ABSTRACT
Brevibacillus laterosporus, an endospore-forming, aerobic, Gram-positive bacillus, is not only a potential biocontrol agent against plant pathogens but also a rare cause of human infection. Its pathogenicity in humans, especially in immunocompetent individuals, is still not fully understood. Skin infections caused by B. laterosporus are typically opportunistic, entering the skin through cuts, wounds, or other breaches in the skin’s protective barrier, as in the case presented here.
KEYWORDS
Brevibacillus laterosporus, osteomyelitis, antibiotics, microbiology
LEARNING POINTS
- Skin infections caused by Brevibacillus laterosporus are generally considered opportunistic and more likely to occur in individuals with compromised immune systems or pre-existing skin conditions.
- Brevibacillus laterosporus infections in immunocompetent patients are exceedingly rare, and information about optimal treatment strategies is limited.
INTRODUCTION
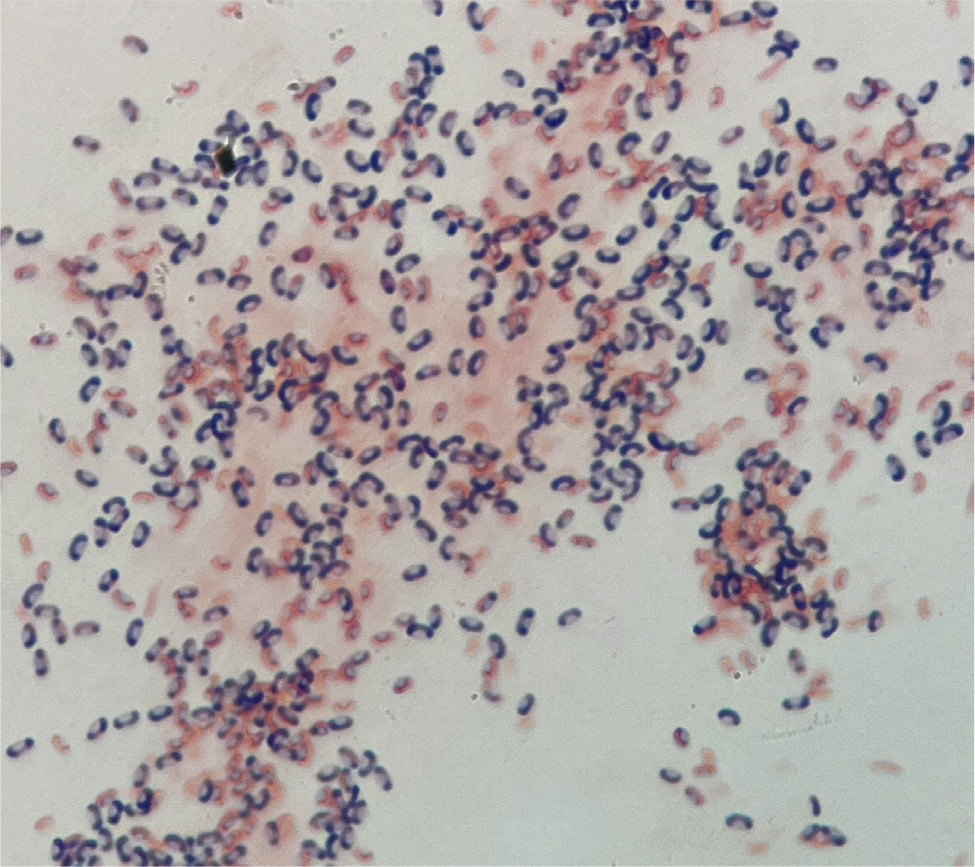
Brevibacillus laterosporus is an endospore-forming, aerobic, Gram-positive bacillus known for its unique “canoe-shaped” body on microscopy. The species was first identified in 1912 and previously belonged to the Bacillus brevis cluster. However, after further research in 1996, it was reclassified as the genus Brevibacillus. This species commonly inhabits soil, freshwater, seawater, insect bodies, leaf surfaces, and fermented foods. The pathogenicity of B. laterosporus is primarily related to invertebrates, including mosquitos, black flies, roundworms, aquatic snails, and flatworm parasites[1]. While insect infections with Brevibacillus are rare, only three cases of Brevibacillus causing localized or systemic infection in humans have been published over the last two decades.
