ABSTRACT
Introduction: Biloma is an uncommon form of liver abscess composed of bile usually associated with procedures of the biliary tree and gallbladder. Cholangitis can be acute or chronic, can result in partial or complete obstruction of the flow of bile. The infection of the bile is so common, that positive blood cultures are highly characteristic. In the case of a suppurative cholangitis with signs of sepsis treatment alone with antibiotics is usually not sufficient to achieve medical remission. Multiple hepatic abscesses are often present, and the mortality approaches 100% unless prompt endoscopic or surgical relief of the obstruction and drainage of infected bile are carried out. Endoscopic retrograde cholangiopancreatography ERCP with endoscopic sphincterotomy is the preferred initial procedure for both establishing a definitive diagnosis and providing effective therapy.
Case description: We present the case of a 69-year-old female patient with complex chronic comorbidities who presented with acute cholangitis initially managed with endoscopically inserted stent and later complicated by sepsis and biloma formation. The bile was drained, and it showed an infection with Candida spp. requiring antifungal therapy.
Conclusions: The failure to perform sphincterotomy in patients with suppurative cholangitis can contribute to the backflow of bile and worse outcomes.
KEYWORDS
Diseases of the bile ducts, biloma, endoscopic retrograde cholangio pancreatography, ERCP, ascending cholangitis
LEARNING POINTS
- Biloma formation is a rare complication of biliary duct procedures and diseases such as cholangitis. A prompt identification of signs of complications in patients with disease of the biliary ducts is key in preventing clinical deterioration.
- Sphincterotomy is vital in the management of ascending cholangitis, as it prevents backflow of bile into the intrahepatic biliary system.
- The presence of multiple comorbidities in complex cases can become an obstacle to optimal management and drainage of septic bile.
INTRODUCTION
A biloma is an encapsulated, intra-abdominal collection of bile inside or outside the biliary tree. It is a rare condition with an incidence of 0.3–2%. Biloma can occur after intra-abdominal trauma, choledocholithiasis or iatrogenic injury which leads to disruption of the biliary tree and bile leakage in the abdominal cavity. Biloma after endoscopic retrograde cholangiopancreatography (ERCP) is very rare. We present the case of a complex patient whose clinical condition was complicated by an insidious biloma. This case highlights the importance of physician awareness about this rare complication. Even though biloma after ERCP is an unusual complication, differential diagnosis of patients with right upper quadrant discomfort following an iatrogenic event should always include biliary tree disruption.
CASE DESCRIPTION
We present a 69-year-old female patient with a history of cholecystectomy one year prior to presentation, chronic pancreatitis, type 2 diabetes, deep venous thrombosis, gastrointestinal bleeding, end-stage renal disease, and coronary and peripheral artery disease. She presented to the emergency department with abdominal pain, fever and nausea for the previous two days. The abdominal pain was located in the epigastric region and in the right upper quadrant, non-radiating and associated with nausea. On admission, she presented with a temperature of 36.7°C, blood pressure levels were 161/70 mmHg, the respiratory rate was 15 rpm and the saturation of oxygen was 96% while breathing ambient air. Initial laboratory tests showed signs of acute sepsis and liver injury as shown in Table 1.
Table 1. Complete blood count and metabolic panel on initial clinical presentation.
