ABSTRACT
Inappropriate therapy is a frequent adverse consequence of implantable cardioverter-defibrillator. Inappropriate therapy often occurs due to the misinterpretation of sinus tachycardia or atrial fibrillation/flutter with rapid atrioventricular conduction by the device. Current implantable cardioverter-defibrillator (ICD) mechanisms integrate various discriminators into algorithms to differentiate supraventricular tachycardia (SVT) from ventricular tachycardia (VT), to prevent such occurrences. A 40-year-old man suffered seizures and cardiac arrest abruptly, without prior complaints of chest pain. Without delay, he initiated cardiopulmonary resuscitation (CPR), resulting in the regaining of spontaneous circulation. The patient had previously received a single-chamber ICD due to recurring VT and a prior episode of cardiac arrest. The patient had a medical background of coronary artery disease with complete revascularisation and no previous occurrence of SVT. Interrogating the ICD revealed captured non-sustained ventricular tachycardia (NSVT) and SVT events but no VT episode or shock therapy. During the specified time period, the patient underwent an electrophysiological study, and no SVT was induced with the normal function of the atrioventricular and sinoatrial nodes. Various causes can lead to errors in morphology discrimination criteria in single-chamber ICDs. Extending the detection interval is highly recommended to avoid misclassification of ICDs.
KEYWORDS
Morphology discrimination, supraventricular tachycardia, ventricular tachycardia, ICD misclassification
LEARNING POINTS
- This highlights the crucial significance of precise classification of supraventricular tachycardia (SVT) and ventricular tachycardia (VT) using a single-chamber implantable cardioverter-defibrillator (ICD) discriminator to guarantee prompt and appropriate therapy delivery.
- The morphology criterion used in single-chamber ICDs may have potential limits and inaccuracies, which might result in the misdiagnosis of VT as SVT.
- Further study and enhancement of differentiation algorithms, paired with precise programming and prolonged detection durations are essential to reduce such misclassifications and improve patient outcomes.
INTRODUCTION
Ventricular tachycardia (VT) is a leading cause of sudden cardiac death and a potentially life-threatening cardiac arrhythmia. Intracardial devices (ICDs) are crucial therapy for ventricular tachyarrhythmias (VT or ventricular fibrillation, VF) and to reduce the risk of sudden cardiac death[1]. Inappropriate shock transmission or undelivered shock have been linked to a considerable increase in morbidity and even worse, fatal outcomes in patients with ICDs[2]. The most common cause of inappropriate ICD therapy is inaccurate interpretation by the device of sinus tachycardia or atrial fibrillation/flutter with rapid atrioventricular conduction. To prevent this, a few methods for identification have been developed by device manufacturers to distinguish supraventricular tachycardia (SVT) from VT. All methods, including dual- or single-chamber ICDs, are integrated into algorithms with the intention of achieving a balance between specificity (prevention of improper therapy) and sensitivity (detection of potentially life-threatening VT or VF)[3]. In the context of ICDs, the algorithms place emphasis on the electrogram morphology and attributes associated with frequency-related tachycardia[4].
Despite over 30 years of technological advancement, an ideal discrimination algorithm remains elusive, and the device continues to handle a significant number of episodes improperly[3]. This case illustrated a condition in which the single-chamber discriminator ICD misclassified SVT, resulting in the patient suffering seizures and cardiac arrest in the absence of shock therapy delivery.
