ABSTRACT
Introduction: Porto-sinusoidal vascular syndrome is characterised by specific histological changes that do not include cirrhosis, with or without portal hypertension. Patients are usually asymptomatic until development of portal hypertension complications.
Case description: A 69-year-old female with history of JAK2 positive essential thrombocythemia (ET) was referred to internal medicine consultation due to elevated liver enzymes. The patient had no previous history of liver disease. Seven months earlier, she had an ischaemic stroke and started treatment with atorvastatin. After discontinuing medication, liver enzymes returned to normal and atorvastatin-related drug-induced liver disease (DILI) was presumed.
During a follow-up visit, iron deficiency anaemia was detected and an endoscopic study was performed. It revealed a gastric varix actively bleeding, which was successfully treated with cyanoacrylate.
Two months later, the patient was admitted due to a new episode of variceal bleeding, and a portal hypertension complementary study was made.
Discussion: Although the pathogenesis of porto-sinusoidal vascular disease (PSVD) remains poorly understood, vascular changes within the liver have been associated with several predisposing conditions, such as hypercoagulable states. Patients with ET, especially those with JAK2 mutation, are known to be at increased risk of non-cirrhotic vein thrombosis. Concerning PSVD, the association is not clear but it is believed that both PSVD and myeloproliferative neoplasms share a common denominator: a state characterised by hypercoagulability, inflammation, endothelial dysfunction and, in some cases, portal hypertension.
Conclusion: Portal hypertension without cirrhosis is a rare condition, presenting diagnostic challenges and significant impact on the patient’s prognosis.
LEARNING POINTS
- The suspicion of PSVD should be raised when signs of portal hypertension are present with normal or mildly elevated liver enzymes and normal liver stiffness measurement. A liver biopsy should be performed in this situation.
- Although the pathogenesis of PSVD is not clearly understood, it is based on the development of vascular changes within the liver and there might be several predisposing conditions such as coagulation disorders.
KEYWORDS
Porto-sinusoidal vascular disease, portal hypertension, incomplete septal fibrosis
INTRODUCTION
Porto-sinusoidal vascular disease (PSVD) combines several conditions characterised by a process that primarily affects the hepatic sinusoids and portal venules[1]. The diagnosis of PSVD requires a liver biopsy excluding liver cirrhosis and the presence of specific signs of portal hypertension, or one specific histological lesion: obliterative portal venopathy, nodular regenerative hyperplasia or incomplete septal fibrosis[1-3]. The presence of gastric, oesophageal or ectopic varices, portal hypertensive bleeding or porto-systemic collaterals at imaging are considered specific signs of portal hypertension. In the absence of a specific histological lesion or a specific sign of portal hypertension, the diagnosis of PSVD requires both a non-specific sign of portal hypertension (ascites, platelet count <150,000/mm3, spleen size >13 cm in the largest axis) and a non-specific histological lesion sign of PSVD (portal tract abnormalities, architectural disturbance, non-zonal sinusoidal dilatation and mild perisinusoidal fibrosis)[1,3]. These patients are usually asymptomatic until they develop complications of portal hypertension. Liver enzymes are usually normal or mildly elevated, and the liver function is preserved[2-4]. Liver and spleen stiffness and the measurement of hepatic venous pressure gradient (HVPG) do not establish a diagnosis, but can be useful; unlike in cirrhosis, expected values are HVPG < 10 mmHg and liver stiffness measure (LSM) < 10 kPa. However, spleen stiffness measurement is typically markedly increased. The clinical course seems to be more favourable than in patients with liver cirrhosis[2-4].
This is a case of a 69-year-old female with PSVD.
CASE DESCRIPTION
