ABSTRACT
This case report presents the management of a 53-year-old female with a complex psychiatric history who ingested multiple medications, resulting in severe cardiovascular compromise and subsequent respiratory failure. The patient’s ingestion included clonidine, fluoxetine, gabapentin, quetiapine and bupropion. Initial treatment involved supportive measures, including fluid resuscitation, bicarbonate infusion and correction of electrolyte imbalances. Despite these interventions, the patient remained haemodynamically unstable, requiring multiple vasopressors. Lipid emulsion therapy was initiated and led to a remarkable improvement in the patient’s cardiovascular status. However, she developed acute respiratory distress syndrome (ARDS) and required prolonged mechanical ventilation. Steroid therapy was initiated to manage the ARDS, and the patient was successfully extubated on day 6. The case highlights the potential effectiveness of lipid emulsion therapy in managing bupropion toxicity, but emphasises the need for further research to establish clear guidelines on dosing, timing and safety protocols. Adverse effects associated with lipid emulsion therapy must be carefully considered. Individualised decision-making and patient-centred care is crucial in optimising outcomes in cases of bupropion toxicity.
LEARNING POINTS
- Recognise the cardiotoxic effects of bupropion toxicity: be vigilant in identifying cardiotoxic effects such as prolonged QTc, hypotension and arrhythmias in cases of bupropion toxicity.
- Consideration of intravenous lipid emulsion therapy for toxic injections of lipophilic drugs such as bupropion: in severe lipophilic drug ingestions, such as bupropion, consider using intravenous lipid emulsion therapy as a potential treatment option.
- Individualised decision-making and monitoring is necessary when using lipid emulsion therapy: tailor treatment based on the patient’s condition and closely monitor for responses and potential adverse effects when using lipid emulsion therapy.
KEYWORDS
Bupropion toxicity, lipid emulsion therapy
CASE PRESENTATION
A 53-year-old female with a complex psychiatric history including generalised anxiety disorder, recurrent severe major depressive disorder, bipolar disorder, attention deficit hyperactivity disorder and chronic pain syndrome, presented to the emergency department after ingesting multiple medications.
She had ingested clonidine (~6 mg), fluoxetine (1.2 g), gabapentin (~9 g), quetiapine (~6 g) and bupropion (~13.5 g). The patient arrived from another medical facility requiring sedation and intubation due to recurrent seizures. Upon arrival, she received IV levetiracetam with no effect and was on midazolam infusion, along with phenobarbital.
She was admitted directly to the intensive care unit in our tertiary facility. Initially, she was on a norepinephrine drip to maintain mean arterial pressure at 65 mmHg; however, she quickly required multiple other pressors (vasopressin, epinephrine and phenylephrine) for further haemodynamic support. Physical examination revealed myoclonic movements, symmetrical pupils with minimal response, flaccid muscle tone, and normal cardiovascular and lung findings. Laboratory investigations revealed normocytic normochromic anaemia, mildly elevated creatine kinase, elevated lactate level and significant acidemia.