CASE DESCRIPTION
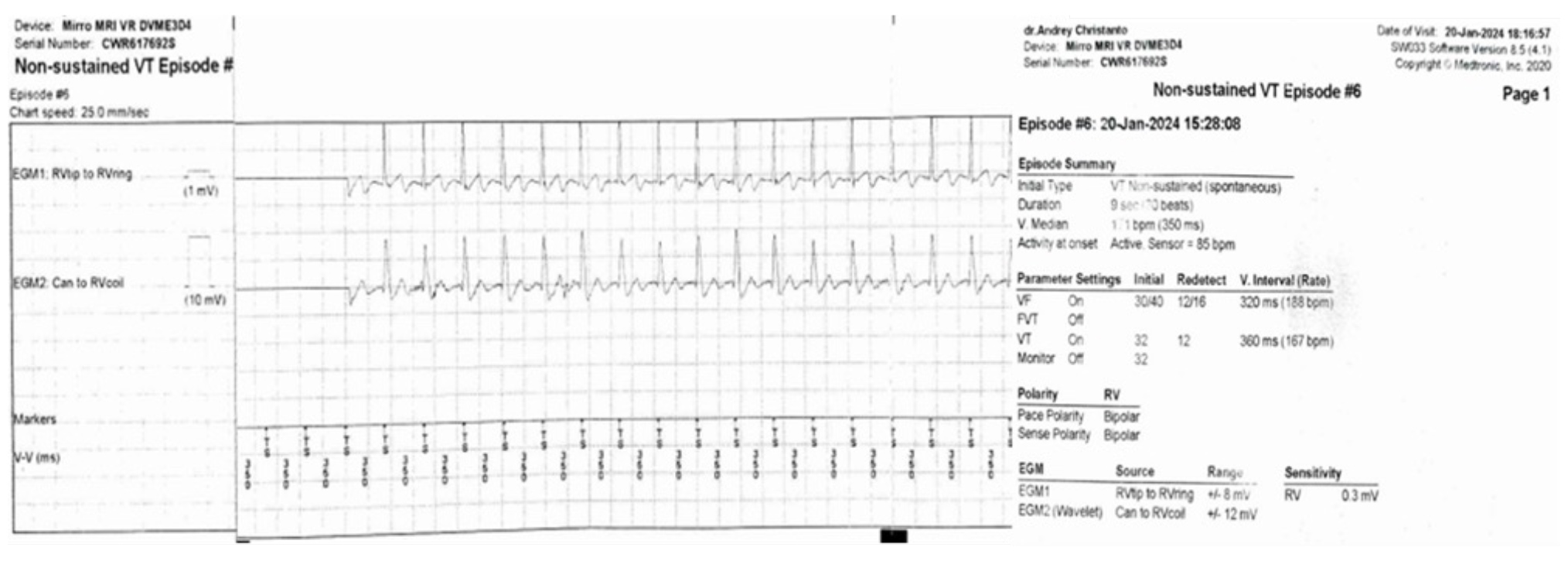
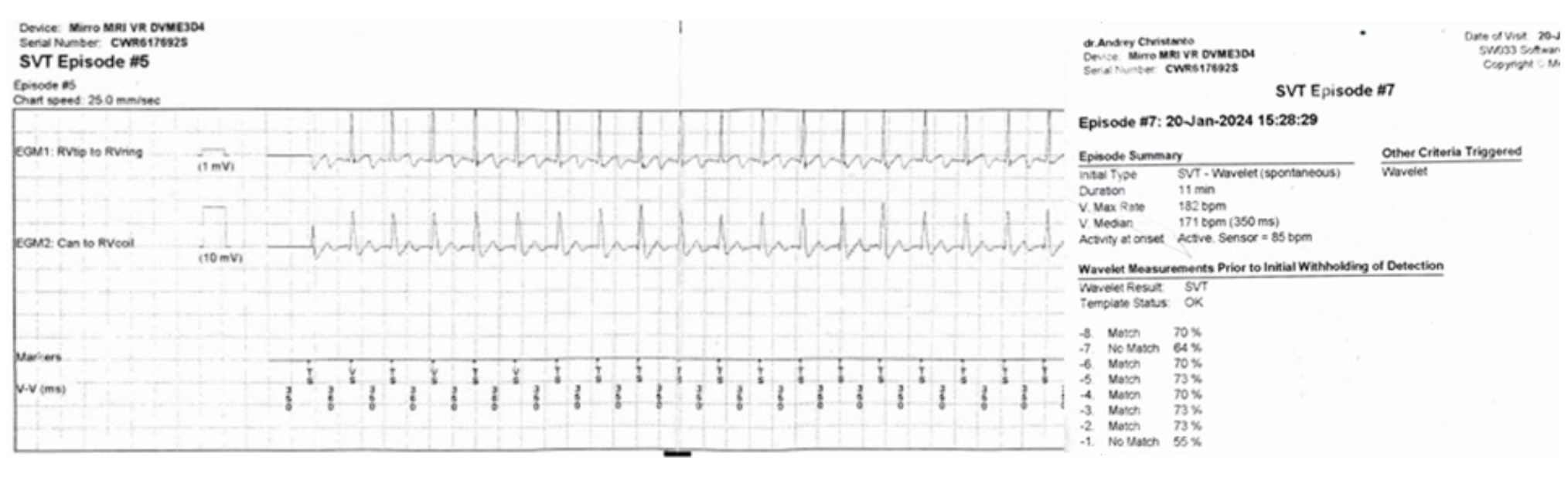
A 40-year-old man suffered seizures and cardiac arrest abruptly, without prior complaints of chest pain, when he was engaged in mild activity. Immediately, the patient initiated cardiopulmonary resuscitation (CPR), resulting in the regaining of spontaneous circulation. Six months before this admission, the patient had a single-chamber ICD implantation due to recurrent VT and a history of cardiac arrest. The patient had a medical background of coronary artery disease with complete revascularisation, and no previous occurrence of supraventricular tachycardia. In the admission to the emergency room, he regained consciousness and a 12-lead ECG showed sinus rhythm, HR 68 bpm, left axis deviation, narrow QRS, normal range QT and no ST-T changes. We began interrogating the ICD straight away, and the electrogram showed four episodes consisting of NSVT twice (duration: 2 seconds and 9 seconds) and SVT twice (duration: 28 seconds and 11 minutes). We concluded that there was an incorrect interpretation of the ICD, where VT was inaccurately identified as SVT, based on contradicting evidence from the electromyography (EGM) results. Subsequently, we performed ICD reprogramming by temporarily turning off the SVT discrimination criteria. We also continued to administer