ABSTRACT
Introduction: Seizure as a sole sign of Stanford Type A aortic dissection (AAD) is mentioned in the medical literature. In this case, AAD was manifested by external bilateral jugular vein distention and generalized seizure.
Patients and Methods: A 47-year-old woman presented to the Emergency Department with convulsions in the upper and lower extremities. She was diagnosed with AAD and transferred to a hospital with cardio-thoracic capabilities for surgery.
Conclusion: Seizure resulting from aortic dissection has been explained by general cerebral hypoperfusion. However, jugular vein distention could be secondary to increased thoracic pressure, due to compression of the pulmonary artery by the ascending aorta.
LEARNING POINTS
- To our knowledge, this is the first report of generalized seizure with the presence of bilateral jugular vein dilatation as a sign of aortic dissection.
- Medical staff should be aware of this unusual presentation.
KEYWORDS
Type A aortic dissection, external jugular vein distention, fatal medical emergency
CASE DESCRIPTION
A 47-year-old woman with no past known pathological medical history presented to the Emergency Department after collapsing and displaying convulsive movements in the upper and lower extremities. According to family members, she had not complained previously of pain in the chest, head, abdomen, or back. The Emergency Medical Staff team diagnosed a generalized seizure with the need of immediate airway protection, and she was intubated enroute to the hospital.
METHODS AND PROCEDURES
