ABSTRACT
Euglycemic diabetic ketoacidosis (euDKA) is a rare but severe metabolic complication of diabetes mellitus characterised by elevated anion gap metabolic acidosis despite normal or mildly elevated blood glucose levels. Sodium-glucose cotransporter 2 inhibitors (SGLT2i) have emerged as effective antidiabetic medications, yet their use is associated with an increased risk of euDKA, especially when coupled with insulin dose reduction.
We present the case of a 50-year-old male with a 20-year history of diabetes mellitus, initially managed with insulin and metformin, who developed euDKA following the introduction of empagliflozin and sitagliptin alongside a reduction in insulin therapy. Despite normoglycaemia the patient exhibited symptoms of ketoacidosis, including chronic fatigue, polydipsia, and polyuria.
Diagnostic workup revealed metabolic acidosis, elevated inflammatory markers, acute kidney injury and ketonuria. Subsequent specialised laboratory tests confirmed type 1 diabetes mellitus (T1DM) with the presence of anti-glutamic acid decarboxylase (anti-GAD) antibodies and the absence of C-peptide secretion. Management involved fluid therapy, intravenous insulin and glucose administration.
This case underscores the diagnostic challenges of euDKA and emphasises the importance of differentiating between T1DM and T2DM, as management strategies vary significantly. Patient education on insulin therapy and injection techniques is crucial to prevent complications such as improper insulin delivery and dose reduction, which can precipitate euDKA.
In conclusion, clinicians should be vigilant for euDKA in patients on SGLT2 inhibitors, particularly when insulin dose reduction is involved. Comprehensive patient education and accurate differentiation between diabetes types are essential for timely diagnosis and optimal management, thereby reducing the risk of severe complications.
KEYWORDS
Sodium-glucose transporter 2 inhibitors, type 1 diabetes mellitus, euglycemic ketoacidosis
LEARNING POINTS
- The reduction in insulin doses combined with the introduction of an SGLT2 inhibitor in a patient with type 1 diabetes may lead to the development of a dangerous health complication known as euglycemic diabetic ketoacidosis.
- In cases of diagnostic uncertainty regarding the differentiation of diabetes types, measuring the levels of C-peptide and anti-GAD antibodies can be helpful.
- Abnormal glycaemic results in a patient using insulin may result from improper administration. During follow-up visits, it is worthwhile to check the subcutaneous tissue for lipodystrophy and also remind the patient about the necessity of rotating insulin injection sites.
INTRODUCTION
Euglycemic diabetic ketoacidosis (euDKA) is a rare but potentially life-threatening metabolic complication of diabetes mellitus. It is characterised by an elevated anion gap metabolic acidosis in the absence of marked hyperglycaemia. Sodium-glucose cotransporter 2 inhibitors (SGLT2i) have emerged as a promising class of antidiabetic medications. They effectively lower blood glucose levels by promoting urinary glucose excretion[1]. However, the use of SGLT2 inhibitors has been associated with an increased risk of euDKA, particularly in the context of insulin dose reduction or interruption, leading to a relative insulin deficiency.
In recent years, an increasing number of cases have been reported documenting the occurrence of euDKA precipitated by SGLT2 inhibitors, with a notable proportion arising in the setting of additional factors such as reducing the dose of insulin, fasting, illness or drinking alcohol[2,3]. The phenomenon presents a clinical challenge due to the deceptive normoglycaemia observed despite profound metabolic derangement, which can lead to potential delays in diagnosis and management.
This report aims to explore the clinical presentation, diagnostic challenges and management strategies in a patient who developed euDKA following the initiation of an SGLT2 inhibitor concomitant with a reduction in insulin therapy. This report emphasises the need for careful management of patients with diabetes who are on combination therapy.
