ABSTRACT
Introduction: Mucormycosis, a rare and life-threatening infection, is caused by microorganisms of the Mucorales order. It affects almost exclusively immunocompromised and diabetic patients, requiring extensive surgical debridement and prolonged antifungal therapy.
Discussion/Results: We report the case of a 26-year-old immunocompetent woman, presenting with cutaneous mucormycosis after suffering blunt force trauma. This rare occurrence of mucormycosis in an immunocompetent patient reinforces the importance of elevated clinical suspicion and early initiation of adequate surgical and antifungal treatment.
Conclusion: Mucormycosis is a challenging condition with potentially devastating consequences. Timely diagnosis and appropriate management are vital to mitigate the morbidity and mortality associated with this condition.
LEARNING POINTS
- Cutaneous mucormycosis is a rare life-threatening infection that affects mainly immunocompromised patients.
- Certain circumstances warrant a high index of clinical suspicion in immunocompetent patients, and indicate histopathological examination.
- Treatment involves a multidisciplinary approach with aggressive surgical debridement, antifungal therapy, and elimination of risk factors.
KEYWORDS
Cutaneous mucormycosis, soft tissue, fasciitis, trauma
INTRODUCTION
Necrotizing fasciitis (NF) is a rare and acute infectious disease that involves the skin, subcutaneous tissue and fascia. It causes tissue necrosis and is frequently associated with systemic toxicity[1,2]. NF can be a monomicrobial or polymicrobial disease. The most common etiological agents are bacteria such as Streptococcus pyogenes, however it can also be caused by fungi like those of the Mucorales order[3-5]. They cause a rare and opportunistic fungal infection, named primary cutaneous mucormycosis[4,5]. Mucormycosis mostly affects immunocompromised hosts, and produces serious lesions with cutaneous necrosis, thrombosis and vascular invasion leading to systemic infection and a poor prognosis[4,5]. Tissue examination by histopathology and culture confirms the fungal infection[4,5]. Treatment includes antifungal therapies and surgical debridement[4,5]. With our clinical report, we would like to emphasize that necrotizing fasciitis can also happen in immunocompetent people and that medical professionals should consider bacteria and fungi as possible etiological agents.
CLINICAL CASE
We report the case of a 26-year-old healthy woman with no history of diabetes mellitus. She was brought to the emergency department (ED) after suffering major blunt force trauma secondary to a high-speed motorcycle collision, which projected her into a nearby pasture where she was found 3 hours later.
Upon arrival in the ED, the patient presented with a Glasgow coma scale (GCS) of 3, hypotension (BP 74/65mmHg), tachycardia (HR 106 bpm), adequate oxygenation and ventilation measured by arterial blood gas analysis, blood glucose level of 92 mg/dl and lactate level of 6 mmol/l. She had been intubated and ventilated on site and transported immobilized with c-spine protection.
Her physical examination revealed signs of pelvic instability with a point of care ultrasound scan negative for free intraperitoneal fluid.
Full body computed tomography (CT) revealed a right maxillary sinus fracture, bilateral pulmonary contusion and an extraperitoneal bladder rupture together with an open book pelvic fracture.
The patient underwent pelvic stabilization using external fixators and was admitted to the Intensive Care Unit (ICU) with a diagnosis of polytrauma and hemorrhagic shock. She was started on prophylactic antibiotics with cefotaxime 1g every 8 hours.
On her third day of ICU admission, the patient became hemodynamically unstable, with a rise in her C-reactive protein (CRP) and an unexpected elevation of her pancreatic amylase and lipase contents. She remained afebrile and her initial cultures were negative. An abdominal and pelvic CT scan was performed which revealed pancreatic necrosis of 50% of the pancreas and a paralytic ileus. Her parenteral nutrition was immediately suspended, and she was started on supportive measures.
On the seventh day, the patient had a low-grade fever (temperature 38ºC) and continuous rise of CRP and leukocytosis. This prompted a repeat abdomen and pelvic CT scan, which showed no increase of the pancreatic necrosis or worsening of her extraperitoneal bladder rupture. Ceftazidime 1g was initiated empirically every 8 hours. Her cultures isolated Staphylococcus aureus in her tracheobronchial aspirate, as well as Escherichia coli in her urine, leading to the added diagnosis of pneumonia and urinary tract infection.
