ABSTRACT
Background: Primary hepatic epithelioid hemangioendothelioma (HEHE) is an extremely rare tumour of vascular origin with an incidence of <0.1 cases per 100,000 people worldwide.
Case description: A 29-year-old female with the history of epigastric pain and unintentional weight loss (3 kg over six months) was referred for upper endoscopy. The examination was without visual pathological findings, but a rapid urease test was positive. First-line treatment with clarithromycin-containing triple therapy for Helicobacter pylori infection was given. After completion of eradication therapy, diffuse abdominal pain developed. An abdominal computed tomography (CT) showed multiple liver nodules. Three consecutive core liver biopsies were performed and were inconclusive. A subsequent surgical liver nodule resection was performed. Histopathology of the specimen revealed grade 2 hepatocellular carcinoma; bone scintigraphy was negative for metastasis. A multidisciplinary team (MDT) recommended giving the patient sorafenib, which was poorly tolerated. The histology was reviewed using immunohistochemistry staining at the request of the oncologist, which showed expression of CD31 and CD34. Based on clinical, morphological and immunohistochemistry findings, a diagnosis of hepatic epithelioid hemangioendothelioma was made. Based on the multidisciplinary team's findings, liver transplantation was indicated as the only curative treatment.
Conclusion: Because of the rarity of this disease, combining clinical, radiological and histopathological methods as well as an MDT approach can help to reach the correct final diagnosis. As demonstrated in this clinical case, it is crucial to perform immunohistochemistry of a liver biopsy to confirm a HEHE diagnosis.
KEYWORDS
Hepatic epithelioid hemangioendothelioma, liver biopsy, vascular tumour
LEARNING POINTS
- Hepatic epithelioid hemangioendothelioma is a rare vascular tumour that is often misdiagnosed and mismanaged.
- This case emphasises the critical importance of interdisciplinary teamwork and the use of non-invasive and invasive techniques to achieve a definitive diagnosis.
INTRODUCTION
Epithelioid hemangioendotheliomas (EHEs) are tumours of vascular endothelial origin. They can be seen in the liver, mediastinum, lungs and multiple other sites. EHEs most often occur in the liver[1]. The most common signs and symptoms of hepatic epithelioid hemangioendothelioma (HEHE) are abdominal pain, weight loss or ascites[2], and sometimes patients can be asymptomatic for a long time. HEHE most commonly occurs in the age group between 30 and 50 years and the disease prevalence in females to males is 3:2[3]. A diagnosis is established after radiological and histopathological evaluation.
CASE DESCRIPTION
In May 2021, a 29-year-old woman visited her primary care physician complaining of epigastric pain, heartburn and weight loss (3 kg over six months). The patient had no remarkable previous medical history. During physical examination the skin and sclera were normal in colour. Abdominal examination showed pain in the right hypochondriac region.
The primary care physician recommended an upper endoscopy; the examination was without visual pathological findings, but a rapid urease test was positive. Helicobacter pylori eradication therapy was recommended. First-line clarithromycin-based H. pylori eradication therapy was prescribed for 14 days: clarithromycin 500 mg b.i.d., amoxicillin 1,000 mg b.i.d. and omeprazole 20 mg b.i.d. Shortly after H. pylori eradication therapy, the patient admitted worsening of the abdominal pain.
A full blood count analysis was within normal values. Liver function tests showed slightly increased bilirubin – 25 μmol/l; alanine transaminase, aspartate transferase and alkaline phosphatase were normal. The coagulation tests as well as urine and faecal analysis were normal.
An abdominal (CT) scan revealed a hepatomegaly (CC hepatic right lobe – 15.8 cm; CC hepatic left lobe – 11.2 cm) with multiple hypodense nodules (~20) on both liver lobes without well-defined borders, a density of 21–25 Hounsfield units, size 0.5 cm to 4.2 × 2.5 cm, with almost no contrast uptake. In the porta hepatis separate lymph nodes of non-specific size up to 0.8 cm in cross-section were discovered. Blood vessels were without any pathological changes. Gastrointestinal tumour markers (CA 19-9, CEA, alpha-fetoprotein) were within normal values. A percutaneous liver biopsy was performed three consecutive times due to an inconclusive pathohistology result. Finally, one liver nodule was surgically resected for histological analysis.
