prognosis for squamous cell carcinoma of the liver is extremely unfavourable with a median overall survival of a few months. However, Kaji et al. described a case of liver SCC that responded remarkably well to intrahepatic arterial chemotherapy with an overall survival of 23 months[5].
CONCLUSION
In summary, primary hepatic squamous cell carcinoma represents a rare malignant tumour with extremely poor prognosis. Clinical presentation is usually non-specific, and no specific serum marker has yet been developed, making diagnosis difficult. There is no established treatment protocol for this disease and a multidisciplinary approach is needed to choose the best therapeutic option.