ABSTRACT
Glucocorticoid intramuscular injections are a quick, routine procedure done in an outpatient setting to relieve musculoskeletal pain quickly. However, despite being a low-risk procedure it can lead to local infections, including abscess and skin necrosis, and even more rarely, bacteraemia and multi-organ failure. In this case, we present a healthy, immunocompetent woman in her 40s diagnosed with a retroperitoneal abscess due to methicillin-resistant Staphylococcus aureus after an intramuscular injection of triamcinolone.
LEARNING POINTS
- Injections of glucocorticoids are commonly used in medical practice to alleviate musculoskeletal pain in addition to oral non-steroidal anti-inflammatory agents.
- Complications of injections include abscess formation, skin necrosis and sepsis, typically from Staphylococcus aureus or other skin colonisers.
- It should be understood that there are risks associated with injections regardless of age or co-morbidities, so these risks should be discussed with the patient in depth before administration.
KEYWORDS
Triamcinolone, intramuscular injection, musculoskeletal pain, retroperitoneal abscess, methicillin-resistant Staphylococcus aureus (MRSA)
INTRODUCTION
Glucocorticoid intramuscular (IM) injections are a non-invasive, commonly used treatment option for musculoskeletal pain. These injections reduce pain and inflammation, increasing the mobility and functionality of patients with moderate to severe musculoskeletal pain. In addition, glucocorticoid injections are typically readily available and easy to do by a trained medical provider. Generally, these injections carry minimal risk and adverse events. However, adverse events such as abscess formation, skin necrosis and – more seldom – sepsis progressing to multi-organ failure are rare, but significant complications. These complications are commonly caused by skin colonisers such as Staphylococcus aureus and are seen to cause complications more often in elderly and immunocompromised individuals[1]. This case report highlights a rare, life-threatening complication after an IM injection of triamcinolone for lower back pain in a previously healthy, younger, immunocompetent patient.
CASE PRESENTATION
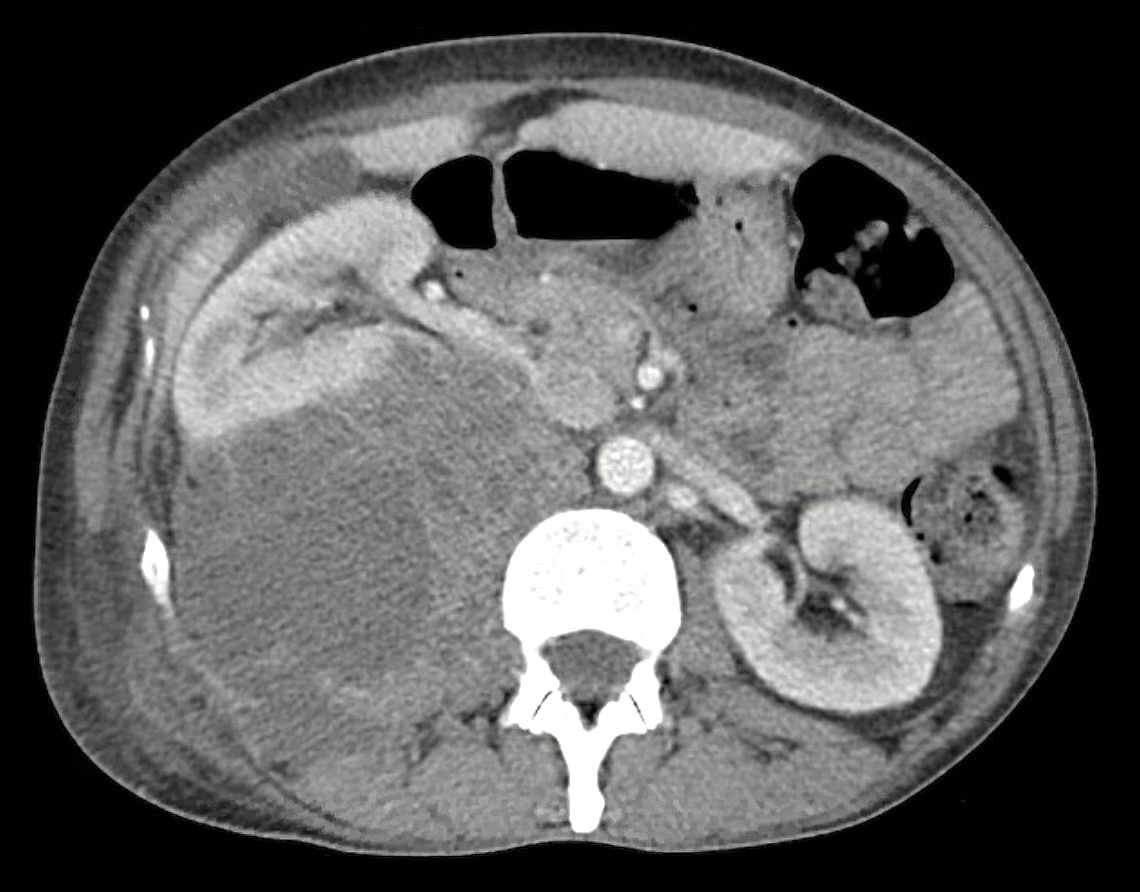
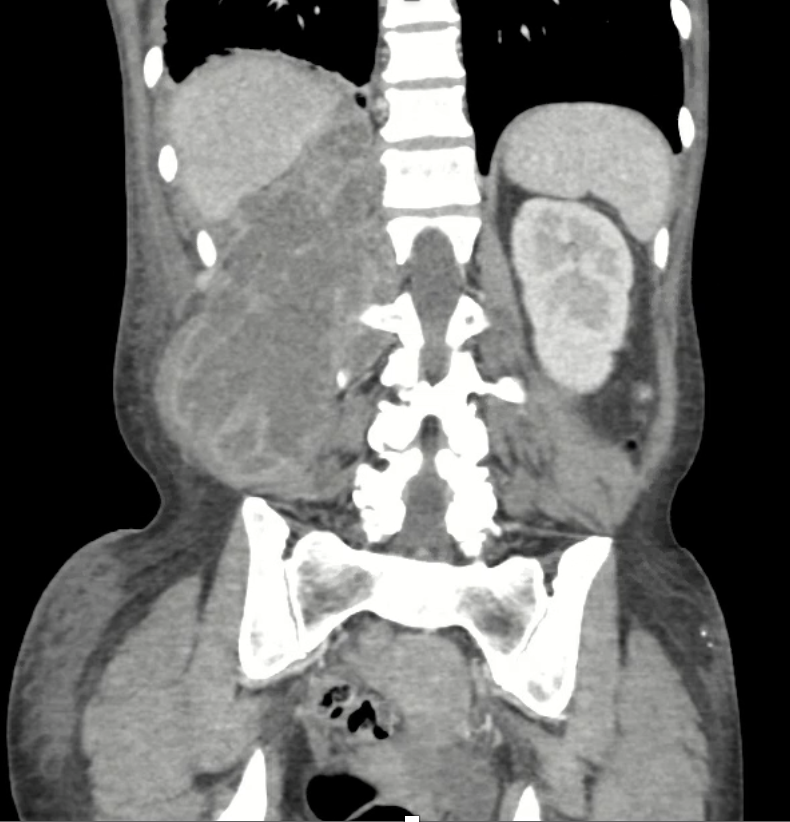
A woman in her 40s with no significant past medical history presented to the emergency department (ED) for a three-week history of right lower back pain with associated fever. Before this visit, she was seen by her primary care provider for dull back pain after performing an extensive amount of landscaping. Her symptoms were treated with an IM injection of triamcinolone in the upper right gluteus. The patient initially felt improvement in her back pain after the IM triamcinolone injection. However, her pain gradually worsened with associated chills and night sweats, prompting her to go to the ED for further evaluation. On clinical examination, the patient was tachycardic with a heart rate of 110 beats per minute (bpm), otherwise normotensive and