ABSTRACT
Syncope is a brief loss of consciousness caused by reduced blood flow to the brain, characterised by sudden onset, short duration and full recovery without intervention. Anamnesis, physical examination and other diagnostic tests such as laboratory analysis and electrocardiogram (ECG) can be conducted to identify the underlying cause of syncope. A Brugada pattern on an ECG in individuals with syndrome of inappropriate antidiuretic hormone secretion (SIADH) who have syncope symptoms may indicate cardiac issues. A 69-year-old man with hypertension and a history of smoking presented with syncope. His vital signs were within normal limits, with no signs of a neurological deficit. The patient met the diagnostic criteria for SIADH, as evidenced by the presence of hyponatraemia (Na 118 mmol/l), a hyperosmolar condition and euvolemia. Upon arrival, a twelve-lead ECG showed ST-segment anomalies that reflected a Brugada ECG pattern. No ventricular arrhythmias were detected during the 24-hour Holter monitoring. Coronary angiography revealed no abnormalities in the coronary arteries. The ECG demonstrated the normalisation of ST elevations and the disappearance of the Brugada ECG pattern after the correction of hyponatraemia. After three months of follow-up the patient, with a normal sodium level, had no episodes of syncope.
KEYWORDS
Syncope, Brugada-like ECG pattern, syndrome of inappropriate antidiuretic hormone secretion, SIADH
LEARNING POINTS
- Syncope in elderly patients with Brugada-like ECG patterns can arise from cardiac causes, thus necessitating more examinations.
- Severe hyponatraemia in patients with SIADH can cause syncope and a Brugada-like ECG pattern.
- Correction of hyponatraemia, after ruling out cardiac causes, can improve syncope and normalise the Brugada-like ECG pattern.
INTRODUCTION
Cardiac syncope is a life-threatening condition that necessitates immediate identification of the cause, and comprehensive treatment. The diagnosis of syncope involves anamnesis, physical examination and other tests such as laboratory tests and ECG[1]. Understanding the cause of syncope is crucial for effective treatment, especially in cases of cardiac syncope, and an ECG is a crucial tool for diagnosing the cause of arrhythmic syncope. Beyond unexplained syncope, there are several other areas where the application of monitoring devices has been explored. The primary aim of ECG monitoring is to establish an objective diagnosis by correlating the patient’s symptoms with the electrocardiographic recordings. In patients presenting with syncope symptoms, a Brugada pattern ECG can suggest potential cardiac causes[2].
Hyponatraemia, the predominant electrolyte problem in clinical practice, affects around 10% of patients when they are admitted to the hospital. The intricate processes that result in hyponatraemia can lead to confusion and misunderstandings among clinicians treating this condition. Typical signs of hyponatraemia include nausea, a history of falls, weakness and vertigo. Somnolence, disorientation, headache, convulsions and syncope have been seen in people with hyponatraemia[3]. Hyponatraemia, a symptom of SIADH, can cause syncope. An electrolyte examination in syncope patients can be a useful diagnostic technique, enhancing the information gathered from history collection and physical examination. Further investigations are required to conclusively identify the underlying reason for syncope[4].