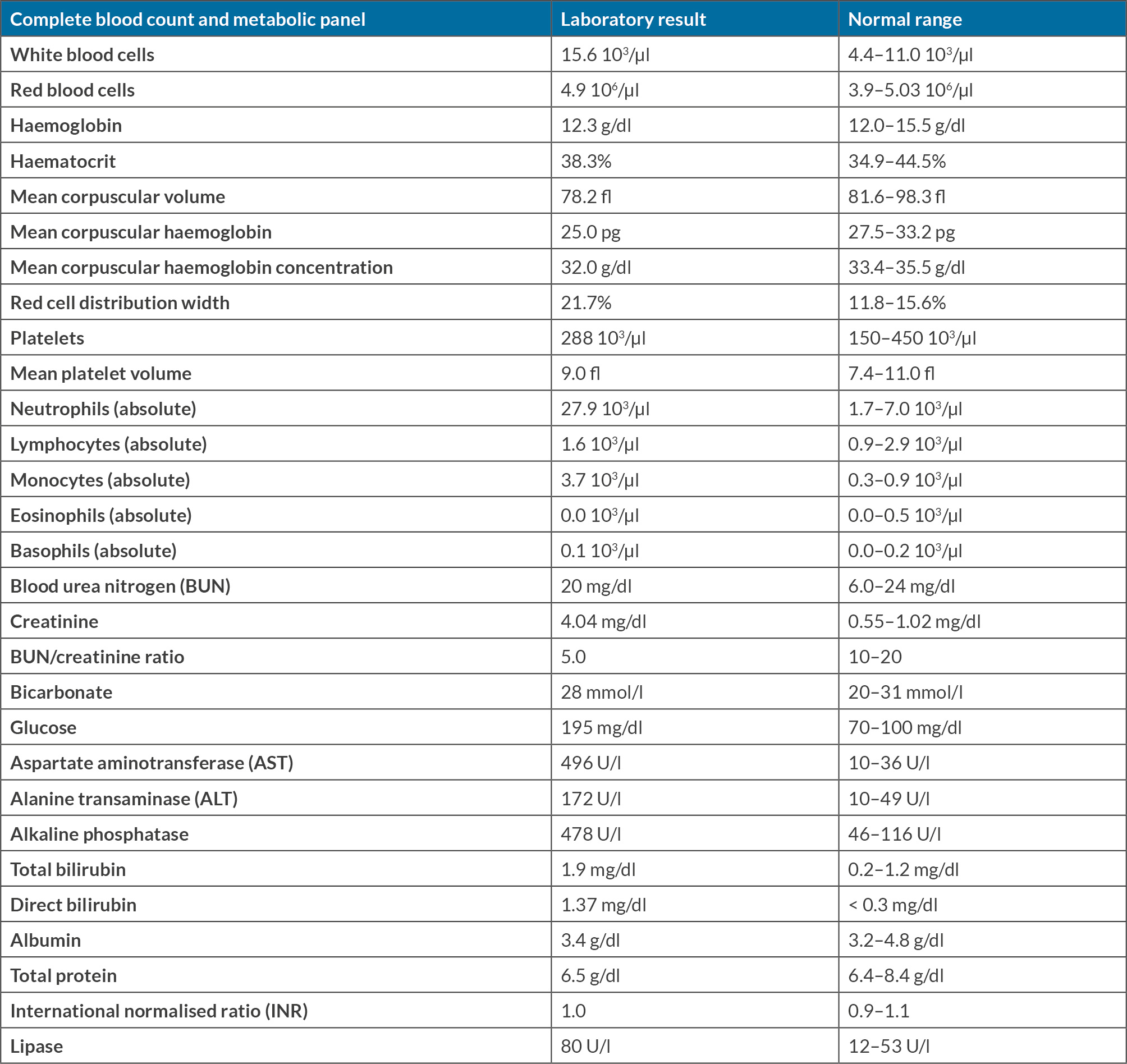
The patient was admitted for monitoring in view of a high suspicion of acute ascending cholangitis, for management with intravenous meropenem administration and further diagnostic assessment. Initial evaluation with magnetic resonance cholangiopancreatography (MRCP) showed a filling defect in the distal common bile duct measuring 5.8 mm (Fig. 1), representing a possible common bile duct stone. There was dilatation of the intrahepatic biliary tree with irregular appearance of the biliary wall. These findings were not present on a previous MRCP performed one month previously.
Figure 1. Magnetic resonance cholangiopancreatography filling defect in the distal common bile duct (green arrow).
