ABSTRACT
Introduction: Fever of unknown origin (FUO) refers to a condition of prolonged increased body temperature, without identified causes. The most common cause of FUO worldwide are infections; arthropod bites (loxoscelism) should be considered in view of the spread of the fiddleback spider. Loxoscelism can present in a cutaneous form (a necrotic cutaneous ulcer) or in a systemic form with fever, haemolytic anaemia, rhabdomyolysis and, rarely, macrophage activation syndrome (MAS). For this suspicion, it is important to have actually seen the spider.
Case description: A 71-year-old man was admitted to our department because of intermittent fever, arthralgia and a necrotic skin lesion on his right forearm that appeared after gardening. Laboratory tests were negative for infectious diseases, and several courses of antibiotics were administered empirically without clinical benefit. Whole-body computed tomography showed multiple colliquative lymphadenomegalies, the largest one in the right axilla, presumably of reactive significance. A shave biopsy of the necrotic lesion was performed: culture tests were negative and histological examination showed non-specific necrotic material, so a second skin and lymph node biopsy was performed. The patient developed MAS for which he received corticosteroid therapy with clinical/laboratory benefit. Cutaneous and systemic loxoscelism complicated by MAS was diagnosed. Subsequently, the second biopsy revealed morphological and immunophenotypic findings consistent with primary cutaneous anaplastic large cell lymphoma (PC-ALCL).
Conclusions: Skin lesions and lymphadenomegalies of unknown origin should always be biopsied. It is very common to get indeterminate results, but this does not justify not repeating the procedure to avoid misdiagnosis.
KEYWORDS
Cutaneous ulcer, fever of unknown origin (FUO), loxoscelism, macrophage activation syndrome (MAS), primary cutaneous anaplastic large cell lymphoma (PC-ALCL)
LEARNING POINTS
- In case of necrotic skin lesions with fever, malignancy (and in particular cutaneous lymphoma) should always be considered.
- Misdiagnosis of loxoscelism is common. Definitive diagnosis requires the identification of the responsible spider.
- It is frequent to obtain inconclusive results from biopsies, but this does not justify not repeating the procedure to avoid misdiagnosis.
INTRODUCTION
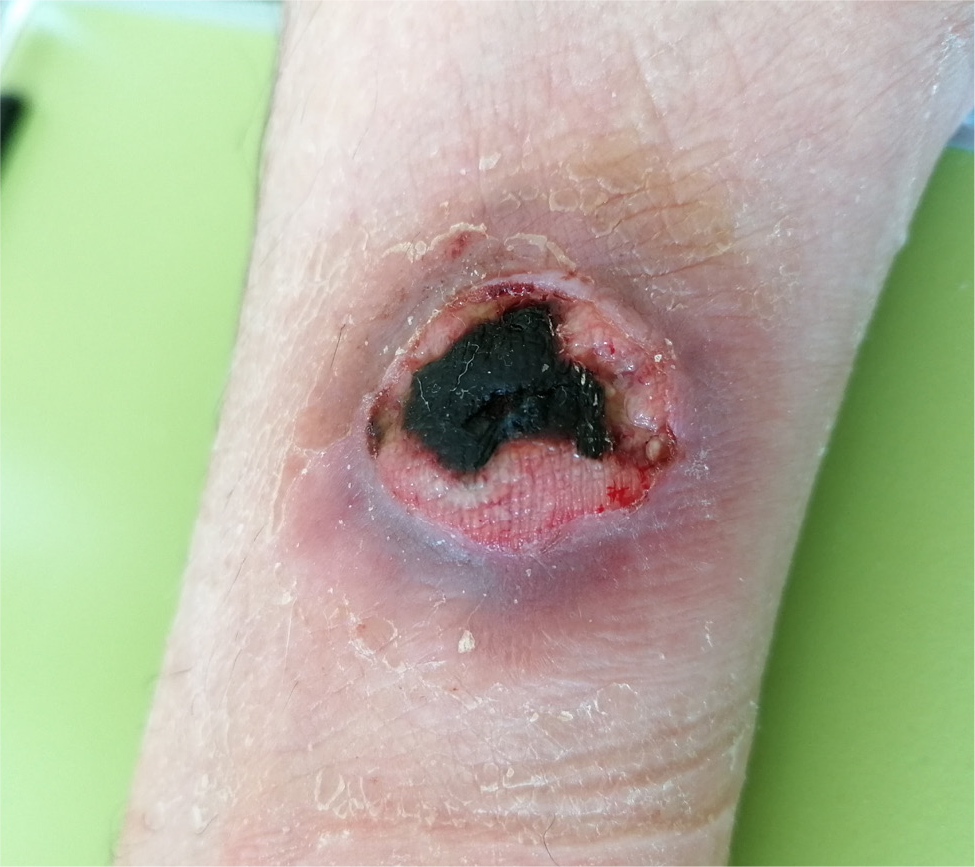
The acronym FUO (fever of unknown origin) refers to a condition of prolonged elevation of body temperature without an identified cause, in the absence of focal reminder signs and symptoms[1]. The most common cause of FUO is infections, and tuberculosis is the leading cause. Exposure to insects (e.g. arthropod bites) should also be considered. Autoimmune diseases and malignancies should always be suspected (in particular, lymphoma)[2]. Loxoscelism, the bite of spiders of the genus Loxosceles, known as fiddleback spiders, is the only arachnological cause of dermonecrosis. Loxosceles species are found in tropical regions and also in Europe. Loxoscelism can occur in two forms: cutaneous and systemic. The spider bite causes oedema, erythema and a painful, reddish bullae around which develops a cyanotic area with ischaemic margins. Successively, the centre of the lesion necrotises and ulcerates concentrically[3]. The most common sites are the proximal lower and distal upper extremity. In terms of systemic involvement, spider bites can cause haemolytic anaemia, acute kidney injury and rhabdomyolysis. As documented in a child in Turkey, loxoscelism can cause secondary haemophagocytic lymphohistiocytosis (HLH)[4]. Diagnosis is clinical, based on the appearance of the skin lesion, but definitive diagnosis can be challenging because the responsible spider may be difficult to find. Misdiagnosis is common. Differential diagnoses include other causes of idiopathic necrotic lesions: infections, neoplasms (basal cell carcinoma, lymphoma) or vascular disorders[5]. Currently, there is no evidence-based effective therapy for loxoscelism.
