ABSTRACT
Background: Hydrophilic polymer gel coatings are used on different intravascular devices to prevent vasospasm and thrombosis. However, it may become dislodged from these devices, leading to ischaemic complications in various organs including the skin, kidneys, brain, heart or lungs. Hydrophilic polymer embolisation (HPE) is a rare complication following endovascular procedures that is currently not fully recognised. The current knowledge of this phenomenon is based on reports consisting of histologic evidence of foreign polymers in the affected organ.
Case description: A 76-year-old male with a history of hypertension, type 2 diabetes, renal cell carcinoma and chronic kidney disease underwent endovascular stenting of the superficial femoral artery due to critical limb ischaemia of the right foot. The patient had an acute kidney injury following the procedure. Upon examining the legs, there were tender non-blanching macular lesions on the right lower limb. A skin biopsy of the lesion was performed and showed hydrophilic polymer embolisation. Unfortunately, a few weeks later the patient was readmitted due to a worsening of the right foot wound situation, which required below-knee amputation.
Conclusion: HPE is a rarely reported complication after endovascular interventions, with the potential to embolise to multiple organs. By observing skin manifestations, it is possible to aid the early detection of ischaemic events in other organs and identify their underlying causes. Generally speaking, the course is benign and self-limiting when the skin is involved, but may be more sinister especially when other organs (e.g. brain) are involved.
LEARNING POINTS
- Meticulous skin examination is an essential part of the diagnostic armamentarium of an internist, aiding in formulating a differential diagnosis based on such findings.
- Hydrophilic polymer embolisation (HPE) is a rarely reported complication after endovascular procedures.
- Given the potentially attenuated histological findings of HPE, history details of recent endovascular intervention are key to the diagnosis.
KEYWORDS
Hydrophilic polymer embolisation, endovascular procedure
INTRODUCTION
Endovascular stenting has largely replaced open surgical repair in cases of critical limb ischaemia. This may be done using either coated or 'bare-metal' stents. Hydrophilic polymer coating of endovascular devices decreases the risk of endothelial trauma[1]. Hydrophilic polymer embolism (HPE) may rarely complicate endovascular procedures, whereby there is a dissociation of coating material with distal embolisation reported to multiple organs including lungs, heart, brain, and skin[2]. In this case, we describe a case of cutaneous manifestation of HPE in a patient undergoing endovascular stenting for treatment of critical limb ischaemia.
CASE DESCRIPTION
A 76-year-old male with a history of smoking, hypertension, type 2 diabetes, renal cell carcinoma with skeletal metastasis treated with tyrosine kinase inhibitors, chronic kidney disease (eGFR ≈ 25–30 ml/min) and critical limb ischaemia of the right foot was admitted. He was to undergo endovascular stenting of the superficial femoral artery to aid in wound healing and pain management, alongside treatment of wound infection with antibiotics. The procedure was technically successful albeit described as complicated due to difficult access. However, following the procedure, the patient's creatinine increased steadily from baseline (153 µmol/l 1 day before the procedure to 235 µmol/l at day 6). There was no eosinophilia and the patient was afebrile. Renal consultation was requested.
The patient seemed to be clinically euvolemic with no signs of fluid overload. Upon examining the legs, macular lesions were found, which were only present on the right lower limb (Fig. 1). These were painful on palpation, and non-blanching. Pain was, however, also elicited when palpating the adjacent skin where lesions were absent. No other such lesions were seen elsewhere on inspection of the upper limbs and the torso. Given these lesions, a urinalysis was requested alongside a dermatology consultation to assess the presence of cholesterol-embolisation syndrome, which would explain both the renal dysfunction and the skin lesions.
Figure 1. Macular, punctate lesions on the anterior aspect of the stented lower limb.
Urinalysis showed multiple short granular casts which would suggest tubular necrosis, without eosinophiluria. The patient's creatinine levels started decreasing day 7 post-procedure, returning to baseline at around day 10 after the procedure, and were therefore deemed to be related to transient contrast-induced nephropathy. Cholesterol embolisation could not be entirely excluded though, given the absence of eosinophilia and fever, alongside the spontaneous improvement of renal function. Further investigations, including a renal biopsy, were therefore regarded as unnecessary.
The dermatology consultant performed a 3 mm punch biopsy of a lesion, 7 days after the endovascular procedure.