An initial assessment of vital signs revealed normal blood pressure (BP) 95/62, heart rate (HR) 70, body core temperature 36.8 °C, and O2 saturation 98% with Fio2 0.60. Glucose level was normal, and a 12-lead electrocardiogram (ECG) showed normal sinus rhythm without ST-T segment changes. Further investigation included blood pressure measurements in both arms that showed slight differences (right arm 95/62, left arm 106/60), and pupil examination that was unremarkable. We palpated peripheral pulses in both upper and lower extremities. However, an unusual finding was bilateral jugular vein distention (JVD).
Considering this finding, we extended our initial routine blood tests to include troponin level and D-dimer (Table 1).
Because of the clinical finding of JVD, we included a bedside echocardiogram to investigate the possibility of pericardial effusion or cardiac tamponade. The initial evaluation in the Emergency Department did not reveal the underlying cause of the patient’s medical signs and symptoms, although the bedside echocardiogram demonstrated a non-specific enlargement of the right ventricle. Further investigation included a CT angiogram of the head and chest.
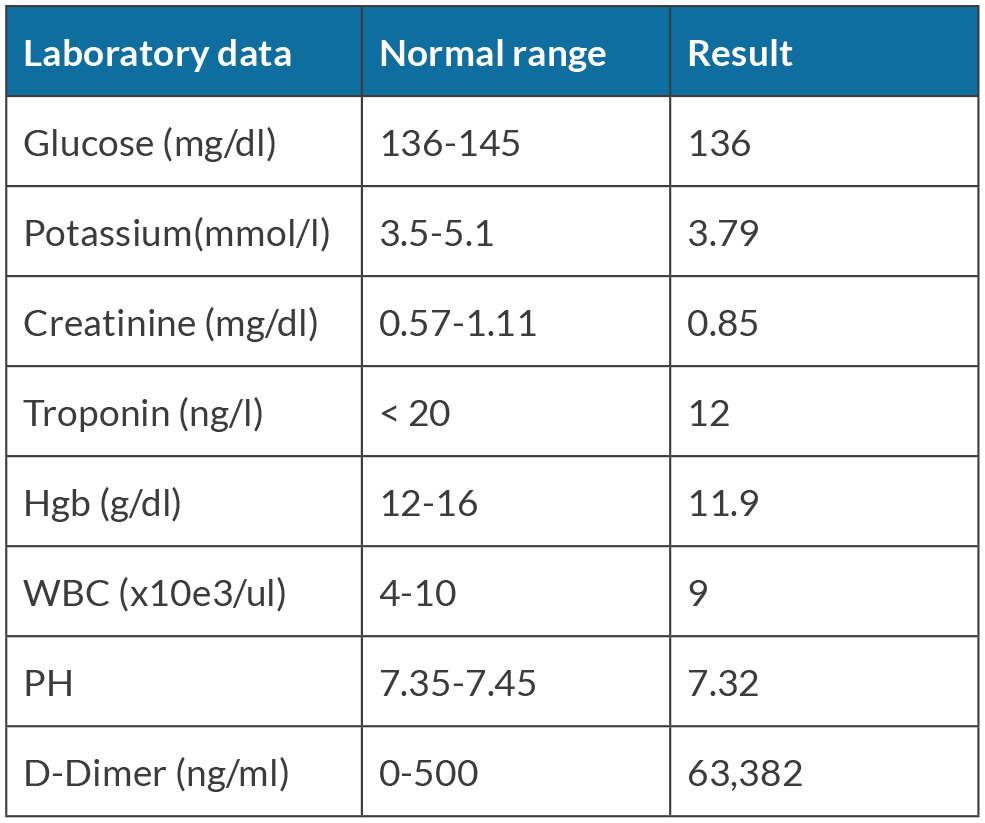
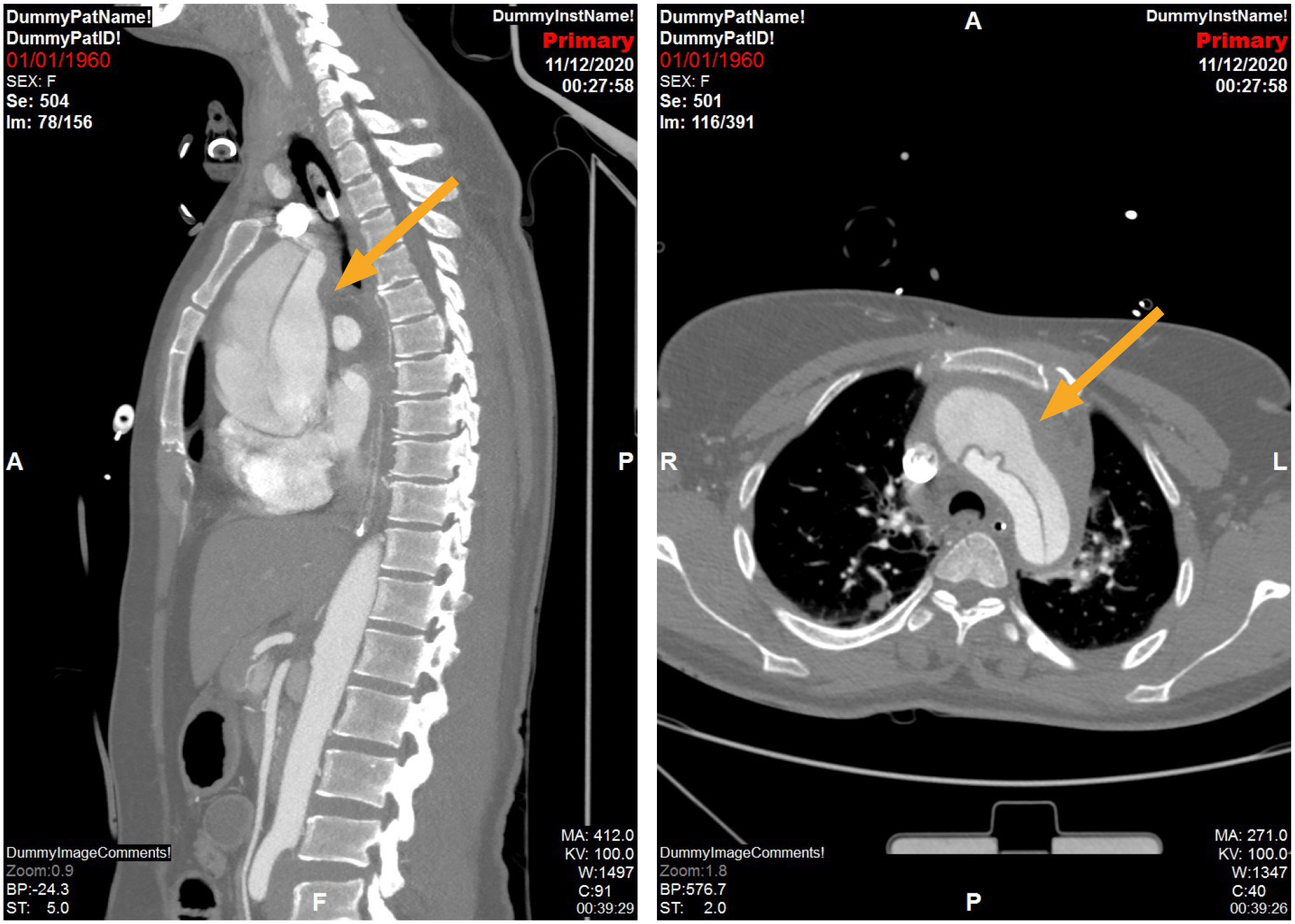
The brain scan showed no signs of bleeding or ischemia, while the CT angiogram of the chest showed acute Stanford type A aortic dissection (AAD), extending to the brachiocephalic artery, proximal subclavian artery with infiltration to the left common carotid artery (Fig. 1), as well as compression of the pulmonary artery by the ascending aorta (Fig. 2).