CASE DESCRIPTION
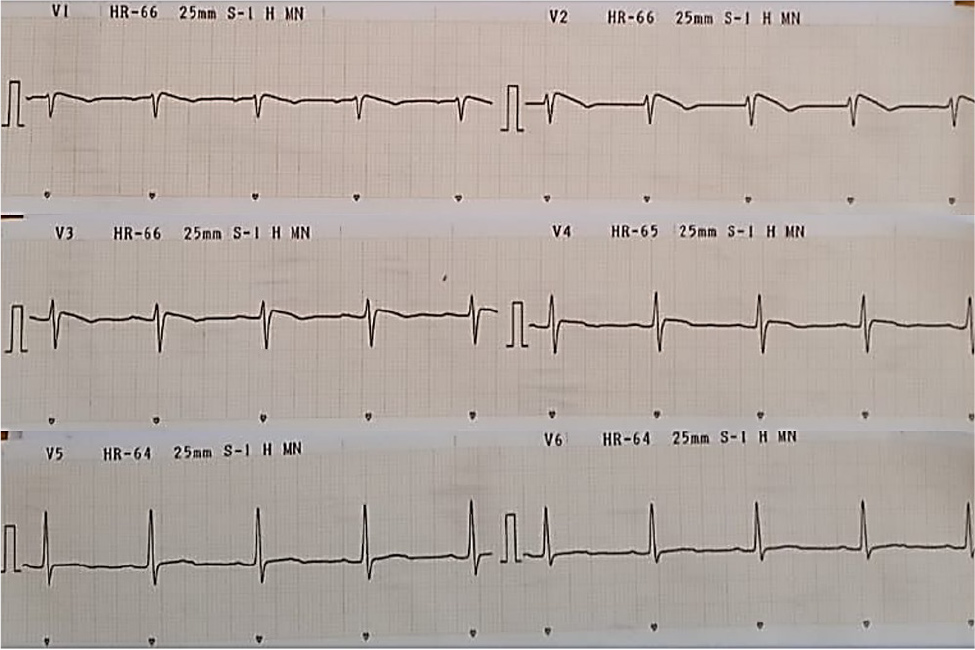
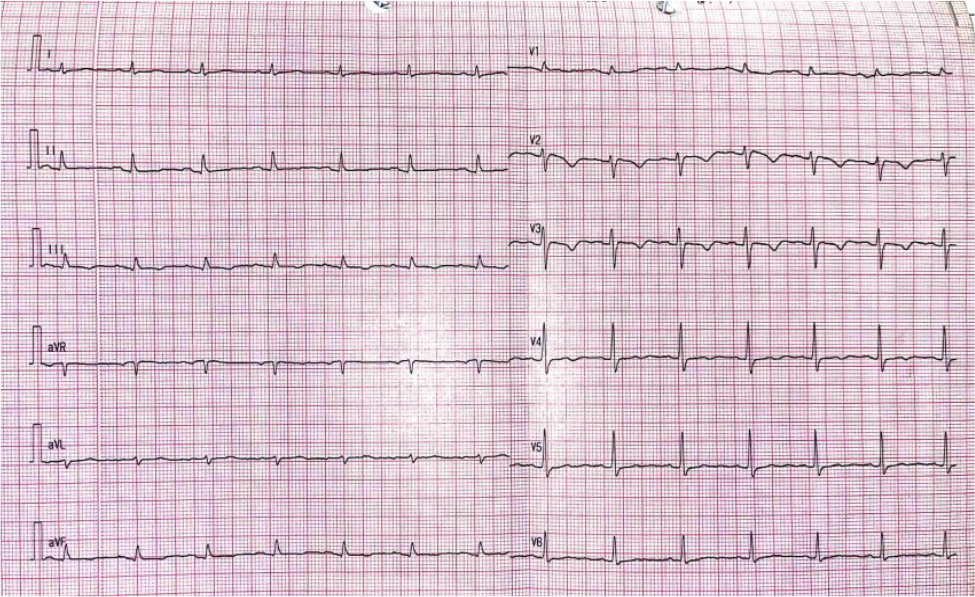
A 69-year-old man with a past history of hypertension and smoking was brought to the emergency department with recurrent syncope. The episodes of syncope occurred without prodromal symptoms such as shortness of breath, palpitations or chest pain, and lasted less than one minute. There was no family history of sudden cardiac death. The physical examination revealed a blood pressure of 135/78 mmHg, a heart rate of 57 bpm and no neurological deficits. An ECG at admission showed alterations in the ST segments and a Brugada-like pattern (serum sodium: 118 mmol/l). In both V1 and V2, the anterior precordial leads displayed a downward coving of the ST-segment with T-wave inversion, indicating a Brugada-like ECG pattern (Fig. 1). The initial laboratory results indicated low Na levels (118 mmol/l), normal potassium levels (3.52 mmol/l), normal albumin levels (3.86 g/dl), decreased blood urea nitrogen (17.9 mg/dl) and normal creatinine levels (0.93 mg/dl). Subsequent laboratory data revealed a hypoosmolar state (254 mOsm/kg, normal range 275–295) as a result of hyponatraemia (Na 121 mmol/l, normal range 135–147), decreased blood urea nitrogen (14.5 mg/dl, normal range 8–20) and normal random blood sugar (99 mg/dl, normal range 70–110). Urine electrolyte examination revealed normal urine sodium (Na urine 126 mmol/24 hrs, normal range 40–220) with normal urine production and fluid balance. The patient, presenting with hyponatraemia, hypotonicity, clinical euvolemia, urinary sodium excretion >30 mmol/l, urine concentration inappropriate for plasma osmolality and normal renal, adrenal and thyroid function, met the diagnostic criteria for SIADH. Holter monitoring did not reveal any ventricular arrhythmias. The patient underwent coronary angiography, which revealed normal coronary arteries, and correction of hyponatraemia was done through the administration of 3% NaCl and fluid restriction. During the patient’s therapy, none of the neurological symptoms usually connected to severe hyponatraemia such as seizures, disorientation and coma, occurred. Subsequent laboratory evaluations showed an improvement in hyponatraemia (Na 130 mmol/l, normal range 135–147). Syncope did not recur after the correction of the patient’s hyponatraemia during a 3-month follow-up. An ECG showed that ST elevations had normalised and the Brugada ECG pattern had disappeared (Fig. 2).
Figure 1. ECG obtained upon admission (Na 118 mmol/l) showing ST-segment changes that mimicking a Brugada ECG pattern, and a downward coving of the ST-segment with T-wave inversion in the anterior precordial leads.
Figure 2. ECG showing normalisation of ST-segment elevations at serum sodium concentration of 130 mmol/l. When compared with the admission ECG, the anterior precordial leads now exhibit a more normal ST-segment and T-wave pattern.