maintenance amiodarone for 24 hours to avoid recurrent VT. In the following period, the patient underwent electrophysiology studies, and no SVT was induced with normal function of the atrioventricular and sinoatrial nodes.
Figure 1. Device electrograms (EGMs) recorded in a patient with a non-sustained VT episode.
DISCUSSION
The aim of this case analysis is to find potential challenges in a single-chamber discriminator ICD that uses the morphology discrimination algorithm. An ICD uses a sequential set of steps to detect and treat ventricular tachyarrhythmias. Once the algorithms detect tachycardia, they can differentiate between SVT and VT. Oversensing or undersensing errors in event detection can result in inaccurate rateyes calculations that make this therapy inappropriate[5]. Sensing and detection accuracy are necessary for the proper classification of cardiac rhythm and the application of discrimination algorithms[6]. Sensing is the process of using filters, amplitude thresholds and blanking periods to determine when cardiac depolarisation signals occur. Oversensing occurs when the category identifies signals not related to local myocardial depolarisation, while undersensing occurs when a depolarisation remains undetected[4].
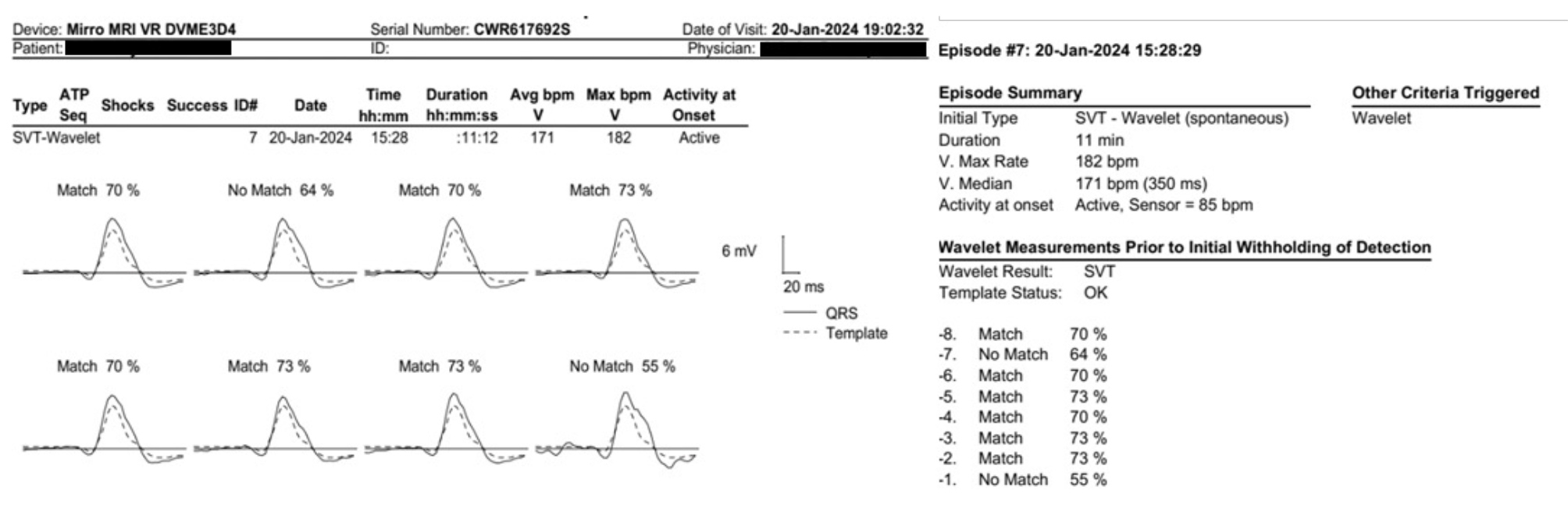
Figure 3. Morphology analysis of tachycardia electrograms (EGMs) using the wavelet.
