ABSTRACT
Hepatitis A is a mild self-limiting infection of the liver with spontaneous resolution of symptoms in most cases. However, clinicians should be aware of some commonly encountered complications and extrahepatic manifestations associated with hepatitis A for timely diagnosis and treatment. Rhabdomyolysis, an exceedingly rare complication of hepatitis A, is scarcely documented. We present a case of a 64-year-old man with symptoms consistent with rhabdomyolysis and an evanescent rash secondary to acute hepatitis A. He eventually recovered with conservative management. This case emphasizes the importance of recognizing and treating atypical presentations of acute hepatitis A infection.
KEYWORDS
Hepatitis A, rhabdomyolysis, complications
LEARNING POINTS
- Recognition of atypical presentations: The case underscores the importance of recognizing and treating atypical presentations of acute hepatitis A infection. Clinicians should be vigilant for unusual manifestations of common infections, facilitating timely diagnosis and appropriate management.
- Understanding rare complications: Rhabdomyolysis is identified as an exceedingly rare complication of hepatitis A infection, which is scarcely documented in the literature. This case contributes to the growing understanding of extrahepatic manifestations associated with hepatitis A, emphasizing the importance of considering uncommon complications in the differential diagnosis, especially when typical clinical presentations are observed.
- Management strategies: The article discusses the treatment approach for rhabdomyolysis secondary to acute hepatitis A, which involves aggressive fluid resuscitation to prevent kidney damage from myoglobinuria, correction of electrolyte imbalances, and metabolic abnormalities. Additionally, vaccination against hepatitis A and advocating for sanitation measures are highlighted as important preventive strategies.
INTRODUCTION
Hepatitis A virus (HAV) is a preventable viral infection which is mainly transmitted through the fecal-oral route. It occurs sporadically with an incidence of 1.2 per 100,000 population in the USA[1,2]. Prodromal symptoms include malaise, joint pain, right upper quadrant pain, fever, evanescent rash, loss of appetite, and jaundice[2,3]. In most cases, the prognosis of HAV infection is favourable, typically resolving on its own with a self-limiting disease course. Various complications of HAV infection are fulminant liver failure, acute kidney injury, autoimmune haemolytic anaemia, aplastic anaemia, acute pancreatitis, mononeuritis, reactive arthritis, glomerulonephritis, cryoglobulinemia, Guillain–Barre syndrome, and pleural or pericardial effusion[4]. Rhabdomyolysis is an exceedingly rare complication of HAV infection that is not well documented in the literature[5,6]. The classic clinical manifestations of rhabdomyolysis are myalgia, weakness, and myoglobinuria which presents as tea-coloured urine[7]. This case underscores the importance of recognizing rare complications of HAV infection and contributes to the growing understanding of extrahepatic manifestations associated with HAV infection.
CASE DESCRIPTION
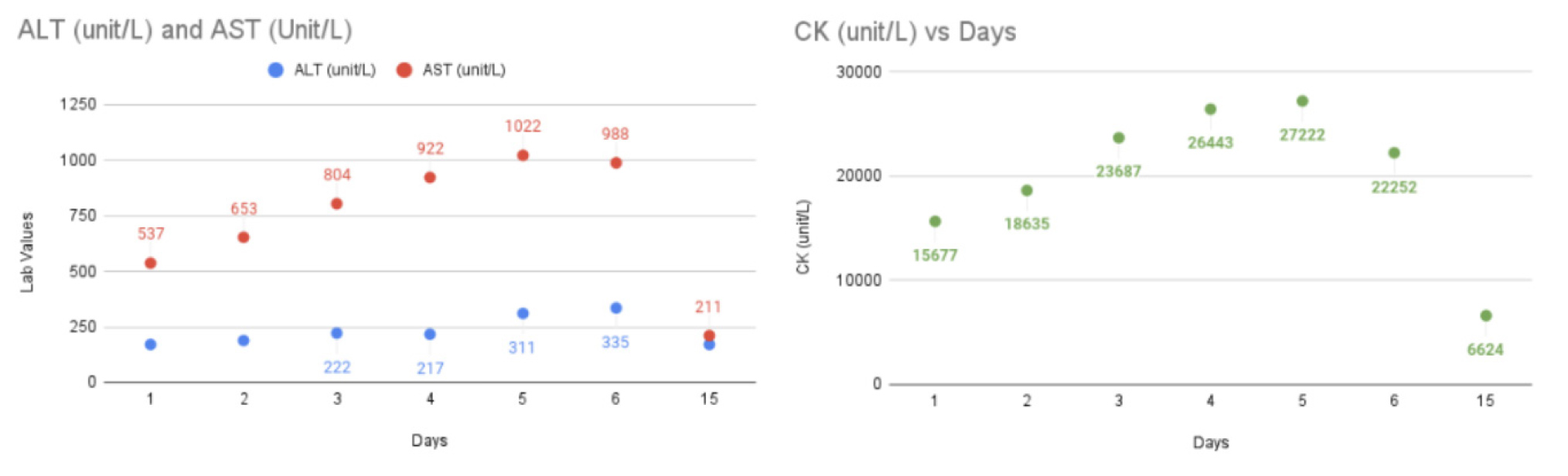
A 64-year-old man with a history of gout maintained on colchicine for acute flare up episodes, initially presented to our facility with complaints of bilateral lower extremity weakness and muscle pain for four days. The patient reported simultaneous onset of non-bloody diarrhoea, erythematous, mildly pruritic rash involving his neck and back, and diffuse progressive ascending myalgias with associated weakness (Fig. 1). The patient otherwise denied any significant medical, family or social history. His vital signs were normal. Laboratory results (aspartate aminotransferase - AST, alanine transaminase - ALT, and creatine kinase) obtained during