ABSTRACT
Positron emission tomography (PET) has gained widespread acceptance as a valuable diagnostic tool for cancer. It is rare for a PET/CT scan to overlook the presence of metastatic disease. Sebaceous carcinoma is an uncommon malignant tumour that typically originates in the skin of the eyelid. In this case report, we present a unique case involving a metastatic sebaceous carcinoma that was not initially detected by a PET/CT scan in an 88-year-old female. Therefore, clinicians must maintain a heightened awareness of sebaceous carcinoma and exercise caution when making decisions solely based on PET scan results. It is crucial to recognise this potential limitation of PET scans in sebaceous carcinoma and consider further diagnostic approaches to ensure timely and accurate detection of sebaceous carcinoma.
KEYWORDS
False-negative PET/CT, sebaceous carcinoma, rare cancer, diagnostic limitations
LEARNING POINTS
- PET scans may miss slow-growing tumours such as sebaceous carcinoma.
- A high index of suspicion for sebaceous carcinoma is crucial, even with negative PET scans. Additional diagnostic approaches might be necessary for accurate detection.
- Sebaceous carcinoma is a rare but aggressive cancer. Diagnosis can be challenging due to its varied presentations.
INTRODUCTION
Sebaceous carcinoma, a rare malignancy that involves the skin and sebaceous glands, can be difficult to diagnose due to its varied presentations[1]. It can affect any part of the body but most often involves the head and neck regions. Metastatic sebaceous carcinoma is an even rarer entity for which treatment options are limited and are undergoing research. The positron emission tomography scan/computed tomography scan (PET/CT) is a commonly utilised diagnostic modality for determining the degree of metastasis, assessing effectiveness of cancer treatments and detecting malignancies[2]. It is highly useful and accurate in discerning between benign and malignant tumours while allowing physicians to examine the body at a cellular level. It is very rare for a PET/CT scan to miss a metastatic disease. We will discuss a case of metastatic sebaceous carcinoma that was not detected on a PET/CT scan.
CASE DESCRIPTION
The patient is an 88-year-old Caucasian woman with a past medical history of rheumatoid arthritis (on methotrexate) and osteoporosis, who initially presented to our outpatient primary clinic with complaints of ongoing neck pain for several months. The patient had been taking hydrocodone prescribed by her rheumatologist, which had not relieved her pain. She had a cervical spine radiograph that showed mild cervicothoracic levoscoliosis and demineralisation, and reported that her rheumatologist had recommended denosumab injections, given her history of osteoporosis; however, she declined. The patient did coincidentally have bilateral lower extremity neuropathy so a magnetic resonance imaging (MRI) of the neck was ordered, and she was referred to pain management.
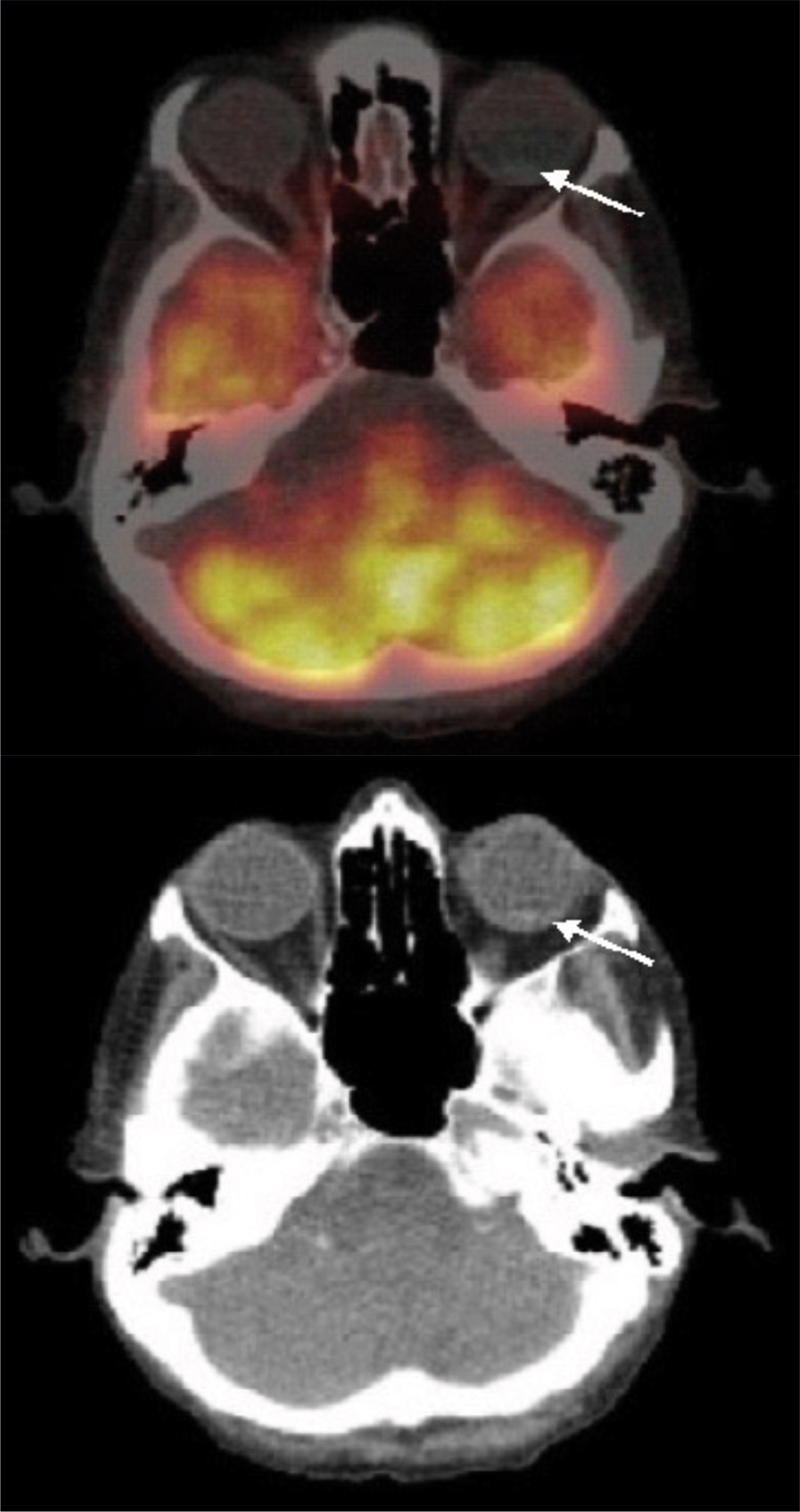
Figure 1. Axial images of the 18F-fluorodeoxyglucose positron emission tomography-CT (left) and CT (right) show a soft-tissue mass 9.6 × 0.8 mm (white arrow) without increased uptake in the posterior left eye.