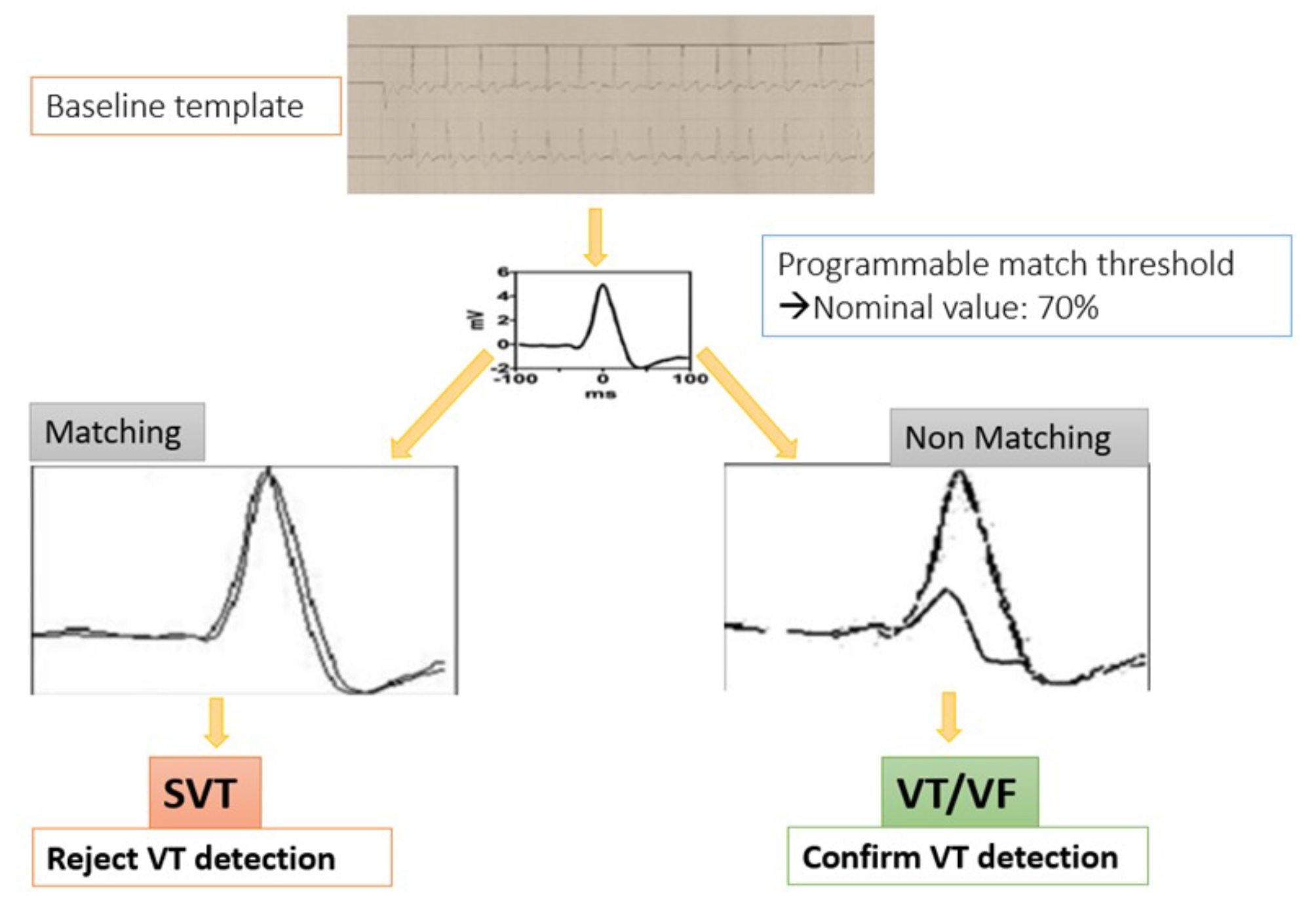
According to single-chamber discrimination, a few algorithms are applied to distinguish between SVT and VT. Every criterion used has its advantages but also has its limitations[7]. The most commonly used criteria in single-chamber discriminators are suddenness of onset, interval stability and electrogram morphology. The sudden-onset algorithm differentiates between the gradually shortening intervals during sinus tachycardia and the abrupt change in R-R intervals with the onset of VT. Stability can discriminate atrial fibrillation (unstable intervals) from VT (stable intervals) based on R-R interval regularity. The only single-chamber SVT-VT discriminator that is not interval-based is the morphology criterion. This algorithm compares the morphology of tachycardia complexes with a previously gathered sinus rhythm template using the wavelet decomposition of EGM signals[3]. An automated feature for collecting templates periodically verifies the template’s quality and updates it when modifications to the intrinsic EGM are detected[6].
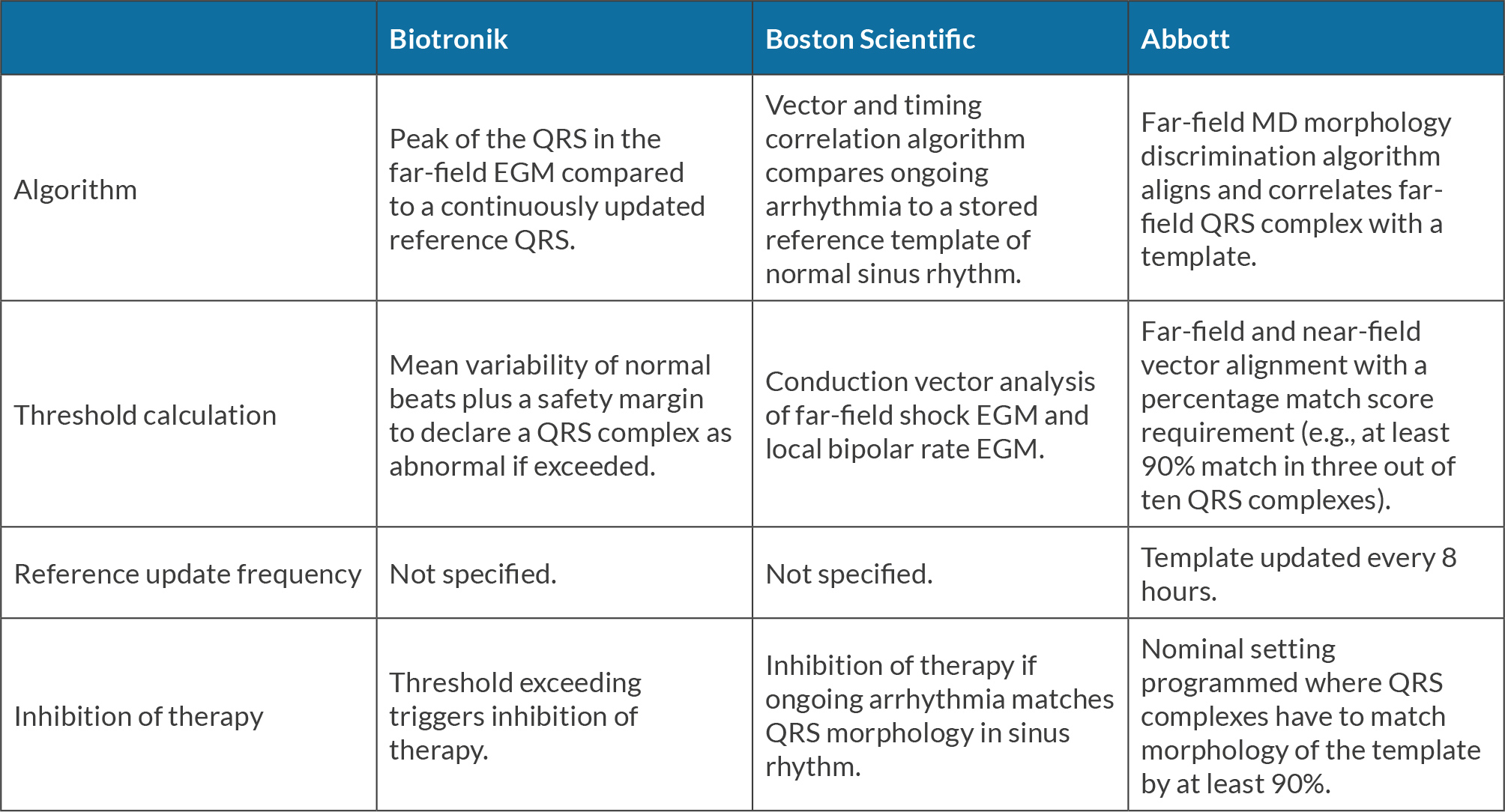
Some manufacturers establish their own algorithms for VT/SVT discrimination using different sequences of discriminators, as shown in Table 1[2]. In this case, the patient implemented a single-chamber discriminator ICD device whose data collection set-up applies the far-field vector (can to right ventricular – RV - tip) and near-field vector (RV tip to RV ring) for alignment and correlation of the far-field QRS complex with the template. The ventricular complex’s