ABSTRACT
Evans syndrome (ES) is a rare autoimmune disorder characterised by autoimmune haemolytic anaemia (AIHA), immune thrombocytopenia and autoimmune neutropenia. The precise pathogenesis of ES remains unclear, but it is believed to involve immune-mediated destruction of erythrocytes and platelets. Thrombotic complications, such as stroke, are critical yet largely unrecognised in ES. Here, we present a case of an 80-year-old male with ES who developed multiple strokes, emphasising the complex management challenges associated with this condition. The patient, known for stage IIB lung adenocarcinoma, presented with right-sided weakness and was diagnosed with a stroke of undetermined aetiology. He was started on warfarin for secondary prevention alongside intravenous immunoglobulin (IVIG) and corticosteroids for ES. Stroke in ES is rarely reported, and the optimal management remains inconclusive due to its rarity. The patient’s management was guided by existing guidelines for stroke prevention and anticoagulation in the setting of antiphospholipid syndrome. While anticoagulants are recommended for venous thromboembolism prophylaxis in AIHA, there are no clear guidelines for stroke prevention in ES. This case underscores the necessity of individualised treatment approaches and highlights the gaps in evidence regarding stroke management in ES. Future research is essential to determine the optimal management of stroke in this complex clinical scenario.
KEYWORDS
Evans syndrome, coagulopathy, stroke of undetermined aetiology, stroke, AIHA
LEARNING POINTS
- Evans syndrome is a rare autoimmune disorder characterised by the coexistence of autoimmune haemolytic anaemia and immune thrombocytopenia, which potentially increase venous and arterial thrombotic risk.
- Managing strokes in Evans syndrome remains challenging due to its rarity and lack of definitive guidelines, necessitating individualised treatment approaches.
- Future prospective studies are warranted to determine the optimal patient population that needs secondary prevention with anticoagulants following a stroke in the context of Evans syndrome.
INTRODUCTION
Evans syndrome (ES) is a rare autoimmune disorder characterised by the coexistence of autoimmune haemolytic anaemia (AIHA), immune thrombocytopenia and rarely, autoimmune neutropenia[1]. ES was first described in 1951 and represents a diagnostic and therapeutic challenge due to its heterogeneous clinical presentations and the risk of complications[2]. The incidence of ES was estimated as 1.8 per million person-years in 2016[3]. While the precise pathogenesis of ES remains unclear, it is thought to be immune-mediated destruction of erythrocytes and platelets[4]. Although ES can occur as a primary condition, it can also be secondary to other autoimmune diseases, infections or lymphoproliferative disorders[1]. The management of ES primarily focuses on immunosuppression to control the autoimmune process, with treatments including corticosteroids, intravenous immunoglobulins, rituximab or splenectomy[5]. Patients with ES are at an increased risk of developing thromboembolic events, including stroke. The incidence of arterial and venous thrombosis alongside ES is reportedly 20%, which adds a layer of complexity to the management[6]. Here, we describe a case of a patient with ES who presented with multiple strokes, a critical yet largely unrecognised thrombotic complication.
