ABSTRACT
Introduction: The differential diagnosis of focal biliary strictures comprises both malignant and benign conditions. We report a rare case of follicular cholangitis presenting with segmental stricture of the left hepatic duct.
Case description: An asymptomatic 59-year-old male with no past medical history presented with dilation of the left intrahepatic bile ducts revealed as an incidental finding on an abdominal ultrasound. Blood examinations showed only a slightly elevated γ- glutamyl transferase (γGT) value, while carbohydrate antigen 19-9 (Ca 19-9) and serum immunoglobulin G4 (IgG4) were within normal range. Abdominal computed tomography and magnetic resonance imaging/magnetic resonance cholangiopancreatography (MRI/MRCP) scans revealed a high grade focal intrahepatic stricture of the left hepatic duct (FIHS type III) with proximal dilatation. Given that a diagnosis of cholangiocarcinoma could not be ruled out, the patient was referred for a left hepatectomy with regional lymph node dissection. Histological analysis showed a lymphoplasmacytic infiltration of the left hepatic duct with fibrosis and follicle formations in the submucosa, findings consistent with follicular cholangitis. The postoperative course was uneventful and there is no evidence of recurrence 8 months after the surgery.
Discussion: The clinical and imaging presentation of follicular cholangitis is very similar to cholangiocarcinoma, rendering it a challenging diagnosis preoperatively.
Conclusion: The approach to these cases should be primarily surgical. Even though it is very rare -- our report is the 13th case reported worldwide -- follicular cholangitis should be included in the differential diagnosis of focal biliary strictures.
LEARNING POINTS
- The differential diagnosis of biliary strictures comprises malignancies, like cholangiocarcinoma, as well as benign conditions.
- It is very challenging to distinguish between malignant and benign biliary strictures preoperatively, so the most reliable treatment approach to these cases is often surgical.
- Follicular cholangitis is a very rare condition and more data is needed to better understand disease pathophysiology, management, recurrence rates, and possible alternatives to surgery.
KEYWORDS
Follicular cholangitis, biliary strictures, cholangiocarcinoma
INTRODUCTION
The differential diagnosis of focal biliary strictures comprises both malignant and benign conditions[1]. Although the majority of cases are attributed to cholangiocarcinoma, about 16% of strictures turn out to be benign after surgical resection[1]. Primary sclerosing cholangitis (PSC), IgG4 sclerosing cholangitis, other inflammatory and infectious cholangiopathies, ischemic or iatrogenic strictures are some of the conditions mimicking cholangiocarcinoma, making a preoperative diagnosis challenging[1]. Follicular cholangitis is a rare benign entity with similar clinical and radiological presentation to cholangiocarcinoma[2]. It is characterized by lymphoplasmacytic infiltration of the bile ducts, fibrosis and follicle formation with germline centers in the submucosa[3].
We hereby report on a case of follicular cholangitis presenting with focal stricture of the left hepatic duct.
CASE DESCRIPTION
An asymptomatic 59-year-old male patient was referred to our hospital for further investigation of dilation of the left intrahepatic bile ducts, shown in an outpatient upper abdominal ultrasound. The patient denied any fever, abdominal pain, pruritus, dark urine, bowel movement alterations or weight loss. Clinical examination was unremarkable. He had no past medical history or significant family history. He was a past smoker and consumed alcohol socially. Blood examinations showed only a slight elevation of γ-glutamyl transferase (γ-GT= 69 IU/l), while the other hepatobiliary enzymes, tumor markers including carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (Ca 19-9), as well as serum immunoglobulin G4 (IgG4) were within normal range.