Figure 1. CT Angiogram showing Type A Aortic Dissection with axial and sagittal views as shown with arrow above including true and false lumen
Figure 2. Compression of Pulmonary Artery as shown with arrow above due to hematoma originating from Dissected Ascending Aorta
Based on this catastrophic diagnosis and its high mortality rate, we transferred the patient to a hospital with cardio-thoracic capabilities for surgical intervention.
The surgery was complicated, involving different surgical teams, including thoracic surgeons, neurosurgeons, and an intensive care cardiologist.
After the surgery and a long rehabilitation period the patient was discharged to outpatient rehabilitation with preserved neurological function and right-side motor dysfunction of the upper and lower limbs.
DISCUSSION
AAD is considered a medical emergency with high rates of mortality and morbidity[1]. The incidence of AAD in the general population ranges between 4 and 6 cases per 100,000 persons per year. The International Registry of Acute Aortic Dissection reported a mean age at presentation of 63 years, with male predominance[2].
AAD occurs when there is a tear in the inner wall of the aorta, which causes blood to flow between layers of muscular wall[3]. AAD may have several complications with diagnostic, prognostic and management implications, such as hypotension and shock, pericardial effusion and tamponade, periaortic hematoma, visceral and peripheral ischemia, renal insufficiency, mesenteric hypoperfusion and acute limb ischemia[4].
According to the Stanford system, AAD is categorized as type A or B, with type A dissections involving the ascending aorta irrespective of the site of the tear, and tType B including all dissections that do not involve the ascending aorta[2]. This classification is crucial for making appropriate decisions regarding future management, such as surgical intervention[4].
Multiple factors contribute to AAD, arterial hypertension and known connective tissue disease being the most common risk factors. The most frequent presentation is sudden-onset severe chest or back pain[1]. Usually, the pain is described as tearing or ripping by patients who survive the life-threatening condition[3].
In this case, we found some interesting connections with previously published case reports. In all cases where the seizure was the initial manifestation of AAD, the CT scan showed three major similarities:
1. Type A Aortic Dissection is the main finding in all known cases attributed to seizure.
2. The dissection extends beyond the ascending aorta, towards the region of the brachiocephalic artery and the common carotid artery.
3. There are remarkably elevated levels of D-dimer in all cases of AAD. D-dimer is however not specific to the diagnosis of AAD and can be elevated in many other medical pathologies.
To the best of our knowledge, this case report is the only one describing a seizure as the first sign of type A AAD and bilateral JVD. In previously published case reports, the seizure can be secondary to general cerebral hypoperfusion, demonstrating hypoxia or stenosis of the common carotid artery[5]. However, one could speculate that external JVD is secondary to increased pressure in the thoracic cavity, particularly due to compression of the pulmonary artery by the ascending aorta, as shown by the CT angiogram (Fig. 2). This compression prevents blood from returning to the right side of the heart from the upper extremities due to mechanical compression of the aortic arch on the pulmonary artery. This eventually leads to accumulation of blood in the upper extremities rather than normal blood flow through the right ventricle to the pulmonary artery, thus making JVD clinically obvious. This case suggests the importance of checking for life-threatening JVD in case of seizures, especially when there is no clear reason explaining the symptoms and clinical findings.