CASE DESCRIPTION
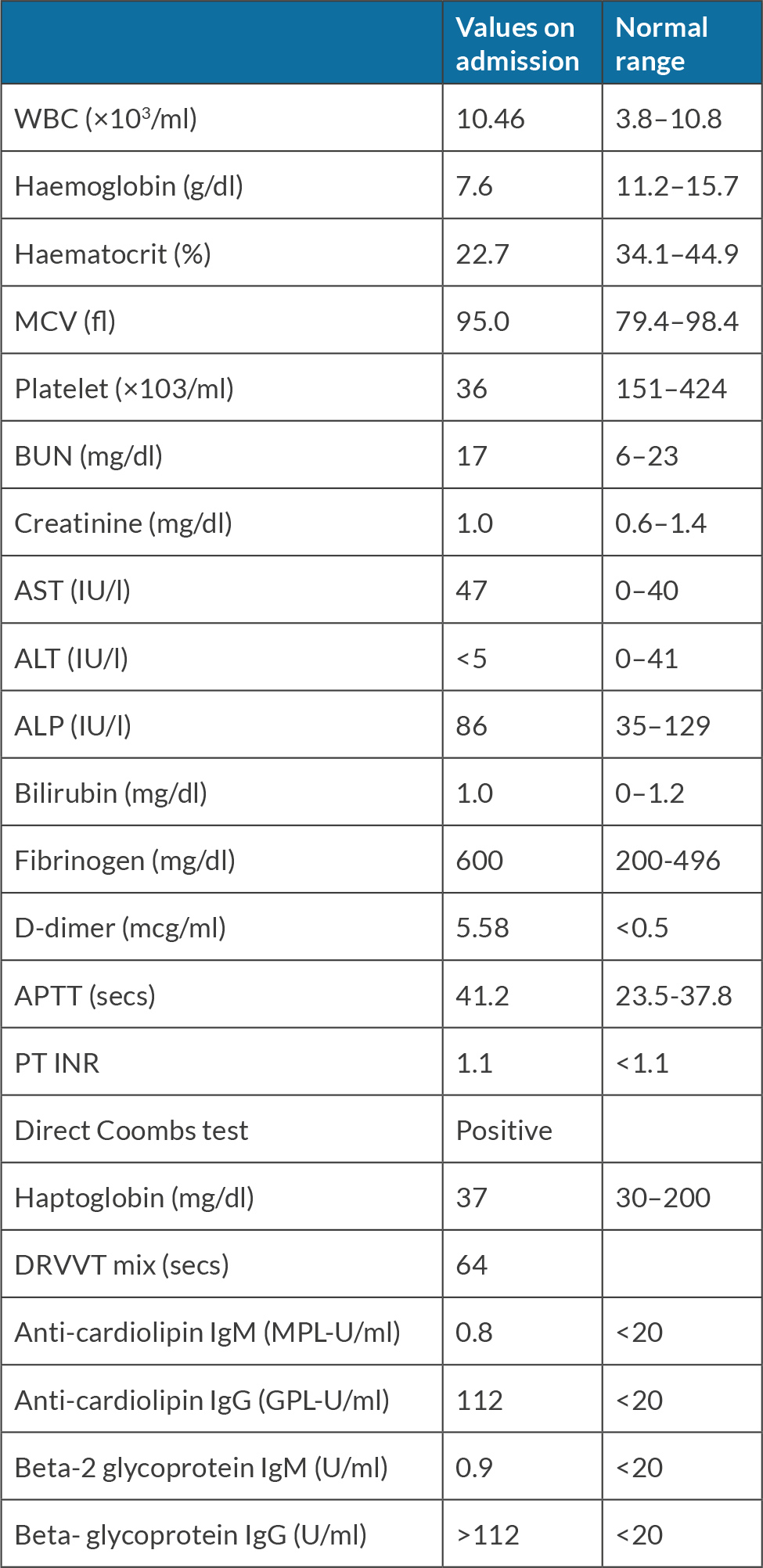
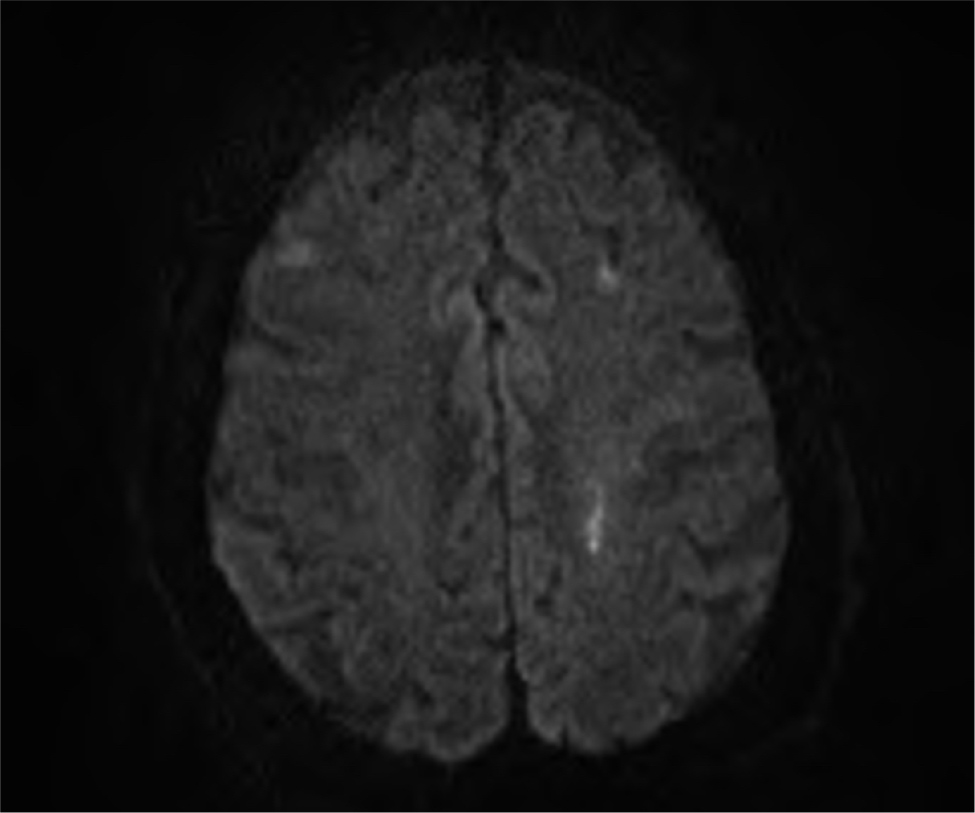
An 80-year-old Chinese male with stage IIB left upper lung adenocarcinoma on chemoradiation presented with right-sided weakness. Seven days before admission, he noticed his right foot dragging on the floor when walking, and a weaker grip on his right hand. He was evaluated at the emergency department with unremarkable initial imaging with head computed tomography without contrast. Two days prior, he had a sudden onset of right eye droop and right flank pain. Four years prior, he was found to be incidentally positive for lupus anticoagulant, cardiolipin IgG and beta-2 glycoprotein without any known thrombotic events. He had been on daily aspirin 81 mg to reduce the risk of arterial thrombosis, which was discontinued seven days prior to the presentation. On admission, he had stable vital signs. On physical examination, he had right eye ptosis and mildly delayed finger-nose-finger testing on the right hand. Aside from 4/5 muscle weakness on the right extremities, the rest of the neurological exam was unremarkable. Table 1 summarises the main laboratory findings on admission. Given a concern for intravascular haemolysis, additional tests were performed. The direct antiglobulin and eluate tests were positive with warm autoantibodies, consistent with ES. Brain magnetic resonance imaging (MRI) showed acute left frontal and centrum semiovale infarcts (Fig. 1). Therefore, the patient was diagnosed with stroke of undetermined cause in light of multiple aetiologies, including ES. After his anaemia and thrombocytopenia gradually improved following administration of intravenous immunoglobulin (IVIG) and high-dose corticosteroid for ES, the decision was made to initiate anticoagulation with warfarin. The duration and dosage were scheduled for adjustment based on the international normalised ratio (INR) and the clinical course. His neurological assessment revealed significant improvement, with a residual neurological deficit characterised by mild hemiparesis of the right upper extremity, and no gait disturbances. He was eventually discharged from the hospital with outpatient follow-up.
Figure 1. Brain MRI showed patchy abnormal diffusion restriction in the left perirolandic parenchyma, with additional small foci of diffusion restriction in the bilateral frontal lobes and right parietal lobe. There was no significant associated mass effect, and there was no acute intracranial haemorrhage.
DISCUSSION