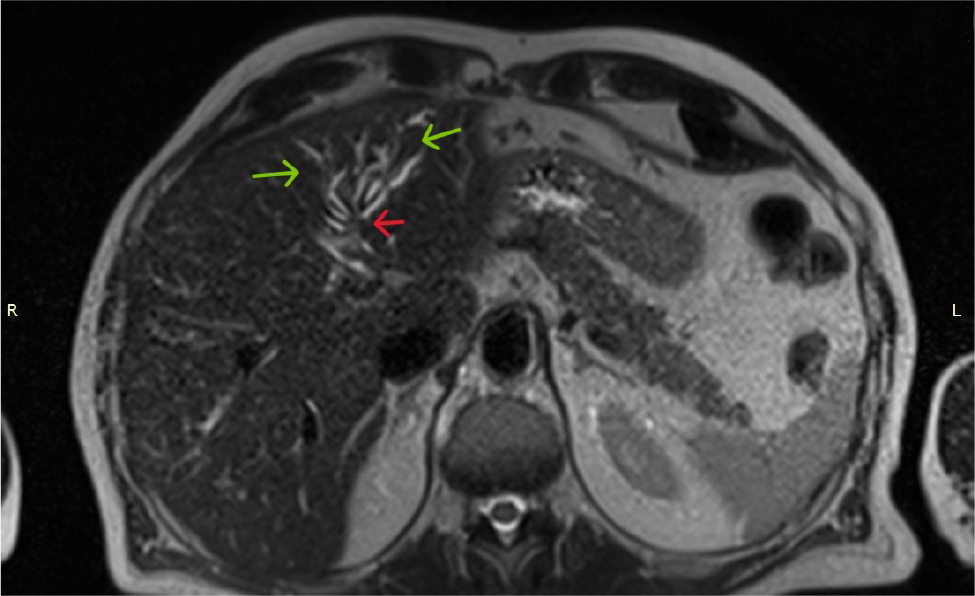
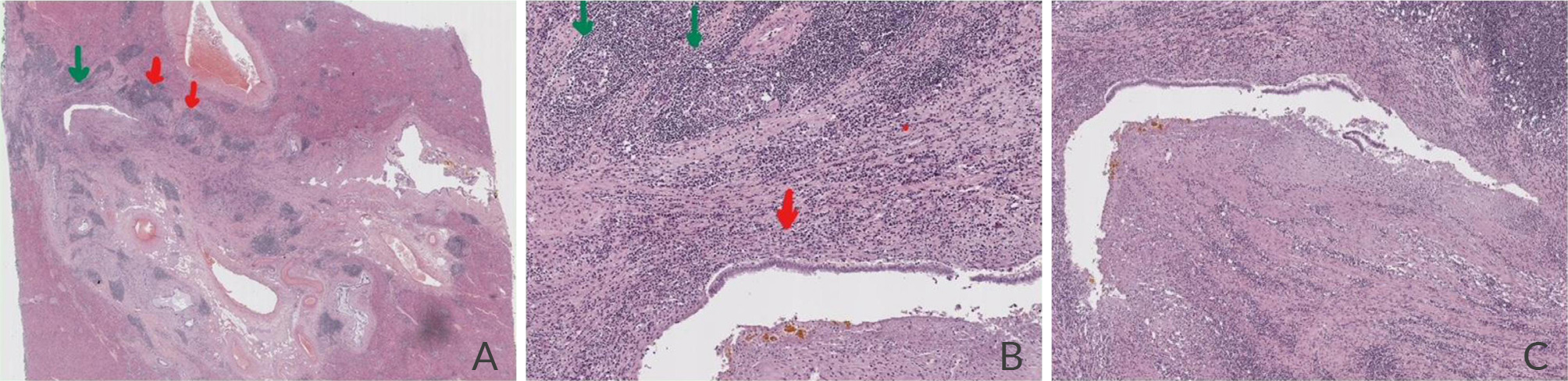
Further imaging with abdominal computed tomography (CT) and magnetic resonance imaging/magnetic resonance cholangiopancreatography (MRI/MRCP) revealed a high grade focal intrahepatic stricture of the left hepatic duct (FIHS type III) with proximal dilatation of the left intrahepatic biliary tree. Choledocholithiasis was excluded and the pancreas was normal (Fig. 1). Based on the radiological findings, the suspicion of hilar cholangiocarcinoma could not be excluded, therefore a left hepatectomy with regional lymph node dissection was performed. In the surgical specimen, the left hepatic duct wall and the surrounding tissue were significantly thickened, leading to the stricture, but there was no mass-like lesion. Macroscopically, a stellate, whitish, elastic area measuring 3 x 1 x 1 cm was noted (Fig. 2).
Microscopy showed lymphoplasmacytic infiltration of the left hepatic duct wall, non-concentric fibrosis of the submucosal connective tissue and several follicles with germline center formations (Fig. 3). Immunohistochemistry was positive for CD3, CD20, CD23 and CD5/PAX5. Additionally, reactive lymphadenitis was found and no signs of malignancy were present. The aforementioned findings were consistent with the diagnosis of follicular cholangitis.