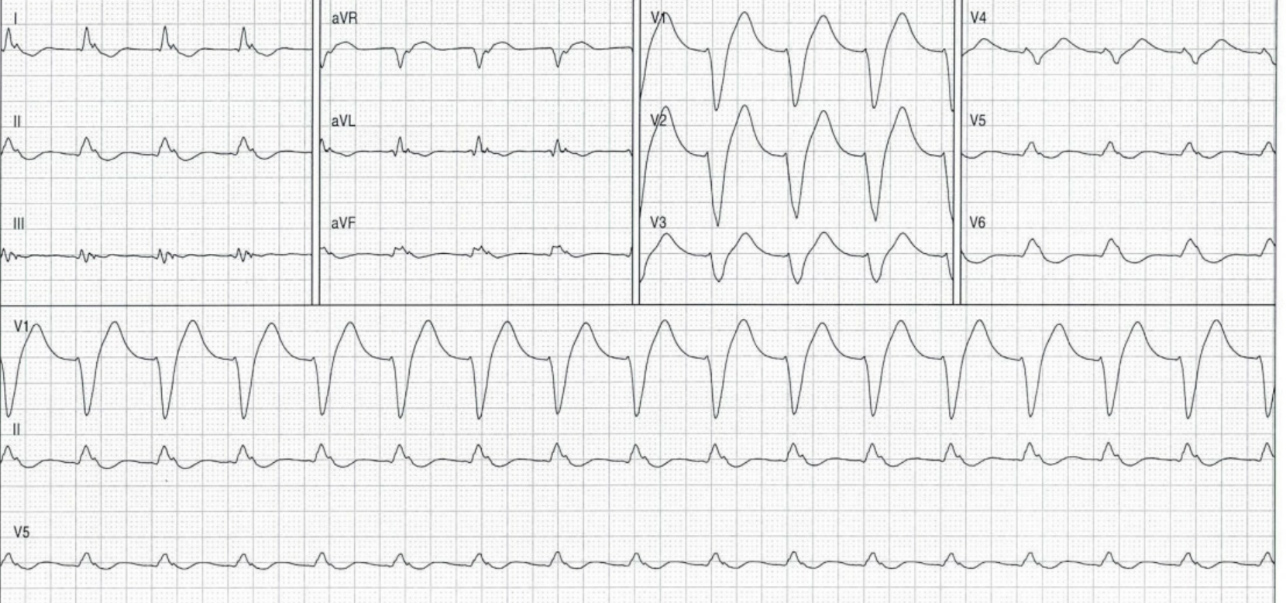
An electrocardiogram (EKG) showed a new junctional wide complex left bundle branch block with a prolonged QTc interval (Fig. 1). Transthoracic echocardiography demonstrated severely reduced biventricular systolic function, severe global hypokinesia of the left ventricular walls and an ejection fraction of 30%.
The patient was started on a bicarbonate infusion as maintenance fluid and to address acidemia. Additionally, she was given calcium and magnesium to help with the prolonged QTc and cyproheptadine for possible serotonin syndrome. Given her continued haemodynamic compromise, she was evaluated for veno-arterial extracorporeal membrane oxygenation. Unfortunately, she required an assessment of higher brain function, and that was challenging given that she was on midazolam infusion for sedation and seizure control.
The decision was made to initiate intravenous lipid emulsion therapy. By the end of day 1, the patient’s EKG showed a normal sinus rhythm with a normal QTc interval. On the following morning (day 2), there was an improvement in the patient’s blood pressure, and she no longer required any vasopressor support. A repeat transthoracic echocardiography performed on day 3 revealed normal biventricular systolic function, with an ejection fraction of 60%.
Unfortunately, the patient’s condition worsened as she developed type II respiratory failure, necessitating increased ventilation support. The patient needed to be paralysed and placed in a prone position. Subsequent chest X-rays showed progressive bilateral patchy infiltrates, raising suspicion for acute respiratory distress syndrome (ARDS). As a result, the patient was started on steroid therapy to manage the ARDS. Afterwards, on day 6, the patient was successfully extubated. While some behavioural concerns of agitation and nonsensical speech were observed, there was no evidence of other neurological dysfunction. She was transferred to the general medical floor and discharged to a psychiatric facility.
DISCUSSION
This case describes a patient with a complex psychiatric history who presented following the intentional ingestion of multiple medications. The patient exhibited severe cardiovascular compromise including hypotension, prolonged QTc and QRS intervals, and severely reduced biventricular systolic function. The initial management involved the administration of fluids, bicarbonate infusion, calcium and magnesium to address acidemia and correct the prolonged QTc interval. Despite these measures, the patient’s haemodynamic instability and EKG changes persisted, necessitating the use of multiple pressors for support and the initiation of lipid emulsion therapy. This led to a remarkable improvement in the patient’s cardiovascular status. However, her respiratory condition deteriorated, suggesting the development of ARDS and this prolonged the duration of mechanical ventilation. Consequently, the extubation process was delayed.