hospitalization and post discharge follow-up are displayed in Figure 2. His lactate dehydrogenase (LDH, 1174 unit/l) and aldolase (120.5 U/l) levels were also elevated. The bilirubin level was normal. Urinalysis showed 2+ blood without any red blood cells indicative of myoglobinuria. The patient’s hepatitis A IgM antibody was reactive but work up for other infectious, autoimmune and chronic liver disease aetiologies were negative. The patient was treated with aggressive fluid resuscitation without any significant improvement in rhabdomyolysis. His electromyogram was suggestive of a mildly diffuse myopathic process of the left upper and lower extremities, which was consistent with polymyositis. Left quadriceps muscle biopsy showed mild neurogenic changes consistent with nonspecific acute inflammatory myopathy without any evidence of chronic changes. Based on the extensive workup, it was determined that the patient’s presentation was most consistent with rhabdomyolysis as a complication of acute hepatitis A infection. He had significant clinical improvement with near-resolution of his symptoms with conservative management and was discharged after 7 days.
Figure 2. Trend of aspartate transaminase (AST), alanine transaminase (ALT), and creatine kinase (CK) during the hospital stay.
DISCUSSION
This case underscores the rare but significant association between acute non-fulminant hepatitis A infection and the onset of rhabdomyolysis. The pathophysiological association of HAV and rhabdomyolysis remains uncertain but may involve multifaceted mechanisms. These include but are not limited to tissue hypoxia, bacterial infiltration into muscle tissue, diminished activity of oxidative and glycolytic enzymes, triggering of lysosomal enzyme cascades, and involvement of endotoxin mediated pathways[8]. In our case, presentation with bilateral lower extremity weakness, muscle pain, non-bloody diarrhoea, erythematous rash, and pertinent abnormal labs pointed towards rhabdomyolysis as a complication of acute hepatitis A infection[9]. Rhabdomyolysis in the context of acute hepatitis A is an uncommon complication. It is important to note that rhabdomyolysis alone can also lead to elevated liver enzymes; however, the positive hepatitis A IgM along with clinical symptoms consistent with hepatitis A and lack of other typical risk factors for rhabdomyolysis supports the likelihood of rhabdomyolysis as a complication of hepatitis A[10]. Additionally, acute renal failure secondary to rhabdomyolysis can complicate the clinical course, emphasizing the need for prompt recognition and management to prevent severe complications[9].
The treatment approach for rhabdomyolysis secondary to acute hepatitis A involves aggressive fluid resuscitation to prevent kidney damage from myoglobinuria. Correction of electrolyte imbalances and metabolic abnormalities are extremely important. In severe cases dialysis may be imperative, especially in instances involving elevated potassium levels or persistent acidosis[9]. It is also important to promote vaccination against hepatitis A as well as other age recommended vaccinations to decrease the disease burden[2]. Additionally, it is imperative to maintain sanitation by advocating for proper disposal of sewage, availability of safe drinking water, and practicing personal hygiene[2]. Despite the severity of the condition, the timely diagnosis and implementation of early interventions led to a favourable prognosis. The patient exhibited significant clinical resolution following the implementation of conservative management strategies and was discharged after 7 days.
CONCLUSION
This case contributes to the existing literature on the uncommon association between hepatitis A and rhabdomyolysis, emphasizing the need for vigilance in diagnosing and managing atypical presentations of viral infections.