Overall description of the surgical specimen: this was a liver tissue fragment 2 × 2 × 2 cm with one white nodule 1.2 cm in diameter. A postoperative histologic examination revealed a grade 2 multicentric hepatocellular carcinoma. Microscopically: liver tissue showed focal hepatocyte damage, lipofuscin deposition, slight fibrosis of portal tracts and slight lymphocytic infiltration. The liver nodule consisted of round and oval-shaped cells, a trabecular, insular, in some places solid structure, moderate cellular polymorphism and moderate stromal desmoplasia. Immunohistochemical staining showed expression of TTF-1, while CA-125, CK19, mammaglobin and glypican-3 were negative. The conclusion indicated the necessity to exclude metastatic thyroid tumour (follicular carcinoma) and lung tumour.
Additional examinations were performed: thyroid ultrasound, colonoscopy, head and lung CT, bone scintigraphy, without any data of distant metastasis or primary oncology.
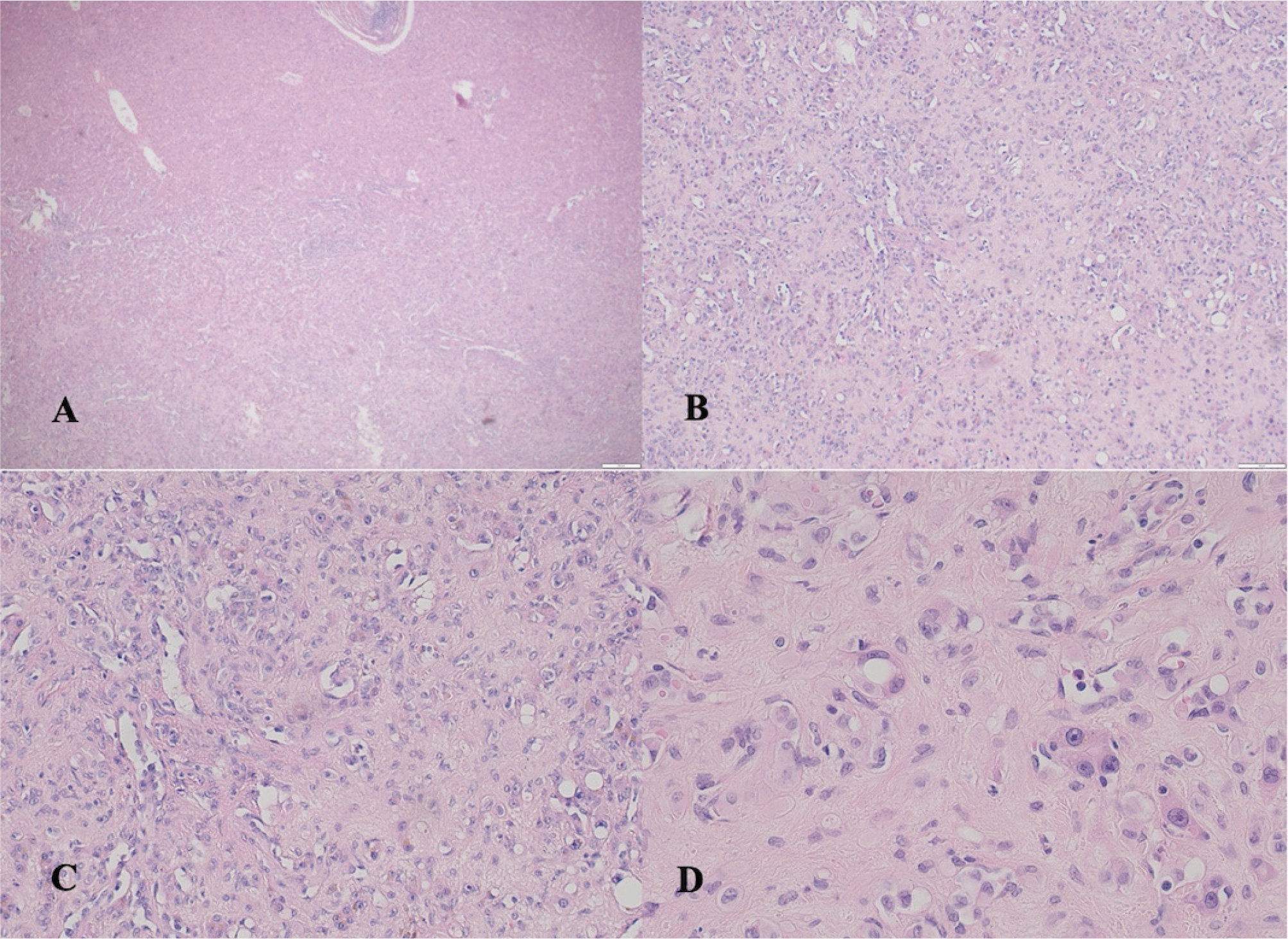
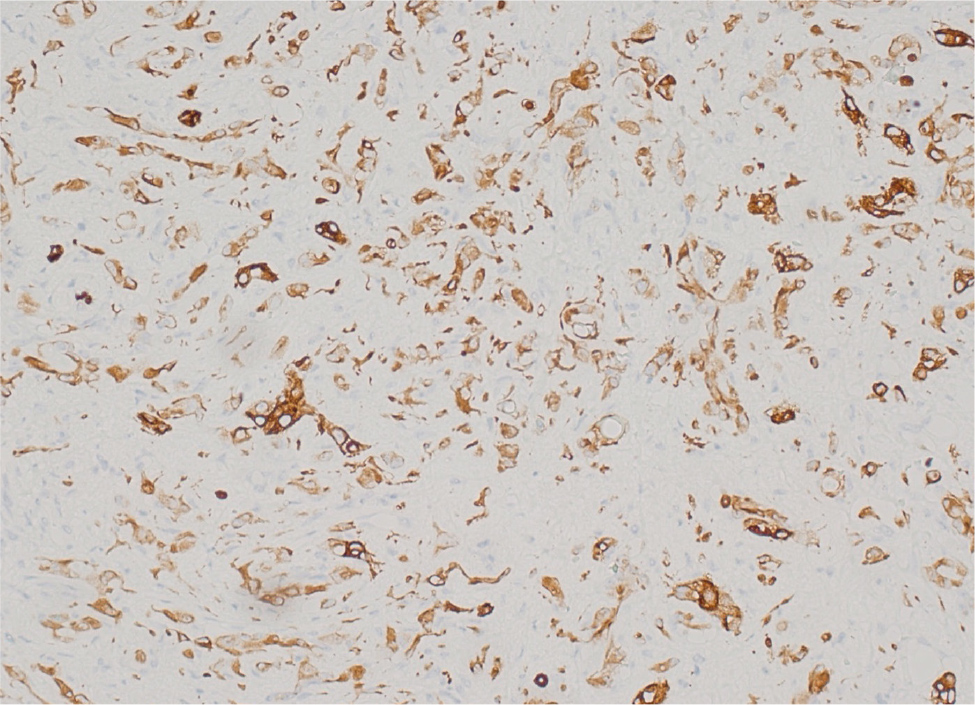
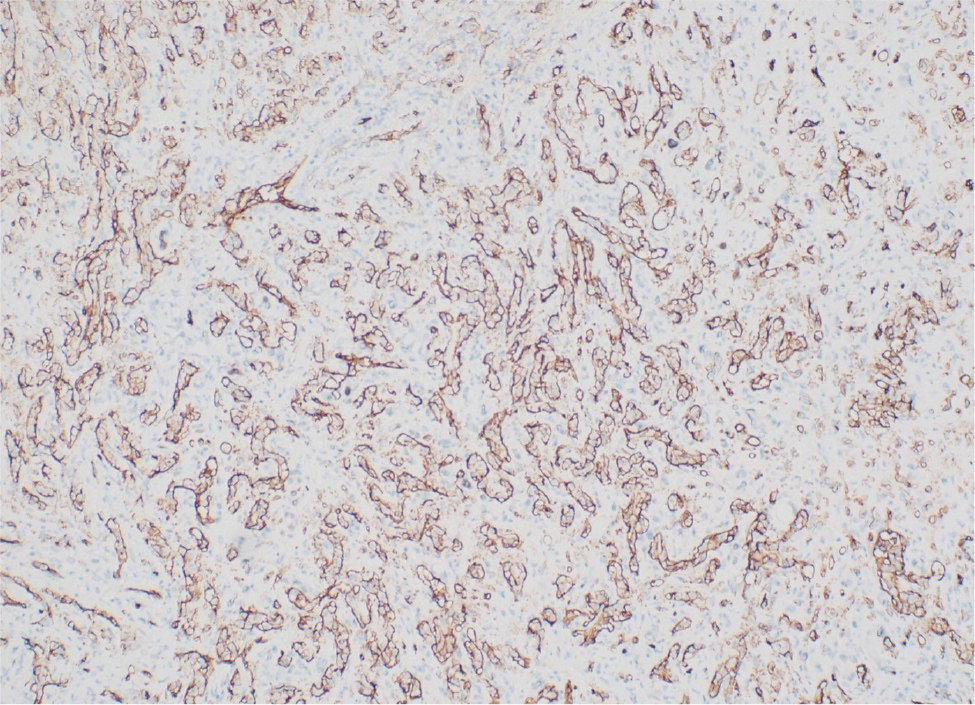