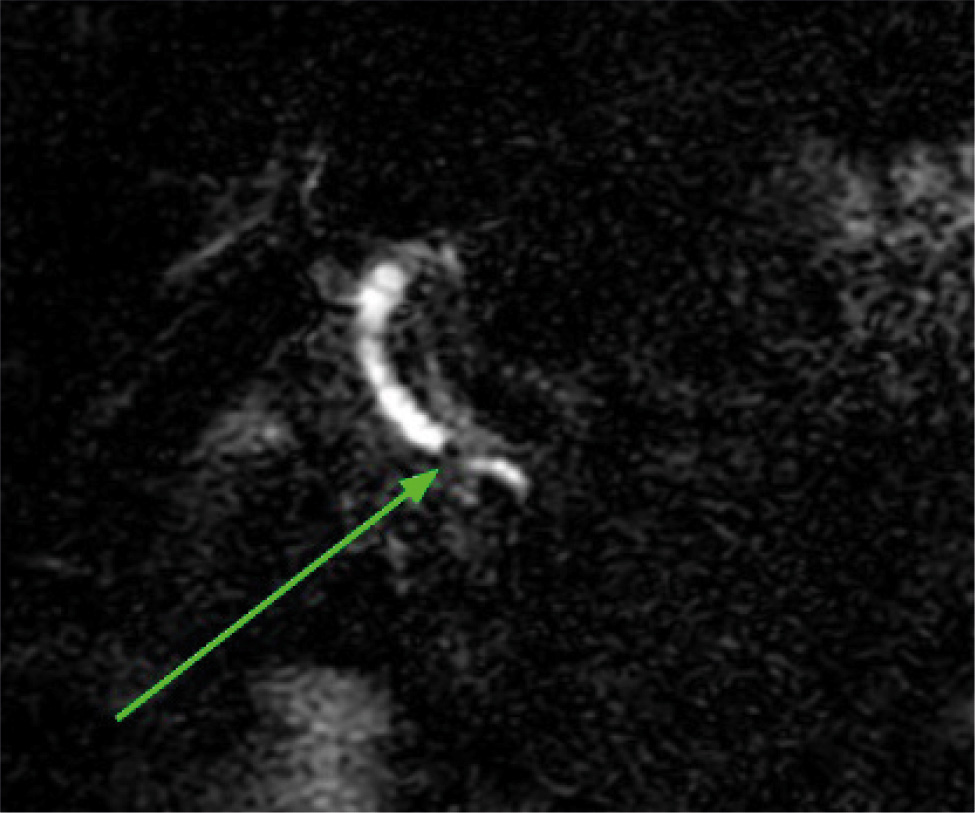
The patient was resuscitated with intravenous fluids, antibiotics were switched to piperacillin/tazobactam, one dose of gentamicin was administered intravenously with supportive measures, and an emergency ERCP was done (Fig. 2). This showed surgical clips consistent with a previous cholecystectomy, the major papilla was bulging, and sludge was emerging from it. A 7-Fr by 7 cm plastic stent with a single external flap and a single internal flap was placed into the common bile duct with good position confirmed; pus flowed through the stent. A sphincterotomy was not performed due to the patient being on acute coronary syndrome protocol treatment with dual antiplatelet therapy.
The patient’s clinical course was complicated by an acute non-ST-elevation myocardial infarction. She underwent a cardiac catheterisation after ERCP, which showed a large calibre left main artery bifurcating into a left anterior descending (LAD) and a left circumflex artery (LCX), which had no significant stenosis. The LAD was a large vessel with no significant stenosis and the LCX showed distal calcified stenosis. The right coronary artery had a complete total occlusion in the ostial segment, with a large collateral supplying the vessel from the left circulation. The patient had a left ventricular end-diastolic pressure of 22 mmHg. No intervention was done in the occlusion and medical management was established.
