ABSTRACT
Anomalous bronchial artery origins may have clinical implications beyond their anatomical curiosity. In this case, identification of such an anomaly led to the diagnosis of chronic thromboembolic pulmonary hypertension (CTEPH).
A 49-year-old male with a history of recurrent deep vein thrombosis (DVT) and pulmonary embolism (PE) on anticoagulation presented with chest pain and shortness of breath. Laboratory analysis was remarkable for a troponin peak of 14.74 ng/ml, a brain natriuretic peptide level of 602 pg/ml and a D-dimer level of 0.62 µg/ml. Electrocardiogram showed non-specific ST elevation in the anterolateral and inferior leads. Computed tomography angiography (CTA) of the chest was positive for PE involving the right lower lobe pulmonary arterial tree. Echocardiogram showed reduced left ventricular function (ejection fraction 38%) and akinesis of the antero-apical and infero-apical segments. Cardiac catheterization revealed non-obstructive coronary arteries, and an anomalous origin of a right bronchial artery from the right coronary artery. The right bronchial hypertrophied as it supplied collateral flow to the occluded right pulmonary artery. This anomaly and the patient’s history of multiple DVT/PEs while on therapeutic levels of warfarin with near normal D-dimer levels raised suspicion for a false positive PE. Pulmonary angiogram revealed chronic occlusion in branches of the right pulmonary artery, mean pulmonary artery pressure of 36 mmHg and no acute thrombus. Ventilation-perfusion scan confirmed the diagnosis of CTEPH. The patient underwent successful pulmonary thromboendarterectomy and subsequently had normalization of mean pulmonary artery pressure.
This case underscores the importance of a comprehensive diagnostic approach, and consideration of alternative explanations for imaging findings, that unveiled the diagnosis of a complex and life-threatening condition such as CTEPH.
KEYWORDS
Anomalous bronchial artery origin, pulmonary embolism, chronic thromboembolic pulmonary hypertension, pulmonary thromboendarterectomy
LEARNING POINTS
- This case underscores the diagnostic significance of identifying anomalous bronchial artery origin which played a crucial role in the diagnosis of the underlying chronic thromboembolic pulmonary hypertension (CTEPH).
- It is important to understand the limitations of computed tomography angiography (CTA) chest for diagnosis of CTEPH.
INTRODUCTION
Bronchial arteries commonly originate from the descending thoracic aorta, however anomalous origins of bronchial arteries have been reported. A bronchial artery originating from a coronary artery is extremely rare. We report a case of anomalous bronchial artery origin from right coronary artery leading to a diagnosis of chronic thromboembolic pulmonary hypertension.
CASE DESCRIPTION
A 49-year-old male came to the emergency department with complaints of chest pain and shortness of breath that started the night prior to presentation. The chest pain was non radiating and increased in intensity with lying down and with deep breaths. He also reported a cough and mild nasal congestion that started a few days prior. Physical examination revealed tachycardia, normal vesicular breath sounds, no jugular venous distention or pedal oedema. The patient’s past medical history was significant for recurrent deep venous thrombosis (DVT) in the lower extremities and pulmonary embolism (PE) in the setting of triple antibody positive anti phospholipid antibody syndrome for which he was on lifelong anticoagulation with warfarin.
The differential diagnosis included non/ST elevation myocardial infarction (N/STEMI), acute PE, pneumonia and viral illnesses.