Due to the advanced stage, the MDT referred the patient to palliative treatment with sorafenib, which was poorly tolerated by the patient – malaise, nausea and worsening of abdominal pain deteriorated the patient's condition. The histologic specimen was reviewed by another pathologist at the request of the oncologist, who observed an atypical course of the disease without preexisting liver cirrhosis. Additional immunohistochemical staining was applied. The histologic examination revealed hepatic epithelioid hemangioendothelioma. Microscopically, a liver nodule consisted of elongated spindle-shaped cells, with moderate polymorphism of cells that formed mutually anastomosing structures, some multinucleated cells, stromal hyalinosis, focal necrosis up to 10% and mitotic activity up to 3 mitoses/10 high-power fields (400× magnification). There was perivascular growth, without ingrowth into sinus-type lymphatic vessels which, according to the FNCLCC (Fédération Nationale des Centres de Lutte Contre le Cancer) grading system, represents 4 points. Immunohistochemical analysis showed expression of CD31 and CD34, while TTF1 was equivocal and CA125, mammaglobin and glypican-3 were negative (Fig. 1, 2 and 3).
Figure 1. Representative photomicrographs of hepatic epithelioid haemangioendothelioma. Tumour consisted of cords and nests of epithelioid cells in densely hyalised stroma. Tumour cells have moderate amounts of eosinophilic cytoplasm and round nuclei with some nucleoli. The tumour cell showed moderate cellular atypia. The mitotic index was 3 mitosis/10 high-powered fields. Haematoxylin-eosin staining: A) optical microscope (OM) magnification ×40; B) OM magnification ×100; C) OM magnification ×200; D) OM magnification ×400.
Figure 2. Representative photomicrographs of hepatic epithelioid haemangioendothelioma. Immunohistochemical staining method, CD31 staining. The tumour cells were diffusely and strongly CD31 positive. OM magnification ×200.
Figure 3. Representative photomicrographs of hepatic epithelioid haemangioendothelioma. Immunohistochemical staining method, CD34 staining. The tumour cells were diffusely CD34 positive. OM magnification ×200.