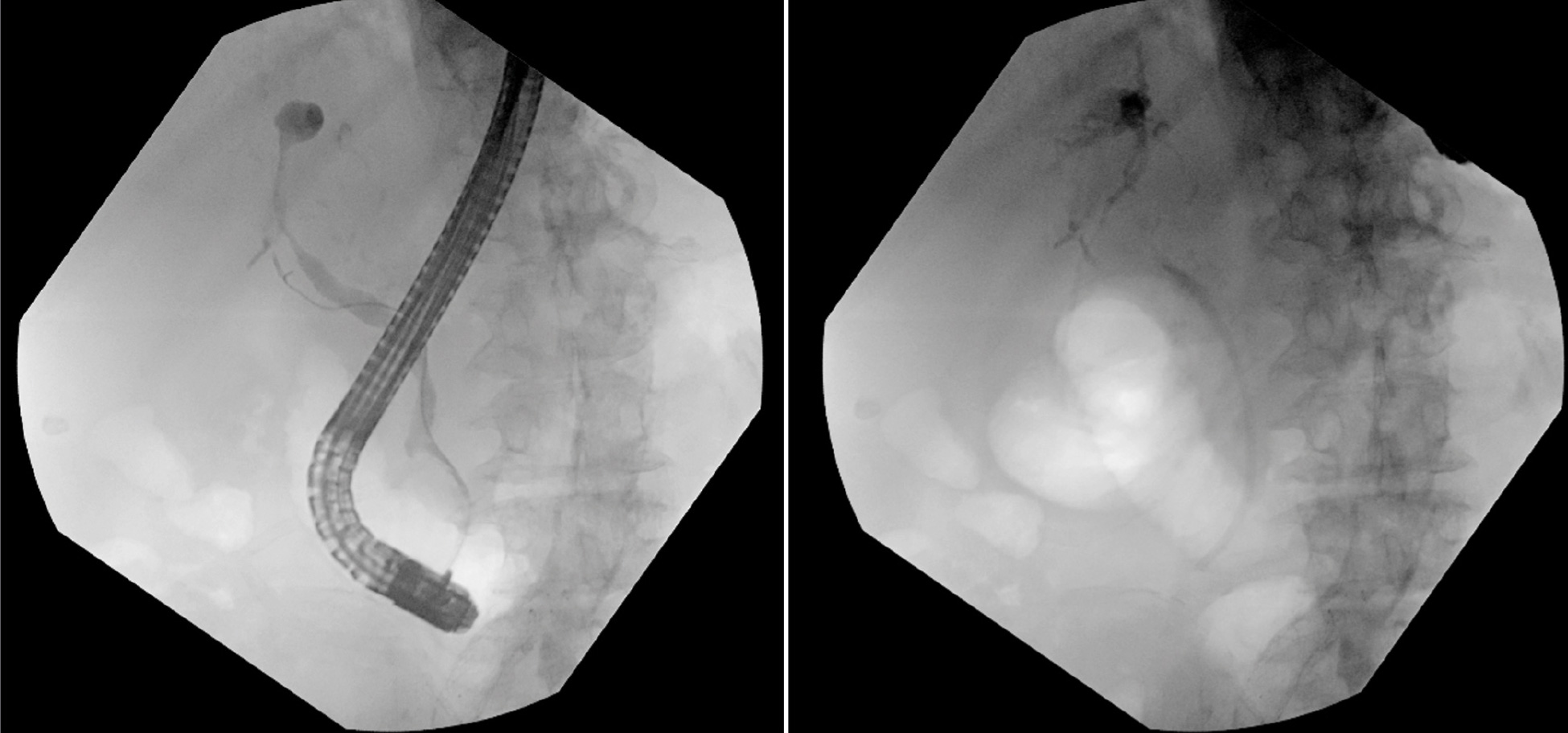
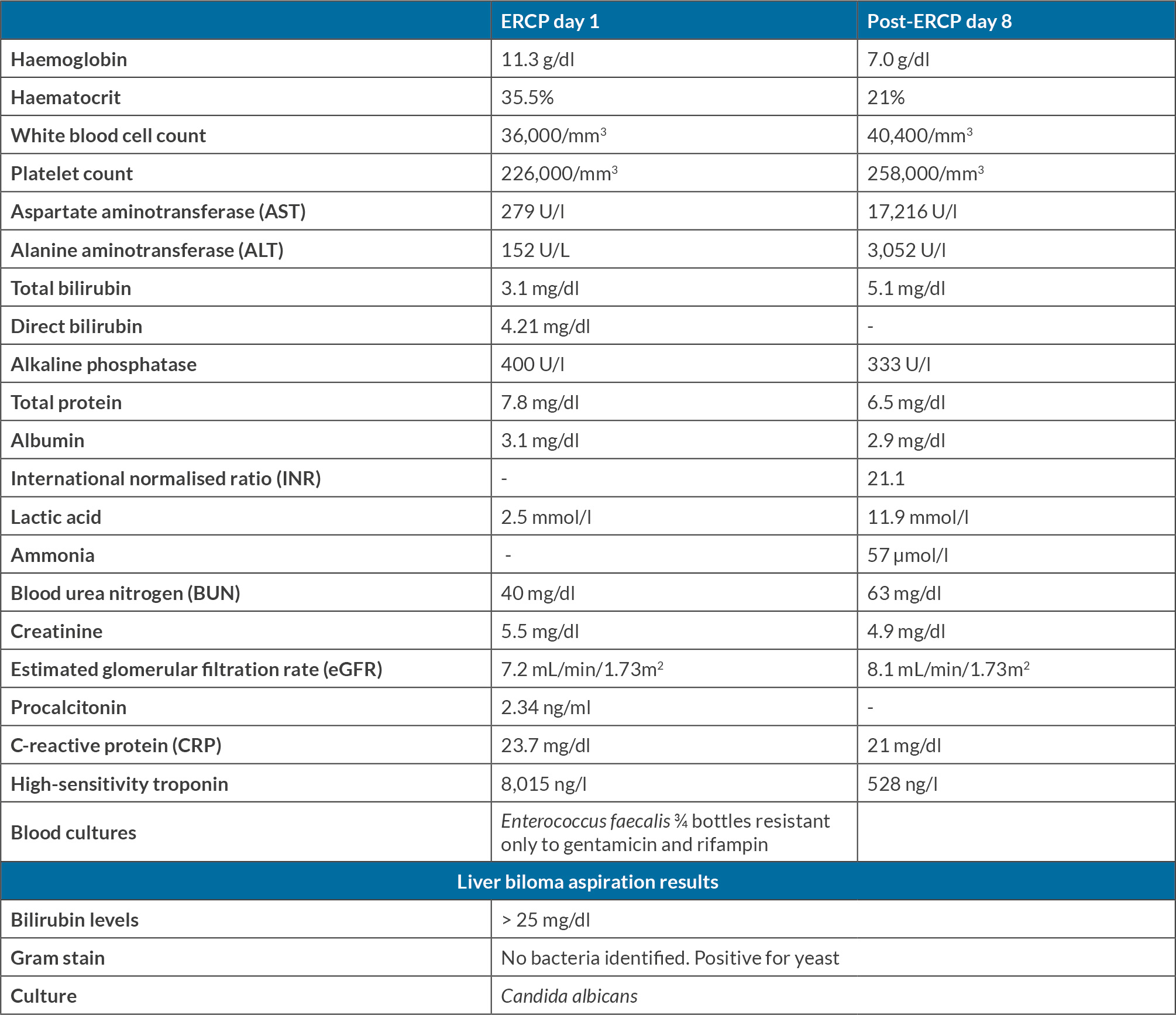
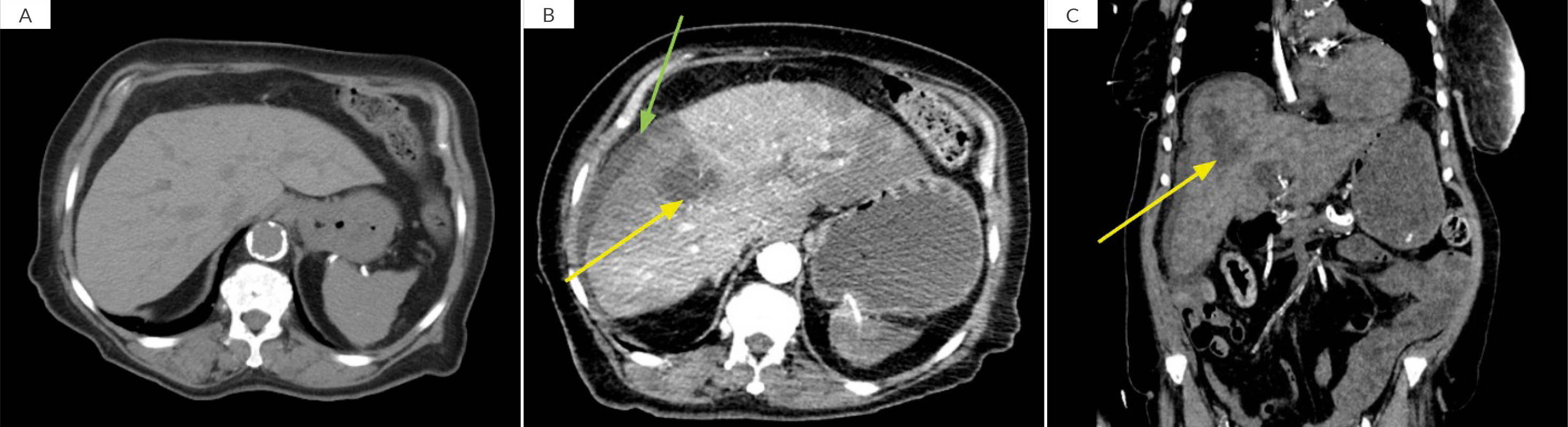
The patient’s past medical history was notorious for end-stage renal disease, for which she received haemodialysis three times per week via a tunnelled central venous catheter. Her blood cultures obtained from the central line were positive for Enterococcus faecalis secondary to thrombophlebitis, and the line was removed. Antibiotic therapy was adjusted and changed to vancomycin, and daptomycin was started and administered with dialysis sessions. The patient’s symptoms improved modestly. Her laboratory tests showed a downtrend of white blood cells, which did not reach normal levels; a transoesophageal echocardiogram was negative for vegetations. Over eight days, the patient remained afebrile and was improving clinically except for very mild abdominal discomfort, which was assumed to be secondary to stent placement. On day eight after ERCP, the patient’s blood