morphology, which includes the area ratios and number of positive and negative peak sequences, can be investigated. Upon detection of the episode, the morphology of every tachycardia cycle is compared with a reference. Morphology compares a reference electrogram taken in the absence of tachycardia with a ventricular electrogram recorded during the tachycardia[7]. The criterion is predicated on the notion that a ventricular complex obtained during an SVT is likely to exhibit a resemblance to a ventricular complex obtained during sinus rhythm. The complexes are classified as carried out, and the parameter supports SVT if the quantity of comparable complexes above the predetermined value (5 out of 8 or 7 out of 12, depending on the devices). Otherwise, VT is preferred[8].
Table 1. The differences in the peak of the QRS detection algorithms and their associated features between Biotronik, Boston Scientific and Abbott devices for single-chamber ICD discriminators.
The system transforms the baseline rhythm template EGM into a wavelet and stores it. The template EGM is aligned with the last eight tachycardia EGMs prior to detection, when tachycardia is identified using the VT rate criterion. The wavelet transform of each tachycardia EGM is calculated in real time[9]. A match score percentage describes the amount of morphological similarity between each tachycardia EGM and the template; VT is rejected if the matching score exceeds the programmable threshold. In the event that the matching score falls below the cut-off, VT is verified and the appropriate treatment is started[7].
This case demonstrated the identification of episodes, as evidenced by the alignment of 6 out of the past 8 waveforms with the stored template, leading to the conclusion that shock therapy should be deferred. Following this occurrence, we have made the decision to deactivate the wavelet discrimination. However, subsequent electrophysiological studies revealed the absence of SVT induction. Therefore, we can conclude that the patient experienced VT for a duration of 11 minutes, which was erroneously identified as SVT by the device.
Algorithmic-related difficulties can lead to under-detection in up to 2% of VTs, resulting in this situation. There are several possible causes why the Wavelet morphology criterion device can result in an inaccurate ICD classification. These include errors in aligning the electrograms, truncation of the electrograms (signal clipping caused by incorrect amplifier settings), distortions in the electrograms due to myopotentials, changes in the morphology of the lead over time or bundle-branch block, and distortion in the electrograms immediately after shock delivery[2,10].
A non-randomised study by Toquero et al. showed 49 of 277 VT episodes were misclassified as SVT (false positive). This number is reduced by about 42% when the programmed threshold is 75% instead of 70% (the nominal value). An additional potential vulnerability of the algorithm is noise or saturation of the EGM signal. This problem might be resolved with careful programming of the gain settings, and we prefer to extend the detection period to prevent misclassification of ICDs.