afebrile. Initial laboratory studies revealed a white blood cell count of 20×103/ml with 83% neutrophil predominance, procalcitonin of 0.25 ng/ml and C-reactive protein of 26.4 mg/dl. A computed tomography (CT) scan of the abdomen and pelvis with intravenous (IV) contrast showed 16x12.1x8.6 cm multiloculated retroperitoneal fluid collection involving the right psoas muscle posterior to the right kidney (Figures 1 and 2). The patient was treated empirically with IV vancomycin, cefepime and metronidazole. The following day, the patient underwent ultrasound-guided drainage of the retroperitoneal abscess with pigtail catheter placement, and 10 ml of purulent fluid was obtained and sent for culture. The patient was continued on antibiotic therapy until fluid culture result was obtained; this was positive for 4+ methicillin-resistant Staphylococcus aureus (MRSA). As a result, antibiotic therapy was narrowed to IV vancomycin based on susceptibilities. A repeat CT scan of the abdomen and pelvis with IV contrast was done, which showed a pigtail catheter with large residual phlegmon: however, there was no significant residual fluid in the abscess (Figure 3). Four days later, the pigtail catheter was removed, IV vancomycin was discontinued and the patient was discharged home. She was followed up two weeks later showing a significant improvement in symptoms.
DISCUSSION
Glucocorticoid IM injections are considered one of the safest medical procedures and, because of this, are done routinely in primary care offices. Complications such as infection, including abscess formation and sepsis, are highly uncommon with one study reporting the IM injection infection rate as low as 1.9% of a 1500-patient case review[2]. Within this analysis, most patients who developed complications were immunocompromised or elderly. Unlike the typical demographic our patient was a female in her 40s with no prior medical history, who formed a sizeable retroperitoneal abscess. An extensive search through the National Library of Medicine yielded three similar cases of IM injection complications, one reporting abscess, another reporting sepsis and lastly, one reporting necrosis of the surrounding area, all after an IM injection of glucocorticoids[2,3,4]. Techniques to avoid these complications may seem evident to providers; however, ensuring sterility through the provider is crucial. In addition, ensuring the injection is placed intramuscularly instead of in the surrounding adipose tissue has decreased complication risk[3]. Finally, patients should also be aware of the dangers of this procedure and symptoms to be aware of following this injection, which would need prompt evaluation[5].
CONCLUSION
This case highlights the importance of proper technique, adequate evaluation and explanation of potential risks and benefits associated with IM injections of glucocorticoids, regardless of age and medical history. While these injections are considered to be simplistic, clinicians and patients should be aware of the potentially severe adverse manifestations.