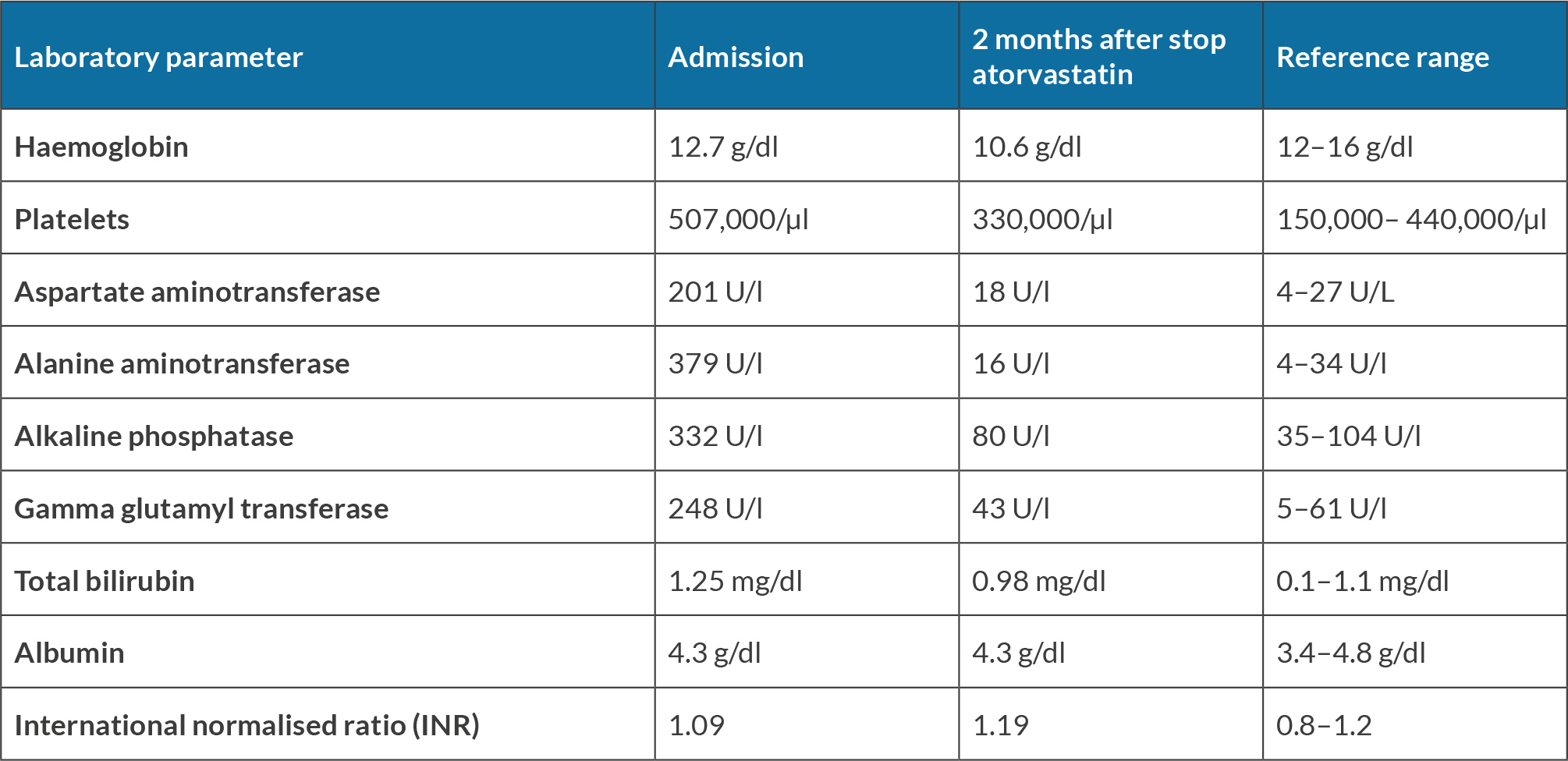
A 69-year-old female with a history of JAK2 positive essential thrombocythemia (ET) was referred to Internal Medicine consultation due to elevated liver enzymes (Table 1).
The patient had no history of regular use of alcohol or recreational drugs. Seven months earlier, she suffered an ischaemic stroke and started treatment with atorvastatin. Physical examination was normal. Viral hepatitis, autoimmune liver diseases and metabolic liver diseases were excluded. Atorvastatin was discontinued and, 2 months later, liver enzymes returned to normal (Table 1). Atorvastatin drug-induced liver disease (DILI) was presumed.
Table 1. Laboratory parameters in consultation at admission and 2 months after stopping atorvastatin
During a follow-up visit, iron deficiency anaemia was detected, with a drop in haemoglobin levels from 10.6 to 7.3 g/dl. An endoscopic study was performed, revealing an actively bleeding gastric varix successfully treated with cyanoacrylate glue. The patient was admitted, treat with terlipressin and ceftriaxone, and discharged 6 days later.
Two months later, she was readmitted due to another episode of variceal bleeding. The subsequent endoscopy study revealed, once again, an actively bleeding gastric varix.
An angio CT scan was performed and showed a liver with normal dimensions and a homogeneous texture; suprahepatic veins and portal vein were patent with preserved calibre; venous collaterals were observed, particularly prominent at the gastric fundus, as well as marked homogeneous splenomegaly, 16 cm. A subsequent magnetic resonance imaging (MRI) allowed the diagnosis of splenic vein thrombosis.
Considering the suggested findings of portal hypertension, an LSM and a transjugular liver biopsy with portal vein catheterisation were performed. The LSM was 4.7 kPa (IQR 9%) and the HVPG was <10 mmHg. Histological findings demonstrated mild chronic hepatitis lesions with incomplete portal and septal fibrosis. No evidence of cirrhotic change of the liver was found.
After a diagnosis of a PSVD was established, the patient continued treatment with carvedilol and started apixaban due to occlusion of the splenic vein. The patient remains under follow-up and no episodes of decompensation have been recorded.
DISCUSSION
Although the pathogenesis of PSVD is unknown, it is based on the development of vascular changes within the liver and it is believed that there are several predisposing conditions[5]. It has been associated with drug exposure, immune disorders or autoimmune diseases, coagulation disorders, infections and hereditary diseases[2]. In ET, the presence of JAK2 V617F has been associated with an increased risk of thrombosis and the association with non-cirrhotic vein thrombosis has been clearly established[2,6]. Several pathophysiologic aspects contribute to thrombotic tendency: there is an increased production of blood cells – including platelets – which can lead to an increased risk of blood clot formation, including splenic vein thrombosis. It can induce changes in plasmatic coagulation, vessel wall, and cell adhesion and function[7]. In PSVD, the relationship between PSVD and JAK2 positive ET is not clear, but the presence of hypercoagulability may induce sinusoidal vascular changes. Beside that, the JAK2 mutation induces endothelial dysfunction, which can contribute to thrombotic events and affect vascular health[7]. Endothelial dysfunction may play a role in the development of both splenic vein thrombosis and PSVD.
CONCLUSION
Portal hypertension without cirrhosis is a rare condition with a challenging diagnosis and impact on the prognosis. Although this case reports a typical course of investigation and diagnosis of PSVD, the pathophysiology that relates this condition to myeloproliferative neoplasms is not well understood and, to the best of our knowledge, has not been previously described in the literature. The authors’ aim is to raise awareness of the potential link between these conditions, allowing for early diagnosis and intervention, and preventing the development of complications.