CASE DESCRIPTION
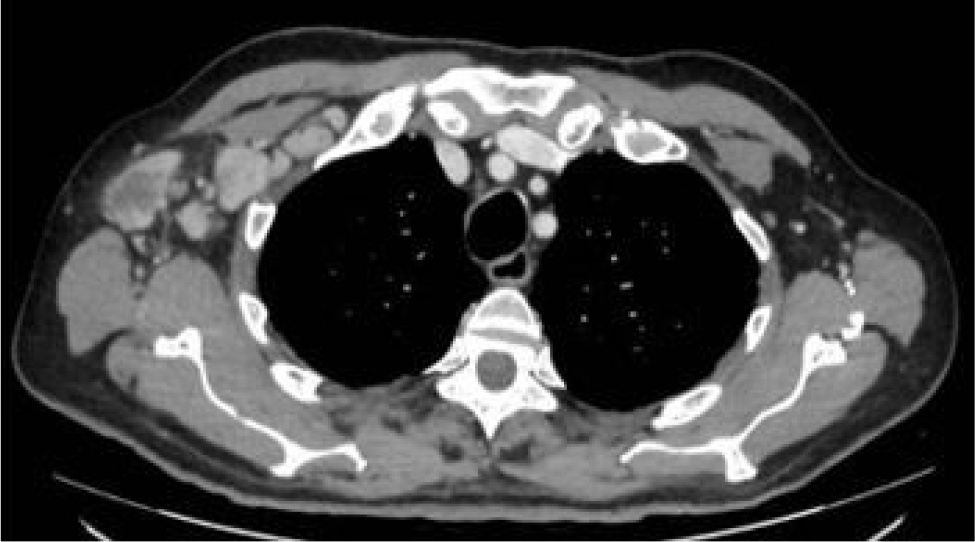
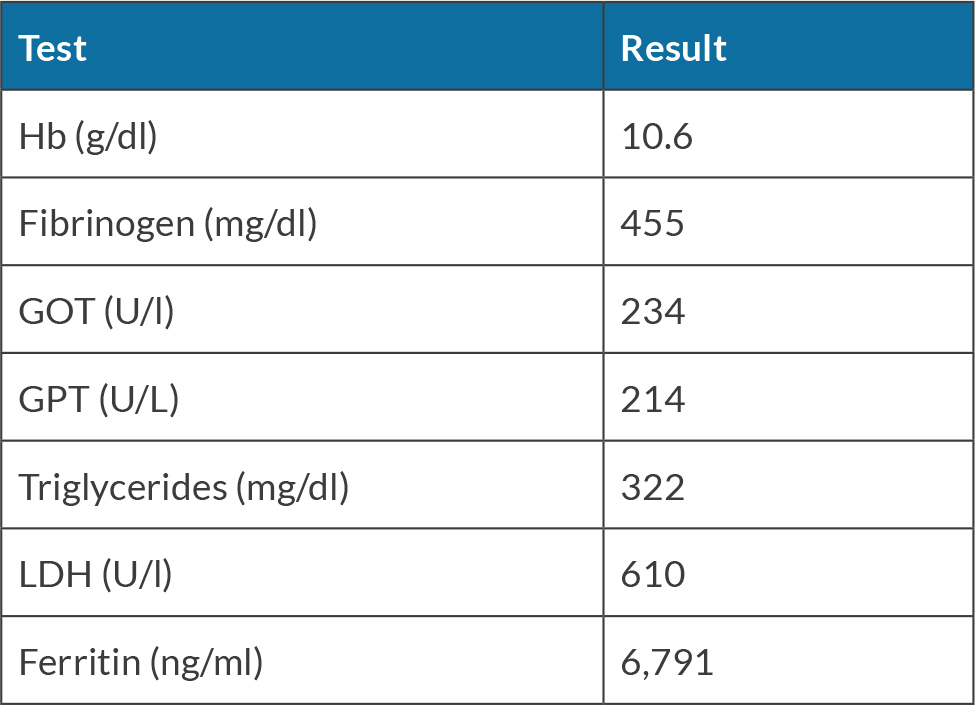
A 71-year-old man was admitted to our department because of intermittent fever above 38°C, arthralgia and the appearance of a necrotic lesion (Fig. 1) on his right arm for approximately 2 weeks, initially described as a wheal with two small incisions similar to an insect bite. The patient reported gardening two days before the onset of symptoms; however, no insect was seen on that occasion. He denied a relevant medical history and recent travel abroad. He reported a weight loss of 9 kg in the past month. He took amoxicillin/clavulanic acid for 12 days, then sulfamethoxazole/trimethoprim without clinical benefit. He went to the emergency room because of worsening symptoms: fever increased to 39°C and there was an extension of the injury. On admission to our department, the patient was not bedbound and was alert, oriented, haemodynamically stable (BP 130/70 mmHg, HR 92 bpm), eupnoeic in room air (SpO2 97%) and febrile (38.5°C). Antibiotic therapy with doxycycline was started. Several blood and urine cultures tested negative; a chest X-ray was negative. Blood serologies for infectious diseases, autoimmunity panel and major oncomarkers tested negative. A transthoracic echocardiogram was negative for endocarditis. The patient underwent a whole-body computed tomography (CT) scan, which documented multiple lymphadenomegalies of probable necrotic colliquative appearance, the largest one at the right axillary level, in a first hypothesis of reactive significance (Fig. 2). A shave/punch biopsy of the necrotic skin lesion was performed: culture tests were negative and histologic examination revealed non-specific necrotic material. Because of the lack of clinical benefit and the persistence of fever, antimicrobial therapy with cefepime, teicoplanin and itraconazole was administered, with no clinical/laboratory benefit. Given the persistence of fever and the negativity of all microbiological tests performed to date, antimicrobial therapy was discontinued, and a new skin and lymph node biopsy and bone marrow aspirate (negative for Leishmania spp. and Mycobacterium spp.) were performed (Fig. 3). Given the progressive anaemia, elevation of C-reactive protein and transaminases that suggested a systemic inflammatory response, blood tests for ferritin, triglycerides and fibrinogen were performed, confirming MAS (Table 1). An osteo-medular biopsy was diagnostic for haemophagocytosis[6]. The case was discussed with the FUO specialist, who made the diagnosis of cutaneous and systemic loxoscelism complicated by MAS based on blood tests, with the exclusion of ongoing infectious diseases, rheumatologic pathologies and active neoplastic pathologies[4]. Intravenous corticosteroid therapy was started with progressive reduction of inflammatory indices and disappearance of fever. The patient was then discharged home, with oral corticosteroid therapy and histologic examinations of the skin and axillary lymph node biopsy still in progress.