The postoperative course was uneventful and there is no evidence of disease recurrence during 8 months of follow up.
Figure 1. MRI of a focal intrahepatic stricture of the left hepatic duct (FIHS III) (red arrow) with proximal dilatation of the left intrahepatic biliary tree (green arrows).
Figure 2. Cross-section of the resected specimen of the left hemiliver (weight = 371 g), revealing a stellate, whitish, elastic lesion (dimensions: 3 x 1 x 1 cm) around the intrahepatic bile ducts (black arrow).
Figure 3. Digital photos from a tissue slide after haematoxylin and eosin staining: A. Panoramic image of the resected lesion, in correspondence with the macroscopic image reported in Figure 2. The left intrahepatic duct (green arrow) shows focal stricturing, inflammatory infiltration and focal erosions. Fibrotic non-concentric thickening of the surrounding connective tissue and dense regional infiltration by lymphocytes, plasmatocytes, eosinophils and neutrophils is observed. There are several lymph follicles with prominent germline centers (red arrows). B. Higher magnification of the same area, showing lymph follicles with germline center formation (green arrows) and inflammatory infiltration of the duct wall (red arrow). C. Higher still magnification of the same area, showing slit-like stenosis and inflammatory infiltration of the left hepatic duct.
DISCUSSION
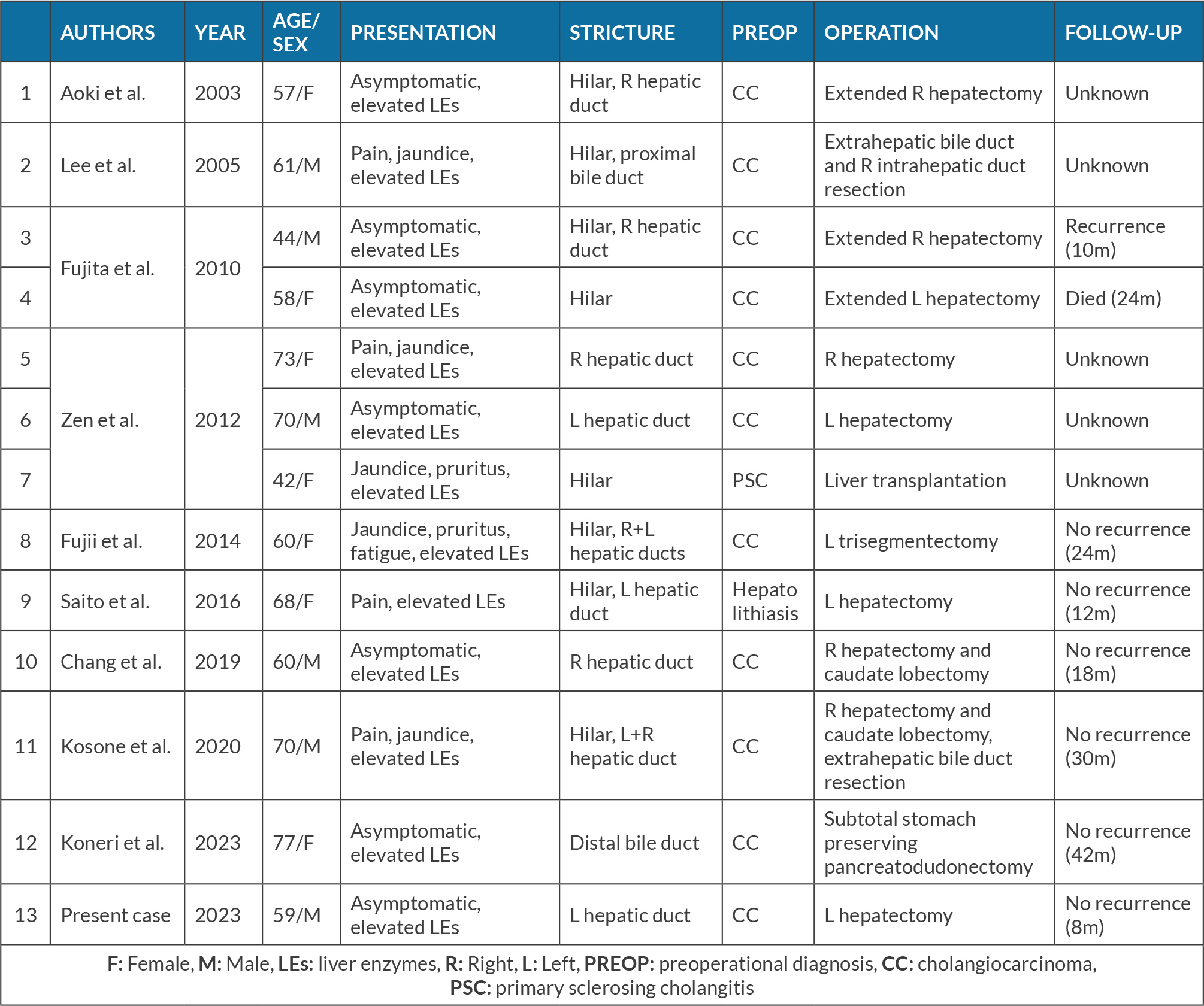
Follicular cholangitis is a rare cause of benign biliary stricture which is difficult to differentiate preoperatively from other benign conditions and cholangiocarcinoma. It was first described by Aoki et al. in 2003[4] and our case represents the 13th case described in the literature. A short review of the published data is shown in Table 1[2–10].