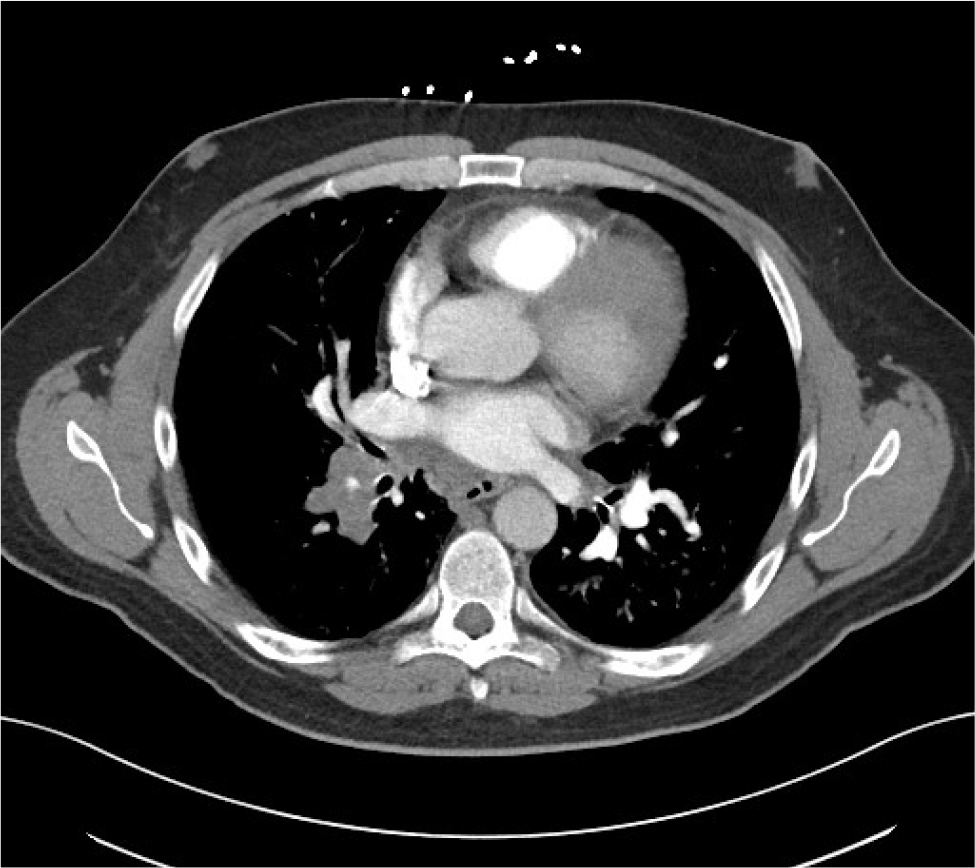
Laboratory analysis showed a troponin level of 5.46 ng/ml, brain natriuretic peptide level of 602 pg/ml, D-dimer level of 0.62 µg/ml, white blood cell count of 11.6 ×103/µl, and an international normalised ratio (INR) of 2.1. A respiratory viral panel was negative. Electrocardiogram revealed non-specific ST elevation in anterolateral and inferior leads without any reciprocal changes. Computed tomography angiography (CTA) of the chest was interpreted as positive for PE nearly completely occluding the segmental and subsegmental branches of the right lower lobe pulmonary arterial tree, with no evidence of right heart strain (Fig. 1).
Figure 1. Computed tomography angiogram of the chest showing occluded right pulmonary artery.
The patient was started on intravenous heparin forPE. Troponin later peaked to 14.74 ng/ml. Echocardiogram revealed newly depressed left ventricular systolic function with ejection fraction of 38% and akinesis of the antero-apical and infero-apical segments with no evidence of shunt on a bubble study.