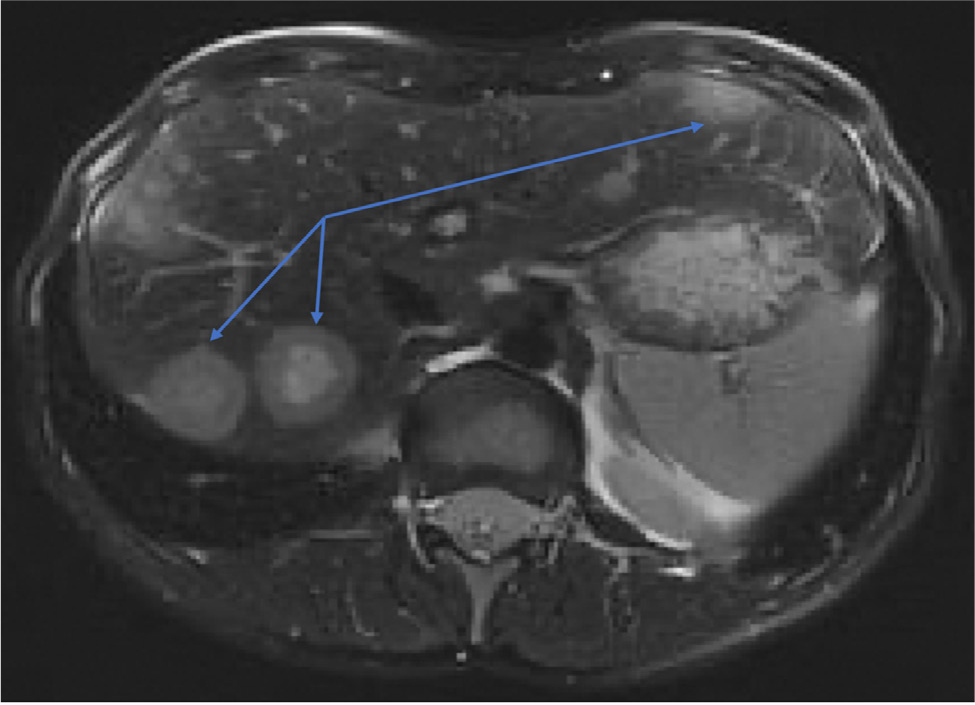
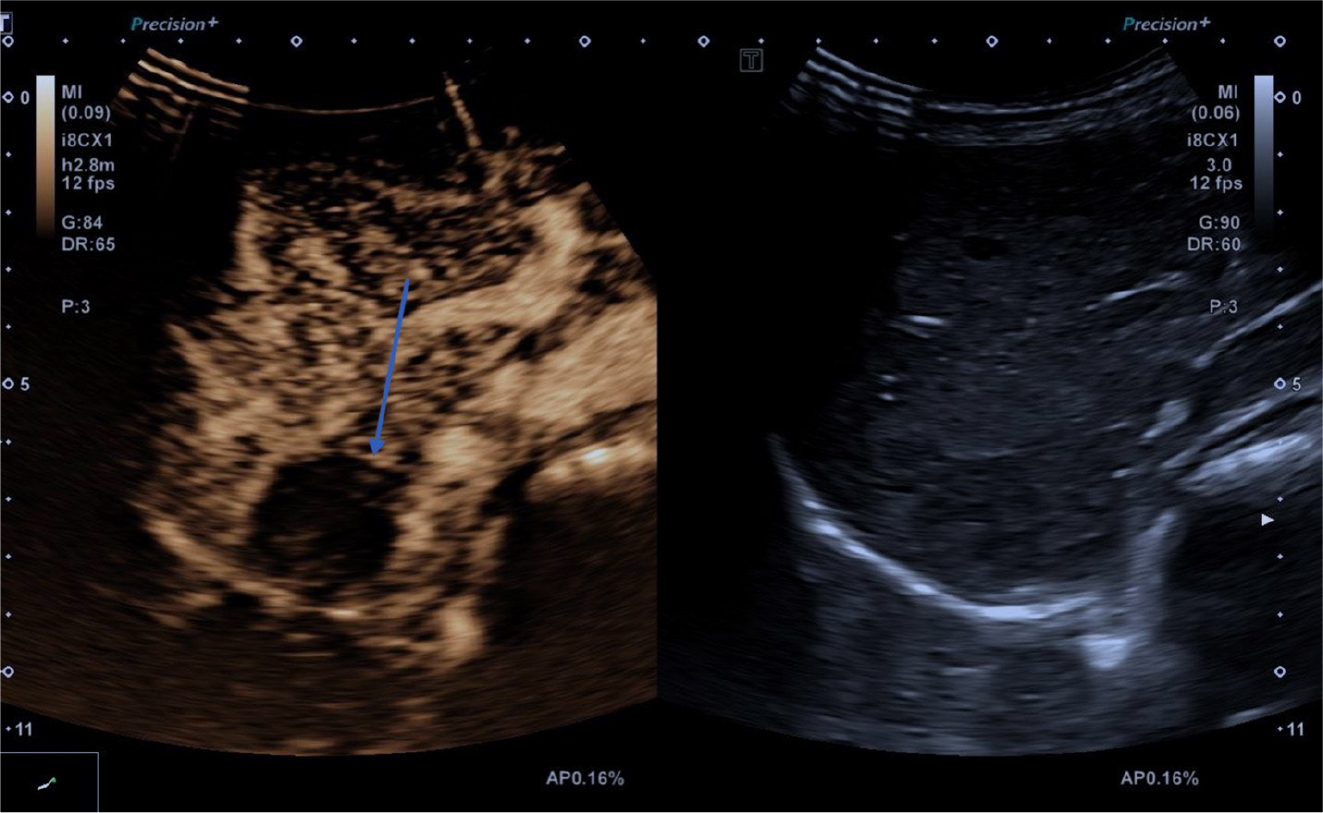
A multidisciplinary liver transplantation team referred the patient for additional examination. An abdominal MRI scan revealed a normal liver size with multiple, smooth contoured nodules, the largest one of 3–4 cm in diameter (Fig. 4) with a poorly vascularised periphery and avascular central part. Enlarged lymph nodes were excluded. The bile ducts were not dilated; however, an abdominal vascular pattern in MR angiography was not evaluated optimally. Contrast-enhanced ultrasound was performed to clarify the diagnosis. Based on this examination, the liver had smooth contours, normal size (12.6 cm) and echogenicity. Diffusely in both lobes, there were many hypoechoic areas of different sizes from 0.5–4.0 cm diameter, slightly inhomogeneous, well-demarcated, with relative hyperechogenicity of the peripheral zone. Blood vessels were without pathological findings. After injection of intravenous contrast media SonoVue® 1.0 ml, the contrast is visible in the liver parenchyma after twelve seconds. The contrast in the parenchyma is homogeneous; the localised formation in the S7 segment collects the contrast material in a peripheral ring-like manner isovascularly, with a markedly hypovascular/avascular central part. Contrast-enhanced liver ultrasound confirmed hepatic epithelioid hemangioendothelioma (Fig. 5). The multidisciplinary liver transplant team members consulted with colleagues in Germany to decide the best curative treatment option for the patient. A liver transplant was recommended as the treatment method to prevent irreversible deterioration of the patient's health in the near future. Currently, the number of liver transplants performed per year in Latvia is insufficient due to the small donor pool suitable for liver transplants. Therefore, a decision was made to perform a live donor liver transplant to save the patient. It is an approved method of liver transplant in cases of chronic or acute liver failure, or liver cancer.
Figure 4. Magnetic resonance imaging shows multiple nodules with a poorly vascularised periphery and an avascular central part.