The patient's fever persisted and there was progressive worsening of her inflammatory markers. At this point we observed a right cervical hematoma with inflammatory signs and swelling. A maxillofacial CT scan was done, revealing an 8mm hypodense submental nodule (Fig. 1). We performed percutaneous drainage which showed a purulent discharge which was sent to the microbiology laboratory. Ceftazidime was stopped, and meropenem, clindamycin and vancomycin were initiated as prevention against methicillin-resistant S. aureus (MRSA) and gram-negative agents.
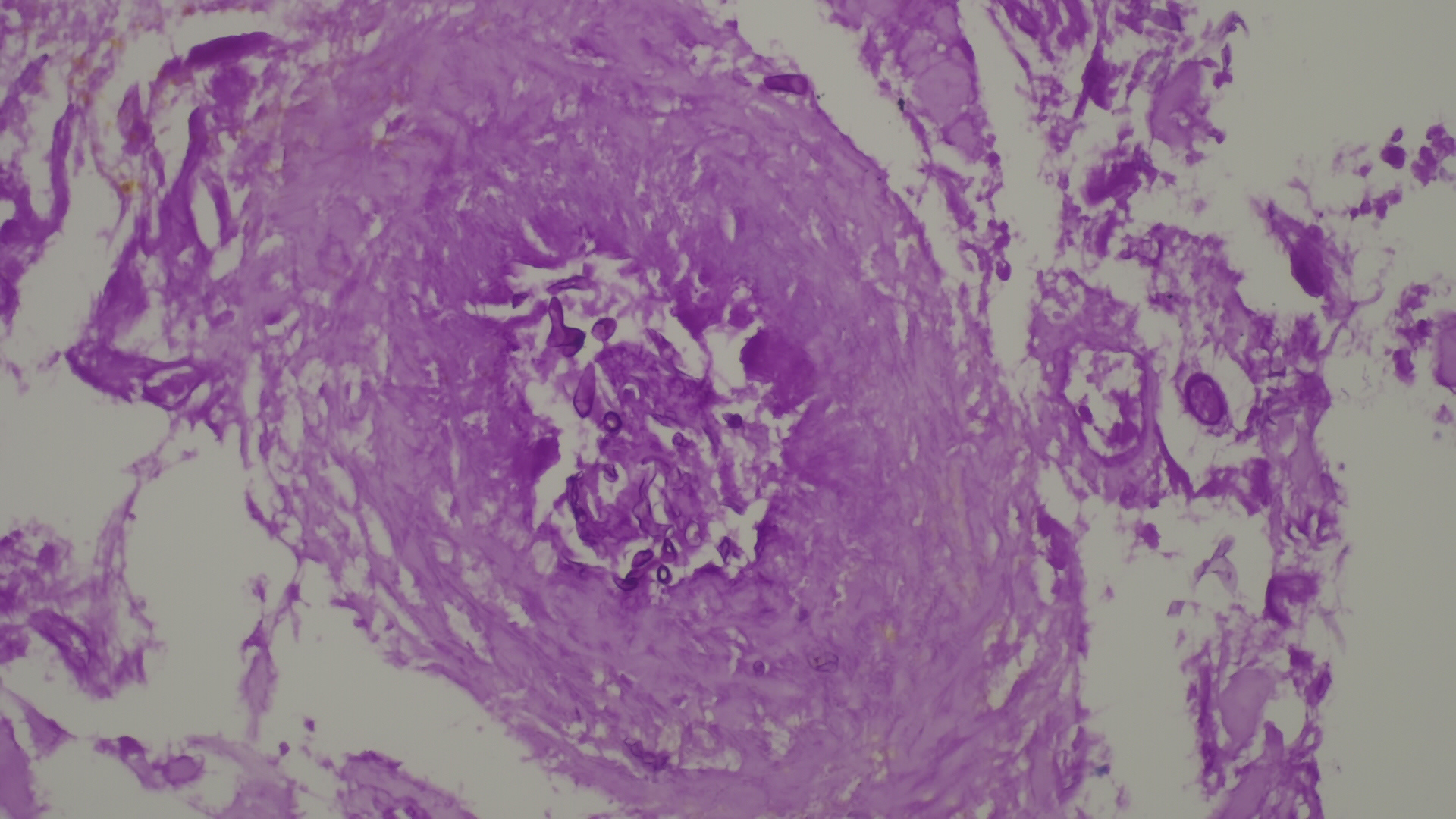
We were not able to control the infection with medical treatment, and on the thirteenth day of ICU admission, a repeat cervical CT scan showed extensive bilateral edematous infiltration of the subcutaneous fat of the submental region. The maxillofacial surgery department was consulted, leading to the differential diagnosis of cervical necrotizing fasciitis versus mucormycosis. Urgent extensive surgical debridement was performed (Fig. 2). Samples were sent once again to the microbiology and pathology lab and daptomycin was added to the ongoing antibiotic scheme, given evident signs of sepsis. Three days later, a microbiology report showed growth of filamentous fungi suggestive of a zygomycete, antibiotics were stopped, and amphotericin B was initiated. The diagnosis of mucormycosis was confirmed later by the pathology laboratory (Fig. 3).
After a month of inpatient treatment, with excellent clinical improvement, antifungal therapy was de-escalated to posaconazole 300 mg twice daily on the first day and 300 mg once daily from the second day onward. Given the fact that mucormycosis is rare in immunocompetent patients, an extensive serological panel was ordered, which was negative for HIV and Hepatitis C, and showed immunity to Hepatitis B virus due to previous vaccination. The patient was discharged two weeks later, given the excellent clinical response.
Figure 3. Periodic acid-Schiff (PAS) staining. Broad pauciseptate hyphae fungus with vascular invasion
DISCUSSION