pressure levels started to decrease, along with increasing intractable abdominal pain. The patient’s physical examination showed an acute onset of increasingly severe abdominal pain, exquisitely tender to superficial palpation, and mild jaundice. After fluid resuscitation was established, an emergency laboratory test revealed signs of acute worsening infection (Table 2). Immediate imaging revealed signs of rupture liver abscess (Fig. 3), for which the multidisciplinary team of general surgery, invasive radiology, gastroenterology and infectious disease was activated and notified, and further management started to be discussed. The patient underwent an emergency ultrasound-guided liver fluid drainage, which revealed the appearance of bilious content (Fig. 4). She was supported with norepinephrine infusion, haemodialysis and blood products as needed. Carbapenem-based antibiotic therapy was started, along with intravenous vancomycin. Blood cultures were negative later on, and the drained fluid grew Candida Albicans in the culture media sent for analysis. Given the sample’s results suggestive of yeast growth, micafungin therapy was initiated as well. The patient’s further clinical progression stabilised in general, and a total of 750 ml of bilious content was drained in the first five days of diagnosis.
Table 2. Change in levels of metabolic markers and serologic tests on day 1 and day 8 post-endoscopic retrograde cholangiopancreatography.
Figure 3. CT of the abdomen showing a heterogenous attenuation of the liver with a large ill-defined low attenuated abnormality in the anterior right hepatic lobe (yellow arrow in B and C) extending to the capsule (green arrow in B). There are signs of hepatomegaly and micronodular contour of the liver. The findings are new compared to previous CT of the abdomen performed on initial presentation (A).
Figure 4. Aspirated content from drainage of the liver ruptured abscess, which turned out to be diagnostic for biloma.