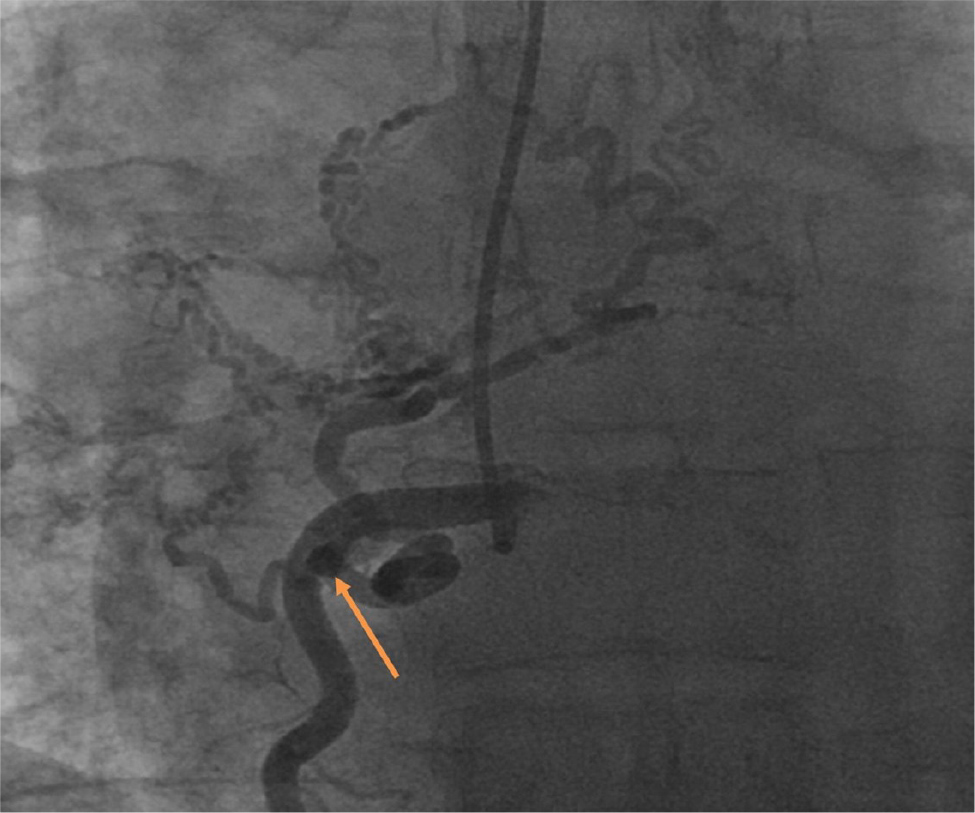
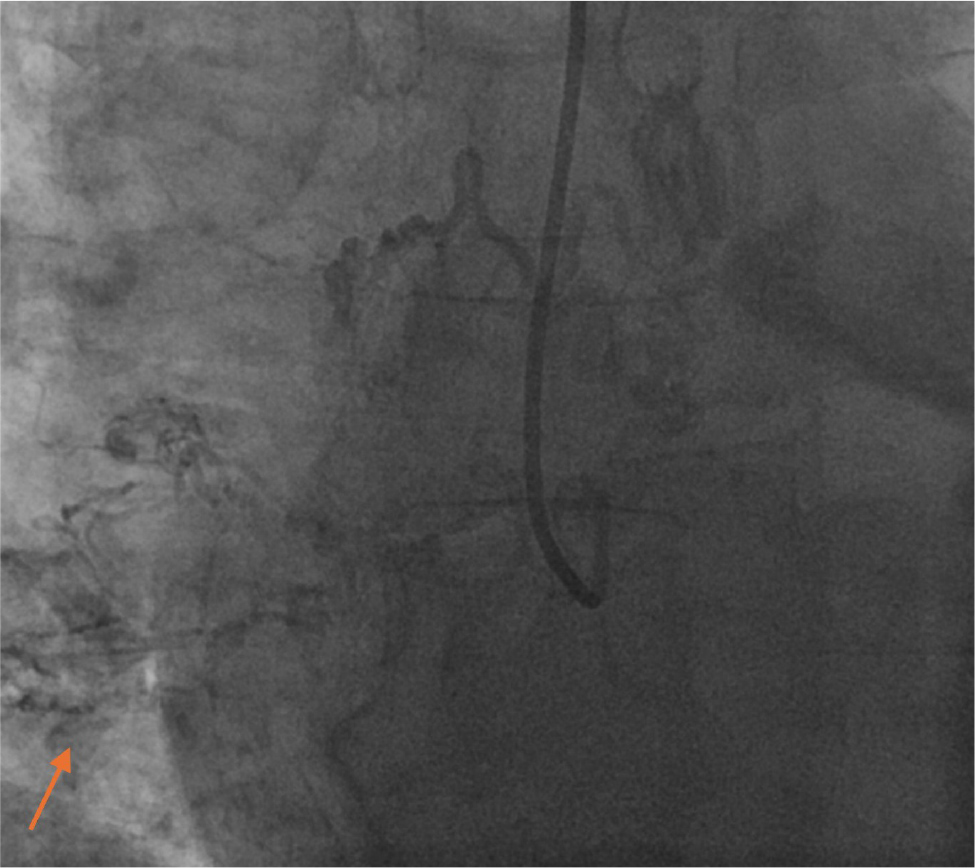
Cardiac catheterization was performed which showed non-obstructive coronary arteries. However, it revealed the anomalous origin of the right bronchial artery, which originated from the ostium of the right coronary artery and was hypertrophied as it supplied collateral flow to the area of the occluded right pulmonary artery (RPA) (Fig. 2). Suspicion for false positive CTA for acute PE was high due to the newly discovered hypertrophied bronchial artery, previous history of multiple DVT/PEs while on therapeutic levels of warfarin and near normal D-dimer levels. A pulmonary angiogram was performed for further characterization and revealed chronic occlusion in branches of the right pulmonary artery, pulmonary hypertension with mean pulmonary artery pressure of 36 mmHg and no evidence of acute thrombus (Fig. 3). A ventilation-perfusion (V/Q) scan was done which confirmed the diagnosis of chronic thromboembolic pulmonary hypertension (CTEPH). The patient was started on guideline directed medical therapy for heart failure with metoprolol succinate, losartan, spironolactone and empagliflozin. Follow-up was arranged for further outpatient management of pulmonary hypertension. The patient was referred to a specialized centre where he underwent successful pulmonary thromboendarterectomy and subsequently had normalization of mean pulmonary artery pressure.
Figure 2. Image from left heart catheterization showing the anomalous origin of the right bronchial artery from right coronary artery.
Figure 3. Pulmonary angiography image showing the right coronary artery flow into the right pulmonary artery.
DISCUSSION
The prevalence of anomalous bronchial arteries has ranged from 8.3 to 35% among patients presenting for bronchial artery embolization for hemoptysis[1,2]. Aberrant bronchial arteries may originate from the aortic arch, internal mammary artery, thyrocervical trunk, subclavian artery, costocervical trunk, brachiocephalic artery, pericardiophrenic artery, inferior phrenic artery