Necrotizing soft tissue infections (NSTI) are rapidly progressive diseases characterized by necrosis of deep soft tissues[1,5]. The number of reported cases in adults is 0.40 cases per 100,000 people/year[2] and a higher incidence of 4-19% in immunocompetent patients[3]. The mortality rate is estimated at between 30-40%, increasing with a delayed diagnosis[3,4]. Necrotizing fasciitis is an uncommon surgical emergency that requires aggressive debridement[4,5].
The vast majority of NSTI are caused by bacteria, however studies have shown that fungi such as Mucorales are highly capable of infecting human hosts compared to other opportunistic molds[5]. Despite the high infectivity of Mucorales fungi, mucormycosis is rare and affects mainly immunocompromised patients[5].
Our patient presented with skin and soft tissue mucormycosis, which is a rare disease resulting from the inoculation of spores into the dermis[5]. It is almost always associated with trauma or wounds[4,5].
Although the diagnosis relies on the identification of organisms in tissues by histopathology with culture confirmation[5], a high index of clinical suspicion is warranted.
A multidisciplinary approach is mandatory for the treatment of mucormycosis, including surgical source control, antifungal therapy, and elimination of risk factors. Early initiation of antifungal therapy must be established, and intravenous amphotericin B is the drug of choice for initial therapy[4,5]. Despite significant advances in critical care management of mucormycosis, mortality remains high. Hyperbaric oxygen therapy has shown promising results when available but is used off-label and should not interfere with the standard treatment[1].
Looking back, we believe that the Mucor was present since the beginning of the infection, however, this was masked by other clinical problems associated with the major trauma experienced by the patient. This highlights the need for frequent assessment of the patient, as well as an elevated clinical suspicion for fungal infection, given the mechanism of injury.
CONCLUSION
Mucormycosis constitutes a challenging diagnosis that requires a high level of suspicion particularly in immunocompetent patients. Whenever faced with a rapidly progressive necrotizing fasciitis, one should consider a fungal origin. Histopathological analyses allow us to rapidly identify fungal structures in the damaged tissue and are a useful guide to initiate early treatment with an antifungal agent, hence improving the patient's prognosis.