An MRI of the neck showed significant inflammatory oedema and swelling of the left inferior neck in the posterior cervical space, deep to the sternocleidomastoid muscle. This area of inflammation measured 9 cm transversely and 11 cm inferiorly and included internal hyperplastic lymph nodes. In addition, there was extension of the oedema signal to the superior mediastinum and left supraclavicular fossa and an enlarged soft tissue nodule in the right neck inferior to the parotid gland, which could represent a parotid neoplasm or hyperplastic lymph node. The patient was then referred to oncology regarding the neck swelling. Oncology ordered a PET/CT scan and discussed the possibility of a biopsy afterwards. The PET/CT scan showed no neck swelling but a right cervical lymph node with mild activity that was smaller than prior MRI; there was no evidence of malignancy. At this point there was no oncological explanation for her head and neck pain. However, the patient’s pain persisted, and she subsequently underwent a biopsy which showed a sebaceous carcinoma with metastasis to the lymph node, with an immune profile supporting the diagnosis. The patient was referred to dermatology; however, no primary lesion was found on examination. She was seen by Ear, Nose, And Throat Department, who did not recommend surgical intervention due to her age. She also had an MRI of the brain that revealed an enhancing soft tissue mass identified in the left globe, measuring 7 mm. The patient was seen by a retina specialist for a potential biopsy. Initially a direct examination was difficult because of retinal scarring. In addition, a biopsy was unable to be performed because it would involve removing the eye and there was no direct cancer evidence. Patient treatment options were discussed with the patient and she was offered radiotherapy, however she and her family ultimately declined therapy and decided to pursue hospice care.
DISCUSSION
Sebaceous carcinoma is a rare and aggressive form of cancer that originates from the sebaceous glands, responsible for producing oil in the skin. While it primarily manifests on the eyelids, face and scalp, it can also arise in other areas of the body containing sebaceous glands. Depending on its location, sebaceous carcinoma can be categorised into two types: periocular (occurring around the eyes) and extraocular (occurring outside the eye area).
The average age of diagnosis for periocular and extraocular sebaceous carcinoma is approximately 67 years[3]. Periocular sebaceous carcinoma tends to occur more frequently in women, whereas extraocular sebaceous carcinoma is more commonly observed in men. Ocular sebaceous carcinomas primarily originate from the meibomian (tarsal), Zeis (eyelash), or sebaceous glands located on the eyelid and caruncle. The exact source of extraocular sebaceous carcinoma is less clearly defined. Extraocular sebaceous carcinoma typically presents as a yellowish-tan nodule, often with ulceration, primarily occurring on the head and neck region. In some cases, it may also appear on the trunk or extremities, although this is less frequently observed[4]. The exact mechanism behind the development of sebaceous carcinoma is not yet fully elucidated[5]. The majority of sebaceous carcinomas are solitary and sporadic, occurring without any known genetic abnormalities. However, there is a subset of cases that are associated with genetic defects. Due to the diverse clinical and histological features exhibited by sebaceous carcinoma, accurate diagnosis can be challenging. Patients with ocular sebaceous carcinomas often present with eyelid tumours that fail to heal, which are commonly misdiagnosed as more prevalent, benign conditions such as chalazion, blepharitis, conjunctivitis or other inflammatory disorders[6]. There is no definitive presentation or characteristic sign that points directly to sebaceous carcinoma, often resulting in a significant delay in diagnosis spanning from months to years[7].
PET scans are a valuable imaging test utilised for cancer detection. They operate by detecting fluorodeoxyglucose (FDG), a modified radioactive glucose. Cancer cells have a higher FDG uptake compared to healthy cells, allowing PET scans to reveal areas with increased FDG uptake, potentially indicating the presence of cancer. However, in certain instances, PET scans may miss the detection of sebaceous carcinoma. This is primarily due to the slow-growing nature of sebaceous carcinomas, resulting in lower FDG uptake compared to other types of cancer. Consequently, cancer cells may not take up enough FDG to be detected. Furthermore, PET scans may have limitations in detecting small tumours, or tumours located in areas with abundant normal tissue, such as the brain.