DISCUSSION
Syncope, characterised by a variety of causes and clinical presentations, exhibits an incidence that varies depending on the population under study[5]. The risk of hospitalisation and mortality associated with syncope is notably higher in older adults. The incidence of the first syncopal episode features a bimodal distribution: the first peak occurs in individuals between the ages of 10 and 30, and the second peak occurs in those over 65[3].
Several conditions can cause a Brugada pattern on an ECG, including Brugada syndrome (BrS), a ventricular aneurysm, early repolarisation and ST-elevation myocardial infarction. To exclude structural and ischaemic aetiologies, coronary angiography and echocardiography are necessary[6]. In patients with BrS, arrhythmic syncope is an extremely uncommon symptom of self-terminating paroxysmal ventricular fibrillation. This spontaneous arrhythmic episode lasts long enough to cause unconsciousness (perhaps longer than 5 seconds) but not long enough to result in sudden cardiac death[7].
Various conditions such as hypokalaemia, hyperkalaemia, hypercalcaemia, specific medications and fever can cause a Brugada pattern on an ECG. Previous studies have shown that hyponatraemia can induce a Brugada ECG pattern[8]. Hyponatraemia decreases the sodium inward current, maximum rate of depolarisation and conduction speed. It also reduces the shortening of the effective refractory period in the epicardium but not in the endocardium. A shift in the transmembrane sodium gradient could explain the regional difference in the extent of effective refractory period shortening and the reversibility of the Brugada pattern following sodium level normalisation[6].
SIADH secretion is defined by the abnormal release of antidiuretic hormone (ADH) that is not related to osmolality or volume status, originating from the pituitary gland or ectopically. Hyponatraemia (sodium <134 mmol/l) with hypoosmolality and euvolemia is a sign of SIADH and can be asymptomatic or can cause neurological deficits. Correction with hypertonic saline and fluid restriction can improve symptoms[3].
Syncope in elderly patients necessitates careful attention. In patients with SIADH presenting with a Brugada pattern ECG, syncope can indicate both cardiac and non-cardiac causes. A comprehensive approach involving anamnesis, physical examination and additional tests – including laboratory tests, serial ECG, Holter monitoring and coronary angiography – can be employed to exclude cardiac causes. The management of syncope in SIADH patients with a Brugada pattern ECG is dependent on the cause. If cardiac causes have been ruled out, treatment of hyponatraemia can be initiated.