ABSTRACT
Angiotensin-converting enzyme inhibitors (ACEI) are frequently prescribed for cardiovascular and renal diseases. However, ACEI-induced visceral angioedema is a rare occurrence that often goes unnoticed and poses a diagnostic challenge due to its non-specific and diverse symptoms. Key diagnostic indicators on a CT scan include the ‘target’ sign, elongation of bowel loops, enlarged mesenteric vessels, mesenteric edema with or without ascites, thickened omentum, and the absence of vascular compromise or adenopathy. Discontinuation of ACEI usually results in symptom resolution within 48 hours. While this phenomenon is more commonly observed in females and African Americans, we present a case of a Caucasian male who underwent an extensive diagnostic evaluation, including exploratory surgery, before ACEI-induced angioedema was considered.
LEARNING POINTS
- The occurrence of angiotensin-converting enzyme inhibitors (ACEI)-induced visceral angioedema is infrequent, frequently overlooked, and presents a diagnostic challenge due to its wide range of non-specific symptoms.
- While ACEI-induced visceral angioedema is more frequently observed in females and African Americans, it is crucial not to overlook the possibility of this phenomenon in other demographic groups as well.
- Its rarity emphasizes the importance of including it in the list of potential conditions to be considered, thus preventing unnecessary tests and procedures.
KEYWORDS
ACEI, visceral angioedema, lisinopril, mesenteric edema, ‘target’ sign
INTRODUCTION
Angiotensin-converting enzyme inhibitors (ACEI) are one of the most commonly prescribed medications in the treatment of cardiovascular and renal diseases around the world. Angioedema secondary to ACEI is a well-known side effect which most commonly affects the face, lips, tongue, and upper airways. Visceral angioedema is a rare and under-recognized clinical phenomenon and thus poses a diagnostic challenge. Gastrointestinal symptoms due to ACEI-induced mesenteric angioedema are non-specific and can mimic several other abdominal diseases. It is thus important to recognize the signs of ACEI-induced mesenteric angioedema with appropriate clinical, laboratory, and imaging analyses.
CASE PRESENTATION