CASE PRESENTATION
A 30-year-old male presented to an orthopedic clinic for a routine post-operative follow-up; three weeks prior, the patient presented to the emergency department (ED) as a level II trauma due to an all-terrain vehicle accident (ATV) at a nearby lake. Imaging in the ED revealed left type II open radius and ulna shaft fractures. He was admitted to the hospital and underwent irrigation and debridement to the bone of the left radius and ulna shaft, as well as open reduction and internal fixation of the left radius and ulna shaft fractures. The patient tolerated the procedure well and was discharged home two days later.
As mentioned above, he followed up with his orthopedic surgeon three weeks later and reported feeling well. He presented as afebrile and hemodynamically stable; however, splint removal revealed an ulnar incision well-healed with sutures in place (Fig. 1). The radial incision measuring 4 cm by 3 cm showed wound dehiscence down to the muscle with visible deep sutures and overlying necrosis (Fig. 2). There was tenderness to the radial aspect of the forearm with no exposed bone. Radial pulses were 2+, with sensation intact throughout the left upper extremity. The remainder of the physical examination was unremarkable, and a complete blood count revealed leukocytosis of 14 K/µl (reference range 4.23-9.07 K/µl) and erythrocyte sedimentation rate of (ESR) of 28 mm/hr (reference range 0-15 mm/hr). All other laboratory testing was within normal limits, and he was redirected to the hospital for surgical intervention.
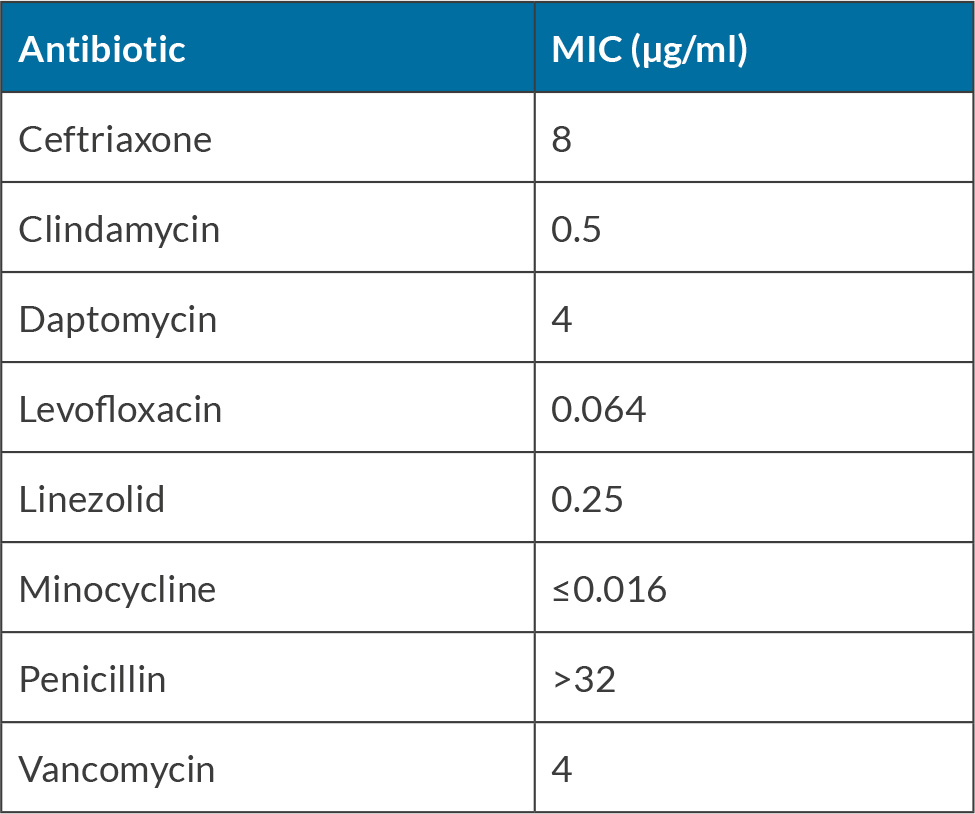
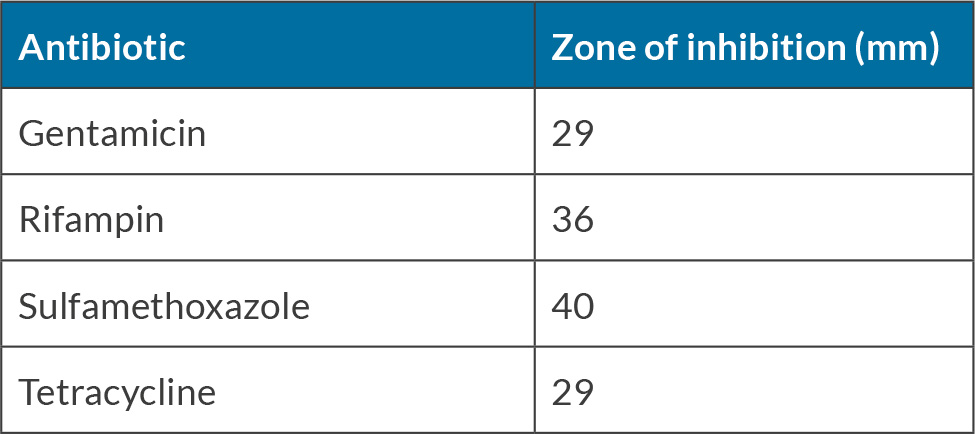
The patient underwent irrigation and debridement of his left forearm. The procedure revealed the wound tracking down to the bone and hardware. Intraoperative wound cultures were obtained, and a wound vacuum device (vac) was placed. Post-operatively, he was empirically started on intravenous (IV) vancomycin 1,750 mg every 12 hours and piperacillin-tazobactam 3.375 g every 8 hours for osteomyelitis and hardware infection. Intraoperative wound culture results (aerobic/anaerobic with Gram staining) were positive for 1+ B. laterosporus (Fig. 3 and 4). Minimum inhibitory concentration (MIC) via Epsilometer testing (E-test) and zones of inhibition via Kirby Bauer methodology were obtained to aid in organism-specific susceptibility to an antibiotic (Tables 1 and 2). The susceptibility results facilitated the de-escalation of antibiotics from vancomycin and piperacillin-tazobactam to a regimen of minocycline 100 mg per os (PO) twice daily and ceftriaxone 2 g every 24 hours via a peripherally inserted central catheter (PICC) for six weeks. After discharge, the patient followed up in the infectious disease clinic. Given that the wound remained open with the wound vac in place, minocycline 100 mg PO twice daily was extended for an additional three months. Since this follow-up, he has successfully had skin grafting, and the wound is healing well.