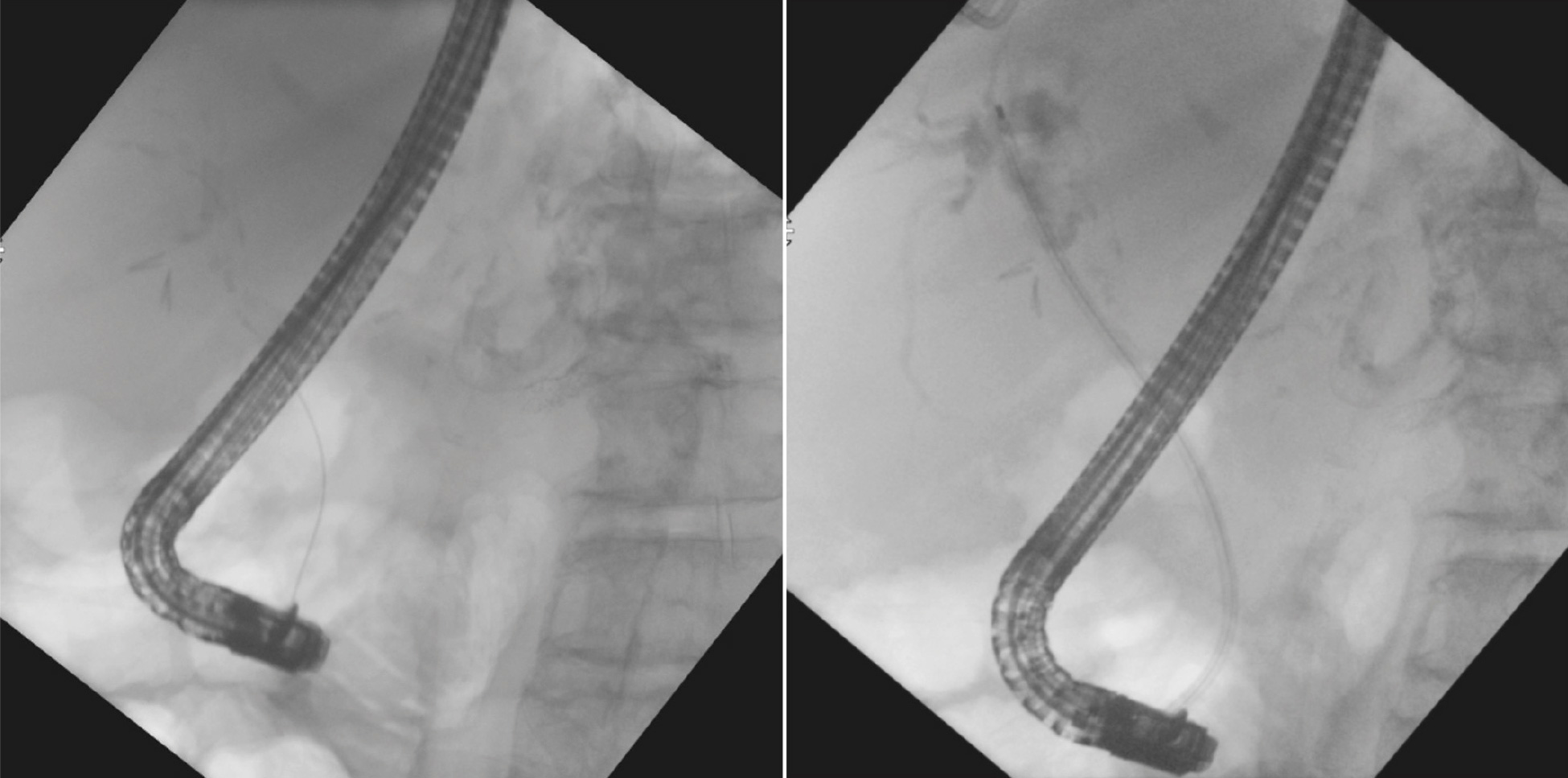
ERCP was performed 14 days after initial intervention with the intention to perform a sphincterotomy. Placement of a wire into the biliary tree was attempted; however, this would not pass. A long cystic duct stump originated in the biliary system; the wire entered the cystic duct and was unable to selectively cannulate the common hepatic duct that was suspected to be obstructed. The bile duct was explored endoscopically using a direct visualisation system, which was advanced to the bifurcation – visibility with the scope was good. The common hepatic duct was partially obstructed by what appeared to be a stone. The system was used to advance the wire through the common hepatic duct into the right intrahepatic duct. The visualisation system was exchanged for a balloon, the biliary tree was swept with a 12 mm balloon starting at the right main hepatic duct. Sludge was swept from the duct and a few stones were removed; no stones remained. One 10-Fr by 12 cm plastic stent was placed into the common bile duct past the site of the cystic duct staples. Bile and sludge flowed through the stent, which was in a good position. These findings were consistent with choledocholithiasis with a partial obstruction and complete removal was accomplished by biliary sphincterotomy and balloon extraction (Fig. 5). A repeated computerised tomography (CT) scan of the abdomen showed residual fluid accumulation, which was newly drained by invasive radiology. Samples were sent to the laboratory for culture and Candida species were growing in the new sample. The patient improved on therapy with intravenous micafungin and fluconazole, with serum (1,3)-β-d-glucan levels showing a downtrend on follow-up.