A 49-year-old male with a history of type 1 diabetes mellitus, Grave’s disease, and hypertension presented with chronic intermittent abdominal pain, nausea, vomiting, and diarrhea for more than 5 years. FODMAP-(fermentable oligosaccharides, disaccharides, monosaccharides and polyols) and lactose-free diets, fiber, cholestyramine, dicyclomine, doxepin, steroids, mesalamine, and antibiotics had been tried without improvement in symptoms, suggesting irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), lactose intolerance as unlikely causes. Laboratory analyses including tests for fecal calprotectin, fecal fat, Helicobacter pylori, IgA, and tissue transglutaminase (tTG) were unremarkable. Multiple endoscopies showed diverticulosis, and biopsies taken under endoscopy were unremarkable. A capsule endoscopy was performed which showed subtle and superficial erosion in the jejunum.
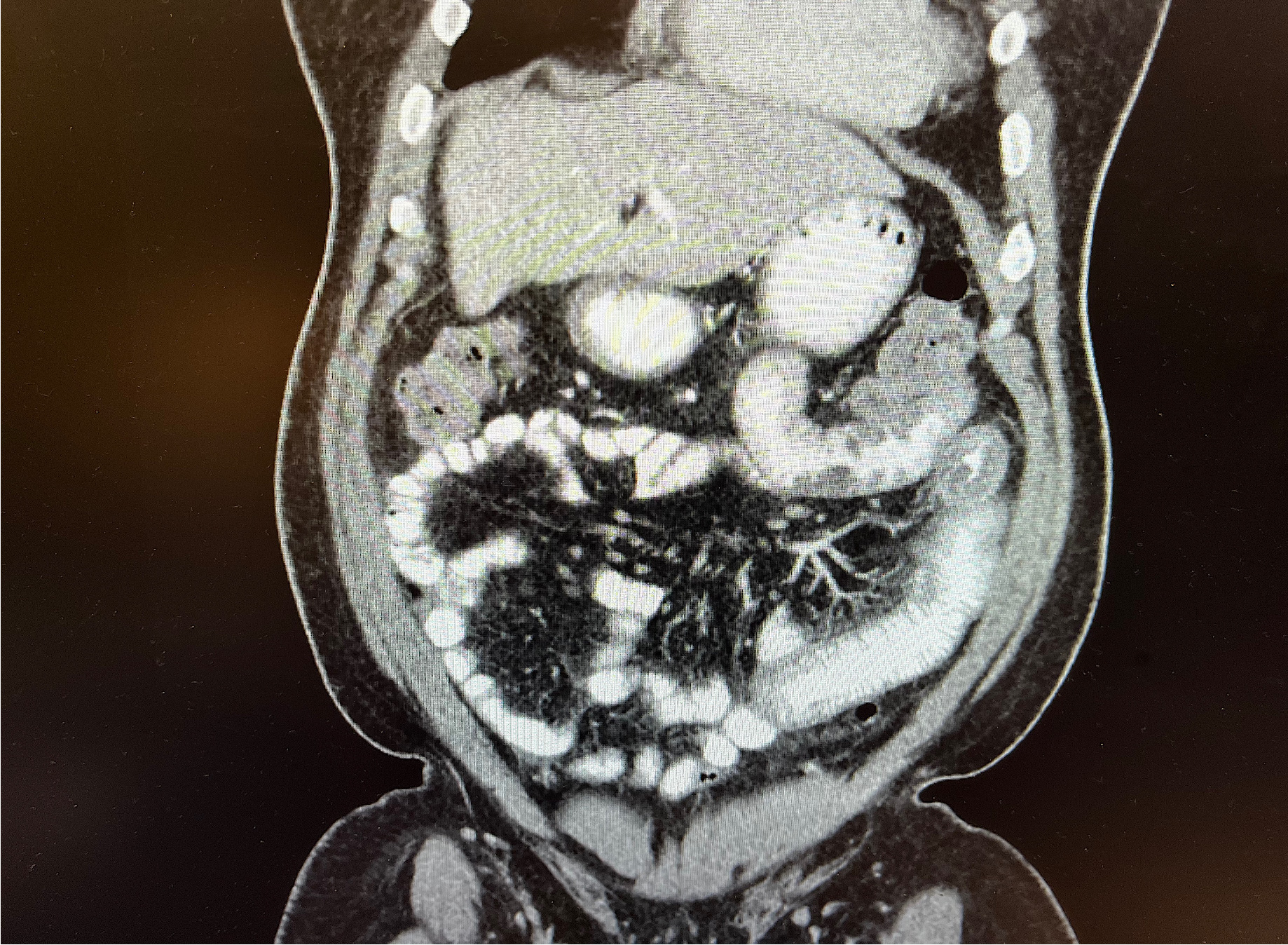
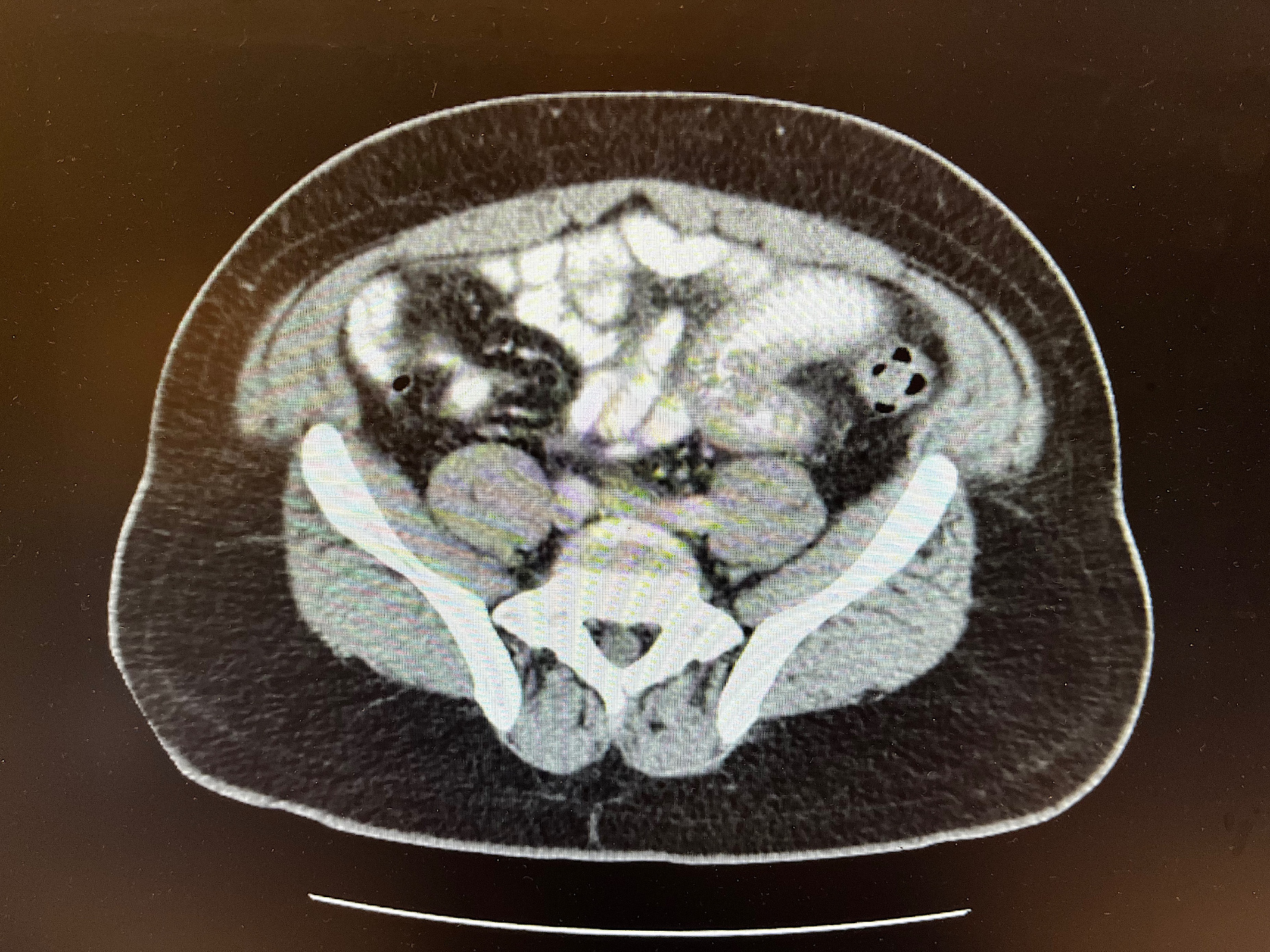
Several computed tomography (CT) scans including CT enterography showed multifocal jejunal wall thickening (Figure 1). One CT revealed possible diverticulitis, and another showed diffuse mesenteric edema (Figure 2). The gastric emptying study was normal. Hepatobiliary iminodiacetic acid (HIDA) scan revealed reduced gallbladder ejection fraction.
During this time the patient underwent two surgeries: an exploratory laparotomy showing possible evidence of creeping fat but no apparent inflammatory bowel disease, and a cholecystectomy which failed to relieve symptoms. Finally, an extensive chart review led to a trial of holding the patient’s lisinopril. The patient returned to the clinic one month later symptom-free.
DISCUSSION
ACEI are medications used to treat and manage hypertension, which is a significant risk factor for multiple cardiovascular conditions. ACEI produce vasodilation by suppressing ACE II formation and by inhibiting bradykinin (a vasodilator substance) metabolism. An elevated level of bradykinin causes vasodilation and increased vascular permeability of the postcapillary venules leading to plasma extravasation and eventual development of angioedema. ACE inhibitor-induced angioedema is believed to result from defective degradation of bradykinin, des-Arg9-BK (a metabolite of bradykinin), and substance P. Studies have shown that in patients taking ACEI, reduced activity of the bradykinin metabolizing enzyme, aminopeptidase-P is associated with an increased risk of developing angioedema[1].