Figure 5. Contrast-enhanced ultrasound shows liver S7 nodule which accumulates contrast media isovascularly to the liver parenchyma, and with a markedly hypovascular/avascular central part.
DISCUSSION
We report a very rare case of hepatic epithelioid hemangioendothelioma that was initially misdiagnosed as hepatocellular carcinoma and treated with sorafenib. Later repeated histopathological examination confirmed primary hepatic epithelioid hemangioendothelioma. Epithelioid hemangioendothelioma symptoms are based on the primary location of the tumour. For example, hepatic EHE may cause symptoms such as malaise, weight loss with anorexia, nausea, jaundice and abdominal pain. However, patients are frequently asymptomatic until an advanced stage of the disease. We would like to emphasise that this case presents a young female with diffuse abdominal pain and other constitutional symptoms that are often mentioned in the literature with regards to disease. The patient had no preexisting chronic liver disease, which could predispose her to the development of hepatocellular carcinoma. Liver transaminases (alanine transaminase and aspartate transferase) as well as the level of alpha-fetoprotein and carcinoembryonic antigen are not indicators of HEHE because generally they are within the normal ranges[4]. Radiological examinations are important for diagnosing HEHE as some of them have typical features of this disease. For example, ultrasonography shows homogeneously hypoechogenic or centred hyperechogenic nodules with a peripheral hypoechogenic structure. For MRI and CT there is a typical ‘halo sign', which is the result of central coagulative necrosis and a ‘capsular retraction' sign caused by an intense fibroproliferation. The ‘lollipop sign' characterises hepatic/portal vein termination on the edge of the HEHE nodule. Some specialists recommend FDG PET/CT for diagnosing and staging of HEHE[5]. Macroscopic and microscopic examination with immunohistochemistry staining of liver nodules are crucial for correct HEHE diagnosis. Macroscopically, HEHE tumour nodules can be white, yellow and brown, with unclear boundaries. The size of the tumour nodule is variable and can reach up to 21 cm in diameter. On palpation, the nodules may feel firm or rubbery if calcification is present, and the surface may have a rough texture. Microscopically, EHE consists of atypical epithelioid endothelial cells arranged in strands in a hyalinised, myxoid and/or myxochondroid stroma. The cells expose vacuoles in the eosinophilic cytoplasm. Tumours broaden vessel walls, propagate into surrounding tissues and may sometimes obstruct vessel walls and/or cause thrombosis. Nuclear atypia and mitotic figures may present but are not conspicuous. Immunohistochemical analysis of tumour cells show expression of vascular markers such as CD31, CD34, ERG and von Willebrand factor[4,6,7]. Treatment options for HEHE depend on tumour localisation and spread. For example, surgical treatment such as a partial resection of the liver or a total hepatectomy with liver transplant is the gold standard for HEHE. Partial hepatectomy is performed for resectable HEHE, and many studies have reported survival benefits after partial hepatectomy. For unresectable HEHE (for example, multifocal disease, diffuse hepatic involvement or the HEHE is located close to vital structures) liver transplant is indicated. With this approach, long-term results are excellent, with 10-year survival rates of approximately 74%[5,8,9]. Other treatment options for HEHE are tumour embolisation, chemotherapy, hormone therapy and radiation therapy. Various chemotherapeutic drugs including doxorubicin, fluorouracil (5FU), vincristine, thalidomide, interferon-α, and monoclonal antibodies against vascular endothelial growth factor have been used for the treatment of HEHE. According to data, adjuvant chemotherapy may be an effective therapy to prevent recurrence after partial liver resection. Radiation therapy can be used for patients who are unfit for surgery and chemotherapy[5,7,10].
CONCLUSION
Due to the rarity of HEHE, correct diagnosis is challenging as the disease is commonly asymptomatic. Radiological and histological examinations are important for a definitive diagnosis. It is important to apply immunohistochemistry staining of a specimen to confirm the diagnosis. Surgical treatment options of HEHE show excellent long-term results and benefits in survival rates.