The intricacy of this case stems from the simultaneous ingestion of multiple medications, each with distinct mechanisms of action, pharmacokinetics and toxicity profiles. Among these, we identified severe bupropion toxicity as a significant contributor to the patient’s presentation. Bupropion is an atypical antidepressant classified as a norepinephrine-dopamine reuptake inhibitor (NRDI). It has a narrow therapeutic index, typically prescribed within a daily dose range of 150 to 450 mg. Neurotoxicity can occur at approximately 3 grams, leading to symptoms ranging from mild delirium and sympathetic over-activation (tachycardia and hypertension) to severe manifestations such as intractable seizures and coma. Cardiac toxicity is typically observed at around 10 grams, resulting in profound hypotension, bradycardia, systolic dysfunction and cardiac arrhythmias. These arrhythmias are commonly associated with QTc and QRS prolongation, ventricular tachycardia and ventricular fibrillation[1-3].
Unfortunately, there is no specific antidote available for bupropion toxicity, and management primarily focuses on supportive measures. Intravenous lipid emulsion (ILE) has shown promise as a useful tool in addressing bupropion toxicity, as demonstrated in our patient, altering the trajectory of her critical illness. Bupropion, a lipophilic drug, has demonstrated a notable response to lipid emulsion therapy in treating lipophilic drug-induced cardiac toxicity. The observed efficacy of lipid emulsion therapy aligns with the expanding body of evidence in this context. The proposed mechanism of action involves the creation of a ‘lipid sink’ through which the lipid emulsion binds to the lipophilic drugs, subsequently reducing their free concentrations and reversing cardiac toxicity. Nonetheless, the use of ILE therapy in bupropion overdose cases remains low, accounting for less than 1% of all cases. This limited adoption can be attributed to the absence of large, controlled studies, leading to significant uncertainties regarding optimal dosing, timing of therapy and the safety profile[3-5].
This case report comprehensively analyses bupropion toxicity management with lipid emulsion therapy. Numerous studies and case reports have contributed valuable insights into the benefits and risks of this approach. Shepherd et al. and Spiller et al. demonstrated the efficacy of lipid emulsion therapy in intentional bupropion overdoses, while Gosselin et al. established evidence-based recommendations for its use in managing toxicological emergencies[4-6]. Lee and Sohn successfully treated cardiogenic shock induced by a toxic dose of bupropion using lipid emulsion therapy, while Herrman et al. managed a case of bupropion overdose complicated by cardiogenic shock through the combination of lipid emulsion therapy and vasopressor support[7-8]. Sirianni et al. were among the first to report a compelling case of resuscitation using lipid emulsion therapy in a patient who experienced prolonged cardiovascular collapse following an overdose of bupropion and lamotrigine[9]. These studies underscore the potential effectiveness of lipid emulsion therapy in bupropion overdose cases.
Despite the positive outcomes, it is crucial to exercise caution and consider the potential risks associated with lipid emulsion therapy. Hayes et al. conducted a systematic review, highlighting adverse events reported after acute ILE administration and emphasising the need for monitoring and careful consideration of potential complications[10]. Specific cases have reported adverse effects related to lipid emulsion therapy in the context of bupropion toxicity, including prolonged lipaemia and pancreatitis resulting from extended infusion, and cases of asystole following intravenous fat emulsion administration[11-12]. Additionally, Schulz et al. documented neurological complications associated with fat emulsion therapy, emphasising the importance of cautious administration and vigilant monitoring[13]. Interestingly, the administration of ILE in our case may have contributed to the deterioration of her respiratory status, necessitating additional interventions to support ventilation.
CONCLUSION
The pendulum swings regarding lipid emulsion as an antidote, as discussed by Mullins and Seger, emphasise the importance of individualised decision-making considering specific clinical circumstances[14]. Although promising, clear guidelines for dosing, timing and the safety protocol are yet to be established and further research is needed. Prioritising evidence-based medicine and first-line therapy is fundamental in managing this toxicity effectively. Intravenous lipid infusion may act as a valuable adjunctive therapy if applied within established guidelines. A noteworthy case report by Tolentino et al. suggests that lipid emulsion therapy combined with plasmapheresis could offer a comprehensive treatment strategy[15]. Nevertheless, optimal patient outcomes hinge on individualised decision-making, informed consent and effective communication about treatment risks and benefits. The adoption of a patient-centred approach is key to the successful management of bupropion toxicity.