Angioedema has been shown to occur in 0.1-0.7 % of patients taking ACEI and typically presents as swelling of the face, tongue, and lips. Isolated gastrointestinal wall (visceral) involvement is rare and is often missed. This diagnostic challenge frequently causes patients to undergo avoidable testing, surgeries, and procedures leading to delays in diagnosis[2]. A review of 34 case reports between 1980 and 2016 by Palmquist and Matheus found several trends, the disease affecting preferentially females (85%), middle age (average age ~ 49.5 years) patients, and African Americans. Abdominal pain is associated in 100% of cases. Lisinopril was the most reported ACEI, but this could also be related to its more frequent prescription. The reactions occurred with both low and high doses[3].
Gastrointestinal symptoms are non-specific and range from abdominal pain, nausea, vomiting, and watery diarrhea to ascites with onset reported between a few days to a decade after starting the ACEI. Laboratory results are usually normal but may show mild leukocytosis. CT findings are key to making the correct diagnosis and include segmental small bowel thickening; ‘target’ sign (submucosal marked hypoattenuation between enhancing mucosa and serosa); straightening/elongation of bowel loops; prominent mesenteric vessels; mesenteric edema with or without ascites; thickened omentum; normal appearance of pericolic fat; no vascular compromise or adenopathy. These CT findings alone can exclude other diagnoses like inflammatory bowel disease, vasculitis, small bowel lymphoma, obstruction, and mesenteric ischemia[4].
The management of ACEI-induced mesenteric angioedema is supportive with hydration, bowel rest, pain control, and discontinuation of the offending agent. Symptoms generally improve 24-48 hours after medication discontinuation[5].
Millions of patients are currently taking ACEI and the number keeps rising. The differential diagnosis for patients taking ACEI who present with gastrointestinal symptoms should consider small-bowel angioedema. Although the most common presentation is a middle-aged female patient on ACEI with abdominal pain, our case proves that it is not always the case. Early suspicion of ACEI-induced mesenteric angioedema is essential to prevent unnecessary testing, surgery, and morbidity.