RESULTS
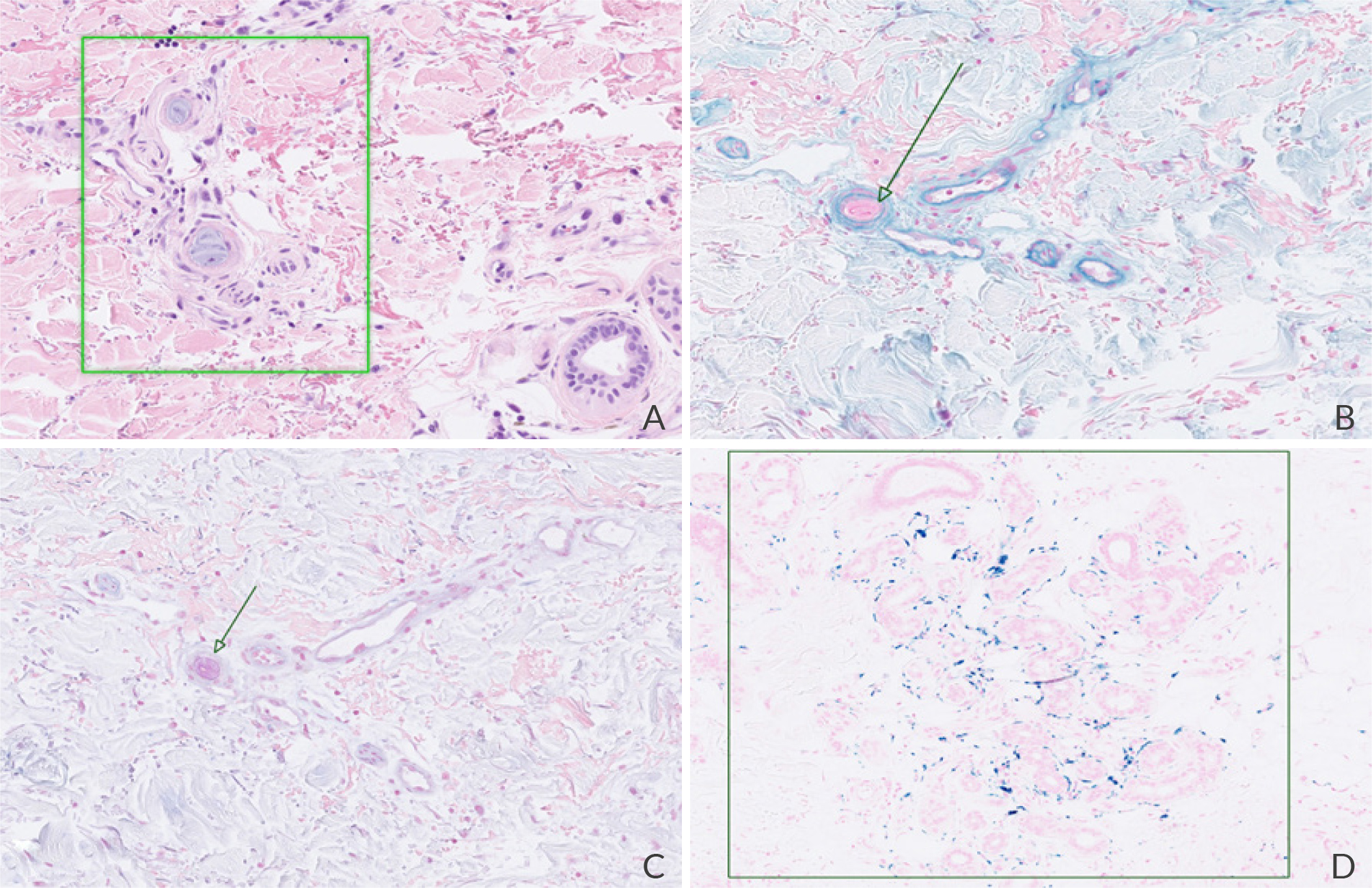
The skin biopsy report showed dermal structures containing amorphous, basophilic lamellar material inside blood vessels; no cholesterol emboli were found in the specimen (Fig. 2). The patient's history of recent endovascular manipulation with stent placement, alongside the histological picture, were both suggestive of HPE. A few weeks later, the patient was readmitted due to a worsening wound at the foot level requiring below-knee amputation. The skin lesions themselves had spontaneously resolved.
Figure 2. Dermis with few vascular structures, with intravascular amorphous, basophilic lamellar material (A, haematoxylin-eosin stain ×13). The intravascular material is non-birefringent in polarised light and is negative for Hale stain (B, ×13) and Alcian blue stain (C, ×13). There were, however, multiple siderophages surrounding the sudoriferous glands, which were positive on iron stain (D, ×10). Altogether, these findings were suggestive of hydrophilic polymer embolisation.
DISCUSSION
HPE is a rarely reported complication of endovascular procedures[3], whereby outcomes depend on the affected organ, ranging from spontaneous resolution to death due to occlusion of vessels in vital organs. The exact mechanism by which polymer material embolises is uncertain, but it involves several factors including irregularity of the endothelial wall, whereby the hydrophilic material 'sheds off' downstream. This has been shown to be commonly occurring even for in vitro models[4].
The majority of HPE cases reported in literature seem to occur within a few hours to days after endovascular intervention and may present as a petechial, or purpura rash. In our case, the skin rash was only found serendipitously upon clinical examination to assess for causes of renal dysfunction after the endovascular procedure, as the patient was asymptomatic from it (unless pressure was applied to the area). This was likely due to underlying diabetic neuropathy and pain from the underlying infected foot ulcers. This case highlights the importance of a thorough examination of the skin and to include it as routine, even when performing a consultation.
The histological findings in our case were scarce given the low number of vessels in which the polymer material was identified and the time period (almost 1 week after the procedure) during which the skin biopsy was undertaken. This is not uncommon[5] given that the polymer material is – over time – readily biodegradable. In addition to this, it is not entirely possible to exclude HPE to the kidneys as a cause of the post-procedural, and transient, worsening renal function. This would have required a renal biopsy to confirm which, given the patient's comorbidities and spontaneous resolution, was deemed unjustified. A high index of suspicion is therefore required to identify the diagnosis. There is no specific therapy for the treatment of HPE, and supportive measures may be instituted depending on the affected organ.
CONCLUSION
HPE is a rarely reported complication after endovascular interventions, with the potential to embolise to multiple organs including the skin. Generally speaking, the course is benign and self-limiting, but may, however, be more sinister especially when other organs (e.g. brain) are involved.