Days after discharge, the results of the second skin biopsy showed a lymphoid infiltrate with a diffuse growth pattern composed of anaplastic elements, with prominent nucleoli, atypical mitotic figures and extensive areas of necrosis. The immunohistochemical profile was CD3+/-; CD5-; CD30+; CD20-; PAX5-; CD34-; CD56-; ALK-; TdT-; BCL2-; c-MYC+ (>40%); CD8-; CD4+/-. The proliferative index was 95%. These morphological and immunophenotypic findings were consistent with primary cutaneous anaplastic large cell lymphoma (PC-ALCL). Lymph node biopsy findings were also consistent with lymph node involvement by PC-ALCL.
DISCUSSION
Lymphoma is characterised by abnormal lymphocytes that lose control of their own replication and proliferate, forming a primitive solid mass. It is characterised by nodal or extranodal localisation and can be distinguished into primary and secondary. In particular, we will focus on the subtype of PC-ALCL, which was the definitive diagnosis based on histologic examination of the nodular skin lesion. Epidemiologically, CD30+ primary cutaneous T-cell lymphoproliferative disorders represent the second most common type of cutaneous T-cell lymphoma[7]. The median age at diagnosis is 60 years, with a slight predominance of males and Caucasians. Tumour nodules can present as single or clustered, growing over weeks or months, with a tendency to ulcerate[8].
The definitive diagnosis is determined by microscopic morphological and immunohistochemical examination. The tissue biopsy can be an excisional, incisional or punch biopsy, and the histologic examination should reflect the profile described above. Locoregional lymph nodes should also be examined histologically, as they could be of a reactive nature. Radiotherapy is recommended for skin lesions with locoregional lymph node involvement[9]. Brentuximab vedotin is the preferred therapy in cases of diffuse systemic lymph node and/or visceral involvement[10]. Involvement of lymph nodes proximal and adjacent to the skin lesion does not necessarily correlate with prognosis, whereas diffused disease is indicative of a poor prognosis.
CONCLUSIONS
Skin lesions and lymphadenomegalies of unknown origin should always be biopsied. It is very common to obtain inconclusive results initially, but this does not justify not repeating the procedure to avoid misdiagnosis; in our patient, it was necessary to repeat biopsies to reach a definitive diagnosis.