DISCUSSION
In 1979, Gould and Patel first described a biloma as an encapsulated bile collection outside the biliary tree, which expanded the term to encompass both extrahepatic and intrahepatic collections[1]. Although the exact pathophysiology of biloma formation remains unclear, factors such as persistent pressure in the biliary ducts, biliary obstruction or infarction are implicated in its formation. Clinical presentations vary widely, ranging from non-specific abdominal pain to severe biliary sepsis, depending on the location, size and underlying cause. Traumatic or postsurgical bilomas tend to be larger and are more readily diagnosed due to pronounced symptoms[2]. In the presence of significant risk factors, biloma formation can be an incidental imaging finding in the setting of symptoms such as discomfort in the right upper quadrant, abdominal fullness, nausea, vomiting, fever, jaundice and peritonitis[3].
Only a few cases of this complication following ERCP have been documented in the literature. The reported causes of biloma formation after ERCP have been attributed to aspects of the endoscopic procedure, including the injection of contrast medium through the catheter leading to increased pressure in the proximal biliary ducts and modification to the biliary epithelium due to persistent cholangitis[3].
We encountered a patient with acute ascending cholangitis for which an ERCP with stent placement in the bile duct and without sphincterotomy was performed. This patient, presenting with severe abdominal pain, highly elevated liver function tests (more than fifteen times the upper limit of normal elevation in aspartate aminotransferase (AST) and alanine transaminase (ALT)), leukocytosis, shock and metabolic acidosis raised suspicion for hepatic abscess and biliary disease complicating her clinical course. This prompted a comprehensive radiological evaluation to confirm the diagnosis and determine an optimal strategy for treatment. Ultrasound is a readily available tool that allows for rapid recognition of fluid collection and evaluation of abdominal organs. In our case, CT was the preferred first modality of imaging used to detect hepatic fluid collection and it revealed a hypoattenuating subcapsular collection, aiding in the differential diagnosis from other postprocedural complications. Smaller bilomas can evade detection on ultrasound, therefore abdominal CT scans are considered to have higher sensitivity. Invasive procedures such as ERCP and percutaneous transhepatic cholangiography play crucial roles in cases requiring intervention. Percutaneous transhepatic biliary drainage, guided by imaging, offer both diagnostic insights and therapeutic benefits, often avoiding the need for surgical intervention. While non-operative management remains the preferred approach for most cases of biloma formation, surgical intervention becomes necessary in instances of unsuccessful drainage, the presence of multiloculated lesions or persistent bile leaks[3]. Biloma is known to confer poorer outcomes and prognosis in patients with different complicated diseases of the biliary tree such as cholangiocarcinoma and cholelithiasis, as well as a postoperative course of cholecystitis and endoscopic procedures[4].
MRI coupled with MRCP has been shown to be helpful in cases requiring detailed evaluation of the biliary tree and identification of leakage sites. Bile is mostly composed of isotonic fluid and bile acids. A biloma will produce a variable signal on T1-weighted images and a high signal intensity on T2-weighted images on MRI, confirming the presence of concentrated bile within the collections on suspicious liver lesions. Other modalities as functional imaging techniques such as hepatobiliary cholescintigraphy using Tc(99m) iminodiacetic acid can also assess the integrity of biliary system. Hepatobiliary iminodiacetic acid (HIDA) scans facilitated the detection of active biliary leaks, guiding subsequent therapeutic interventions[3].
In conclusion, the management of bilomas entails a multidisciplinary approach with a significant reliance on radiological imaging techniques. By integrating various modalities, clinicians can accurately diagnose bilomas, guide therapeutic interventions and optimise patient outcomes in this challenging clinical scenario.