Table 1. Antibiotic susceptibility via E-test of Brevibacillus laterosporus. Abbreviation: MIC, minimum inhibitory concentration.
DISCUSSION
The first case of infection identified in humans from B. laterosporus was published in 1977 after a young adult had suffered a traumatic injury to the eye, causing endophthalmitis. Despite early therapy with local and systemic gentamicin, there was no improvement, resulting in eye enucleation. Cultures of the vitreous humor, retina, and uvea were collected, and grew B. laterosporus[2]. The second case in 1987 involved a pediatric patient receiving chemotherapy for medulloblastoma through a tunneled central venous catheter found to have B. laterosporus bacteremia that was successfully treated with oxacillin 200 mg/kg/day and gentamicin 7.5 mg/kg/day[3]. The third case in 2020 involved a young adult patient receiving eculizumab for hemolytic uremic syndrome through a tunneled central venous catheter found to have B. laterosporus bacteremia. She was initially treated empirically with IV vancomycin and cefepime before changing to IV gentamicin monotherapy based on the prior case in the literature review[4]. Due to the limited information and successful treatment options, we aim to assist clinicians in determining the most current treatment strategies for infections with B. laterosporus. Choosing the proper antibiotic treatment for B. laterosporus infections is a complex task. The limited occurrence of this pathogen and the absence of clearly defined antibiotic susceptibilities pose a significant challenge. Our microbiology laboratory performed susceptibilities via E-test and Kirby Bauer methodology for several antibiotics, as shown in Figure 3 and 4. Despite the lack of established breakpoints for this organism, our team used the MICs, zones of inhibition, prior case reports, and current guidelines for osteomyelitis to develop an antibiotic regimen, highlighting the professional engagement and problem-solving required in such cases.
CONCLUSION
In conclusion, selecting an antibiotic regimen for B. laterosporus infections was challenging in the absence of clearly defined microbial susceptibilities and breakpoints. This case serves as a testament to our medical team’s collaborative efforts and expertise, providing a valuable guide for clinicians who may encounter similar infections in the future.