CASE DESCRIPTION
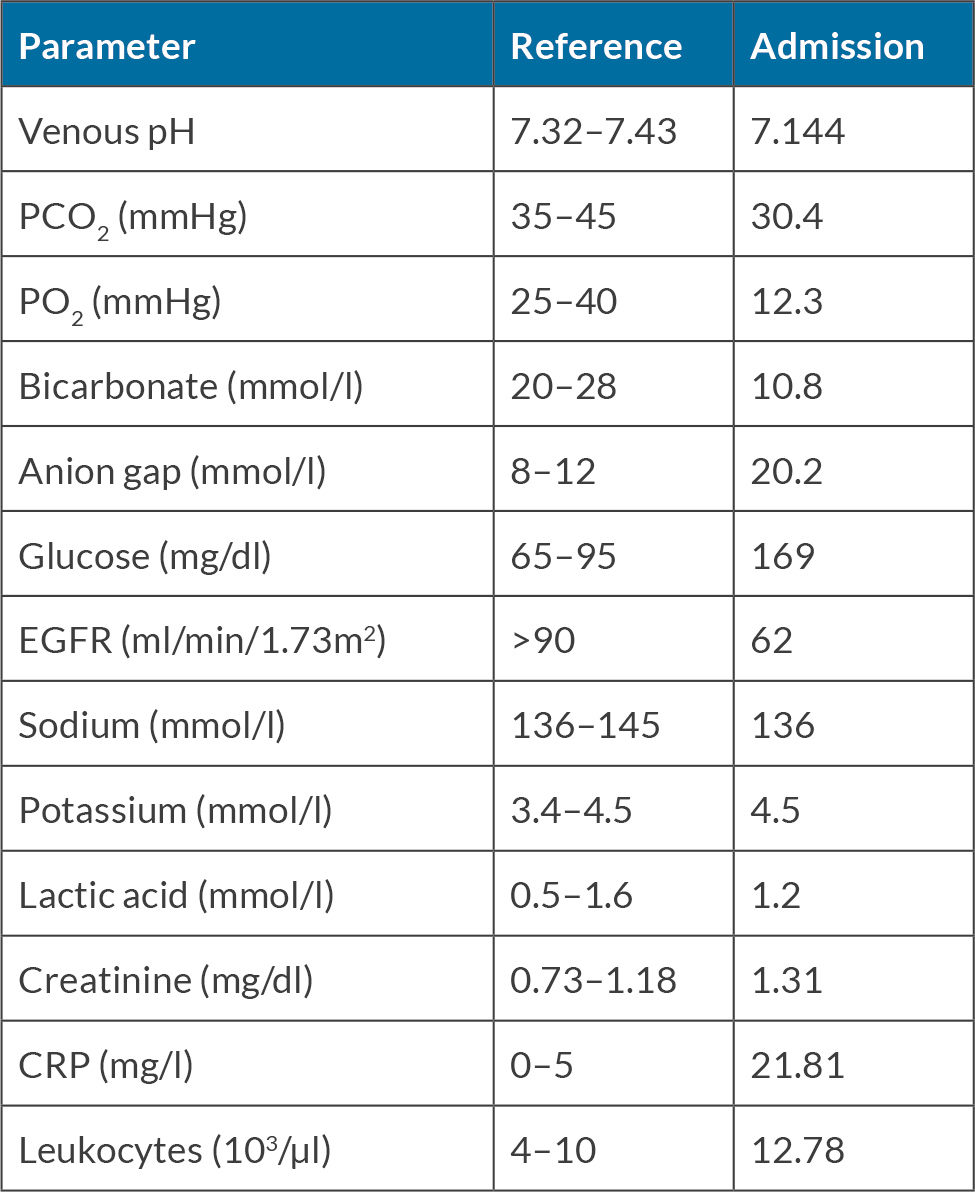
A 50-year-old male presented to the emergency department (ED) with symptoms of chronic fatigue, polydipsia, and polyuria. In his medical history, he had diabetes for 20 years, managed with a combination of insulin mixtures administered twice daily and the maximum dose of metformin, along with hypercholesterolaemia and hypertension. Physical examination revealed no abnormalities. Laboratory tests performed in the ED identified metabolic acidosis, elevated inflammatory markers, acute kidney injury and the presence of ketonuria in the urinalysis. Glucose concentration remained within the normal range (see Table 1). The level of glycated haemoglobin was 9.3%.
The symptoms worsened after the change in treatment – about a month earlier, the patient was hospitalised in a district hospital due to decompensation of diabetes, where the doses of insulin mix (20 units administered twice daily reduced to 14 units once daily) were decreased and empagliflozin and sitagliptin were introduced. During hospitalisation, due to doubts about the type of diabetes (diagnostics in this direction had not been conducted in the patient’s history), C-peptide and anti-GAD antibodies were measured. However, the patient was discharged with new recommendations before receiving the results.