This case describes a patient diagnosed with ES who initially manifested with multiple strokes. The patient was treated with aspirin and warfarin as secondary stroke prevention, alongside glucocorticoid and IVIG for ES. While clinicians tend to focus on bleeding or infection-related complications in ES, thrombosis is a life-threatening complication of ES that may warrant further attention.
Strokes in the setting of ES have rarely been reported in the literature[7-9]. Previous reports highlighted the occurrence of recurrent cerebral infarctions in patients with ES despite treatment with antiplatelet agents and anticoagulants. These findings underscore the increased risk of stroke in patients with ES. In this case, the patient was diagnosed with stroke of undetermined aetiology likely due to multiple contributing factors, including ES, malignancy and antiphospholipid syndrome (APS)[10]. A thorough review of patient history is crucial to identify any modifiable thrombophilic conditions and risk factors.
The definitive management for stroke in the setting of ES remains inconclusive because of its rarity. In this case, thrombolytic therapy was not administered as the patient exceeded the time window for eligibility. Aspirin was initiated for the patient based on guidelines from the American Heart Association (AHA)/the American Stroke Association (ASA), which recommends antiplatelet therapy for patients with ischaemic stroke of unknown source, who are found to have hypercoagulable states. Additionally, warfarin was initiated since the patient has antiphospholipid syndrome based on the European Alliance of Associations for Rheumatology (EULAR) guideline[11]. However, ES is not explicitly listed as one of the hypercoagulable states in the AHA/ASA guidelines, and the current landscape lacks definitive guidelines regarding primary and secondary prophylaxis for arterial thromboembolism secondary to ES. Moreover, the initiation of antiplatelet agents or anticoagulants is occasionally challenging among patients with ES, particularly when complicated by thrombocytopenia, and the underlying hypercoagulable state sometimes needs to be addressed prior to initiating anticoagulation therapy to prevent haemorrhagic complications. In this case, the patient was successfully treated with warfarin after responding to the high-dose glucocorticoid and IVIG therapy, evidenced by the improvement of thrombocytopenia with platelet levels increasing from 29 ×103 /ml to 108 × 103 /ml. Treatment should be tailored on a case-by-case basis, given the inadequate evidence on the management of stroke associated with ES. Future prospective studies are warranted to determine the optimal patient population necessitating secondary prevention with anticoagulants following a stroke in the context of ES.
CONCLUSION
This case illustrates the multifactorial aetiology of stroke, highlighting the intricate interplay between the patient’s comorbidities in ES. The findings underscore the importance of vigilance in stroke risk assessment, individualised treatment approaches and the ongoing need for research to optimise management strategies in complex clinical scenarios.