or abdominal aorta or rarely coronary arteries[3]. Understanding the normal bronchial artery anatomy and possible anomalies is essential for the diagnosis and differentiation of diseases associated with pulmonary artery obstruction, including chronic inflammatory/infectious processes, chronic thromboembolic disease, or congenital anomalies of the thorax[4]. Here we report the case of an anomalous and hypertrophied bronchial artery origin from the right coronary artery which unveiled the diagnosis of CTEPH. The chronic thromboembolic lesions may have led to microvascular remodelling, abnormal flow pattern and development of bronchial artery collateral supply to the pulmonary circulation. CTEPH is a serious condition characterized by persistent thromboembolic obstruction of the pulmonary arteries, leading to increased pulmonary vascular resistance and, eventually, right heart failure. CTEPH patients with collaterals have a significantly higher incidence of total occlusion of their right or left main pulmonary artery or lobar arteries. These collateral vessels can be analogized to a CTEPH biomarker and could help differentiate CTEPH from idiopathic pulmonary arterial hypertension[5].
Diagnosing CTEPH involves a combination of clinical evaluation, imaging studies, and hemodynamic assessments. Imaging modalities such as CTA chest, pulmonary angiography and V/Q scans are commonly used to identify thromboembolic obstruction in the pulmonary arteries. The management of CTEPH typically involves a multidisciplinary approach, including medical therapy, surgical interventions (such as pulmonary thromboendarterectomy), percutaneous balloon dilation, and, in some cases, lung transplantation. The specific treatment plan will depend on the severity of the condition, the extent of thromboembolic involvement, and the overall health of the patient.
CONCLUSION
Our case is an example of a rare anomaly being used to guide the diagnosis of CTEPH, a potentially devastating but treatable medical condition. It shows the limitations of a CTA chest in the setting of chronic PE.