Table 1. Review of the published case reports with the diagnosis of follicular cholangitis.
Middle-aged men and women with no autoimmune background are mostly affected[2]. Seven cases, including ours, did not present any symptoms[2–4,8,10], while five cases presented with jaundice and cholestasis-related symptoms[3,5,6,9]. There was some degree of liver enzyme abnormality in all cases, but only two patients had elevated Ca 19-9 values, which can possibly be attributed to elevated bilirubin levels[3,10]. Imaging with CT, MRI/MRCP or endoscopic retrograde cholangiopancreatography (ERCP) was performed in all cases and all the biliary strictures were located around the hepatic hilum, with the exception of the most recent case reported, in which the stricture was located in the middle and distal bile duct[10]. One case was positive on 18F-FDG-PET/CT scan, making the preoperative exclusion of malignancy even more difficult[9]. After the diagnosis of follicular cholangitis was made, the scan results could be explained by the increased uptake of glucose in the lesion due to inflammation[9].
Surgery was performed in all reported cases with a presumed diagnosis of cholangiocarcinoma, apart from two cases: one suspicion of primary sclerosing cholangitis[3] and one case of recurrent hepatolithiasis[7]. There was no specific pattern of stricture, but Koneri et al. described overlapping leaf-like folds in the resected specimen, as a novel and potentially useful finding[10]. As far as other treatment options are concerned, a moderate benefit was reported in one case treated with corticosteroids[2] and a case of surgery after 8 years of close surveillance, demonstrating that a conservative approach could be considered[7]. Even though the evidence is limited, only one patient experienced recurrence of follicular cholangitis and one died in the two years following the operation[2].
The most reliable way to distinguish follicular cholangitis from other causes of biliary strictures is the microscopic examination of the surgical specimen, since no other clinical or radiological finding alone is pathognomonic[2]. Pathology results indicate inflammatory infiltration of the affected bile duct wall and dense non-concentric fibrosis with reactive hyperplastic follicles and prominent germline centers under the mucosa[3]. IgG4 positive cells are very scarce[6] and there is no obliterative phlebitis, excluding other autoimmune benign causes of biliary stenosis[8]. Immunohistochemistry is also useful in confirming the benign nature of the bcl-2 negative follicles, which contain both T (CD3 positive) and B cells (CD20 positive)[2,3,6].
The inability to differentiate malignant from benign biliary strictures preoperatively leads to surgical management in many cases. Indeed, there is no diagnostic modality specific enough to change the current management of the condition[1]. More data and case series are needed to investigate the potential place of corticosteroids in non-invasive management and close surveillance of disease progression, as alternatives to surgery[2,7]. A reliable test to rule out malignancy, instead of the neither sensitive nor specific brush cytology, and the development of new imaging techniques and biomarkers to differentiate malignant disease from the various benign conditions[2] may potentially provide a better and more personalized management of cases of follicular cholangitis in the future.
CONCLUSIONS
The clinical and imaging findings of follicular cholangitis are almost indistinguishable from those of cholangiocarcinoma, so the main treatment for both malignant and benign focal biliary strictures is surgical resection. Despite its rarity, follicular cholangitis should be part of the diagnostic approach to localized biliary stricture.