The preliminary diagnosis was an euglycemic diabetic ketoacidosis caused by the use of an SGLT-2 inhibitor with simultaneous reduction in insulin dose. It was therefore decided to admit the patient to the Department of Diabetology and Internal Medicine in Wroclaw on an emergency basis. During hospitalisation, fluid therapy and intravenous infusion of insulin and glucose were administered, which was later changed to intensive insulin therapy with a daily insulin dose of 70 units. The insulin therapy proceeded according to the following regimen: 26 units of insulin glargine administered in the evening, and insulin lispro with the three main meals (16 units for breakfast, 14 units each for lunch and dinner). Attention was paid to educating the patient on proper insulin delivery. Lack of rotation of insulin injection sites was observed – the patient administered the medication into massive adhesions located in the abdomen for about six months. Incorrect insulin delivery combined with an insufficient dosage of the medication could have been the cause of earlier decompensation of diabetes prior to the initiation of SGLT-2 inhibitor.
Specialised laboratory tests were conducted, confirming type 1 diabetes in the patient with the presence of anti-GAD antibodies and a lack of preserved C-peptide secretion. After metabolic stabilisation of the patient and appropriate education regarding insulin therapy, the patient was discharged home.
DISCUSSION
The diagnosis of euDKA is based on several key criteria, including a decreased pH (<7.3) and a serum bicarbonate level less than <18 mEq/l. Despite the presence of ketoacidosis, blood glucose levels are typically within the normal range or only mildly elevated, often ranging from 100 to 250 mg/dl (5.6 to 13.9 mmol/l)[4]. Symptoms of euDKA may include nausea, vomiting, abdominal pain, weakness and altered mental status.
Euglycemic diabetic ketoacidosis (EDKA) is primarily caused by insufficient carbohydrate intake, which leads to reduced serum insulin levels and an excess of counter-regulatory hormones such as glucagon, epinephrine and cortisol. This hormonal imbalance increases lipolysis and the release of free fatty acids, ultimately resulting in ketoacidosis[5].
This case highlights the challenges of diagnosing and managing euDKA caused by SGLT2i, especially when insulin dose reduction is also a factor. The clinical presentation of euDKA, which is characterised by an elevated anion gap metabolic acidosis in the absence of marked hyperglycaemia, presents significant diagnostic difficulties that often lead to delays in appropriate treatment.
Our patient has a 20-year history of diabetes mellitus, which was initially treated with a combination of insulin blends and metformin, followed by the introduction of empagliflozin and sitagliptin. The reduction in insulin dose during a previous hospitalisation, coupled with the initiation of an SGLT2i, likely precipitated the development of euDKA. The patient’s glucose concentration remained within the normal range despite profound metabolic derangement, emphasising the deceptive nature of normoglycaemia in euDKA.
The diagnostic workup revealed metabolic acidosis, elevated inflammatory markers, acute kidney injury and ketonuria, consistent with the diagnosis of euDKA. However, specialised laboratory tests conducted during hospitalisation confirmed the presence of anti-GAD antibodies and absence of preserved C-peptide secretion, indicative of T1DM. This finding emphasises the significance of distinguishing between T1DM and T2DM in patients with euDKA, as management strategies can differ significantly between these two distinct forms of diabetes.
In this case, the management of euDKA focused on fluid therapy, intravenous insulin, and glucose administration. This was followed by intensive insulin therapy to address the underlying insulin deficiency in T1DM. Patient education was also emphasised to optimise treatment adherence and efficacy, specifically regarding proper insulin delivery techniques and rotation of injection sites. The observation of incorrect insulin delivery, inadequate dosing and failure to rotate injection sites underscores the importance of comprehensive patient education and ongoing support in diabetes management.
CONCLUSION
A detailed assessment of the patient’s history and specialised laboratory tests, such as C-peptide level evaluation and anti-GAD antibody presence, are crucial for accurate differentiation between diabetes types. A correct diagnosis enables early initiation of optimal treatment, the omission of which, especially in type 1 diabetes, can have serious consequences. In addition to essential insulin therapy, options for expanding treatment include metformin, GLP-1 analogues or SGLT2 inhibitors. Despite the recommendation by the Polish Diabetes Association allowing the use of SGLT2 inhibitors in type 1 diabetes, caution must be exercised in this regard. Patient education about diabetes management, particularly insulin therapy, is also essential. Simultaneous insulin dose reduction – whether intentional or due to infection or improper administration – can lead to the development of euglycemic diabetic ketoacidosis. Normoglycaemia observed in this condition continues to pose diagnostic challenges and may be associated with treatment delays.