ABSTRACT
Purpose: Flavobacterium lindanitolerans is an environmental Gram-negative, non-spore-forming rod which is usually not considered to be a human pathogen. Isolation from human clinical samples has been described only once. We report the first case of meningoencephalitis and bacteraemia with Flavobacterium lindanitolerans.
Case description: A 76-year-old female presented with fever, headache, alteration of mental status, marked meningism and dysarthria. A lumbar puncture demonstrated cerebrospinal fluid findings consistent with bacterial meningitis, and a broad-spectrum antibiotic therapy was initiated. Blood and cerebrospinal fluid cultures revealed a growth of Flavobacterium lindanitolerans. Based on antimicrobial susceptibilities testing, antibiotic treatment was changed to levofloxacin, resulting in a remission of the clinical symptoms after 21 days of treatment.
Conclusion: Flavobacterium species are extremely rare human pathogens. However, some of them have been reported to cause opportunistic infections. We describe the first case of meningoencephalitis and bacteraemia caused by Flavobacterium lindanitolerans which was effectively treated with levofloxacin for 21 days.
LEARNING POINTS
- This is the first case of a meningoencephalitis and bacteraemia with Flavobacterium lindanitolerans.
- Levofloxacin can be given for 21 days as a treatment of F. lindanitolerans.
KEYWORDS
Flavobacterium lindanitolerans, meningoencephalitis, Gram-negative bacteria, cerebral infection, bacterial meningitis, Gram-negative meningitis
CASE REPORT
A 76-year-old female was admitted to the emergency department of our hospital with fever, headache, mental alteration and dysarthria, starting approximately 24 hours before admission. Her medical history included a curatively treated vipoma of the pancreas – in this context, a splenectomy had been performed two years previously. She was currently in remission and had been vaccinated according to guidelines in the context of the splenectomy. Parkinson's disease, arterial hypertension and type 2 diabetes mellitus were also present. Her medication included levodopa with decarboxylase inhibitor, mirtazapine, Rivotril, insulin, pancreatic enzymes, esomeprazole, aspirin, metoprolol and enalapril. The specific medical history was unremarkable in terms of contact with animals, travel, hobbies, contact with infectious persons or recent blood transfusions.
The clinical examination showed an encephalopathic patient with a Glasgow Coma Score of 14, an oxygen saturation of 91%, and she was hypertonus, with abdominal tenderness on palpation and terminal meningism.
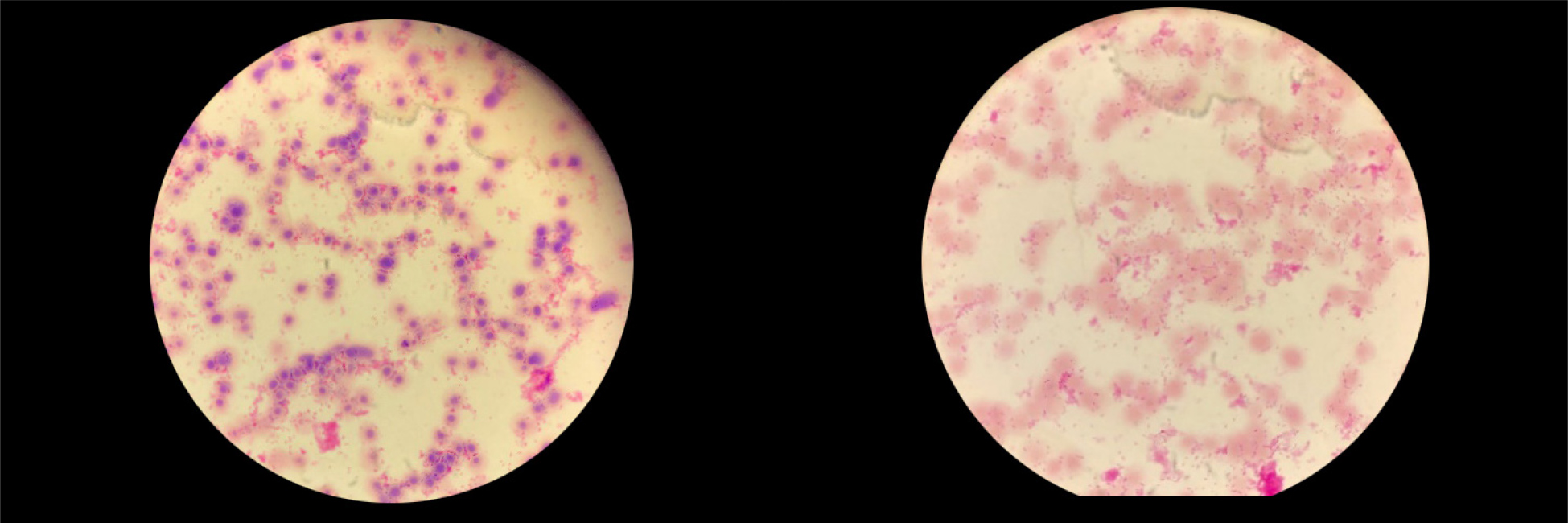
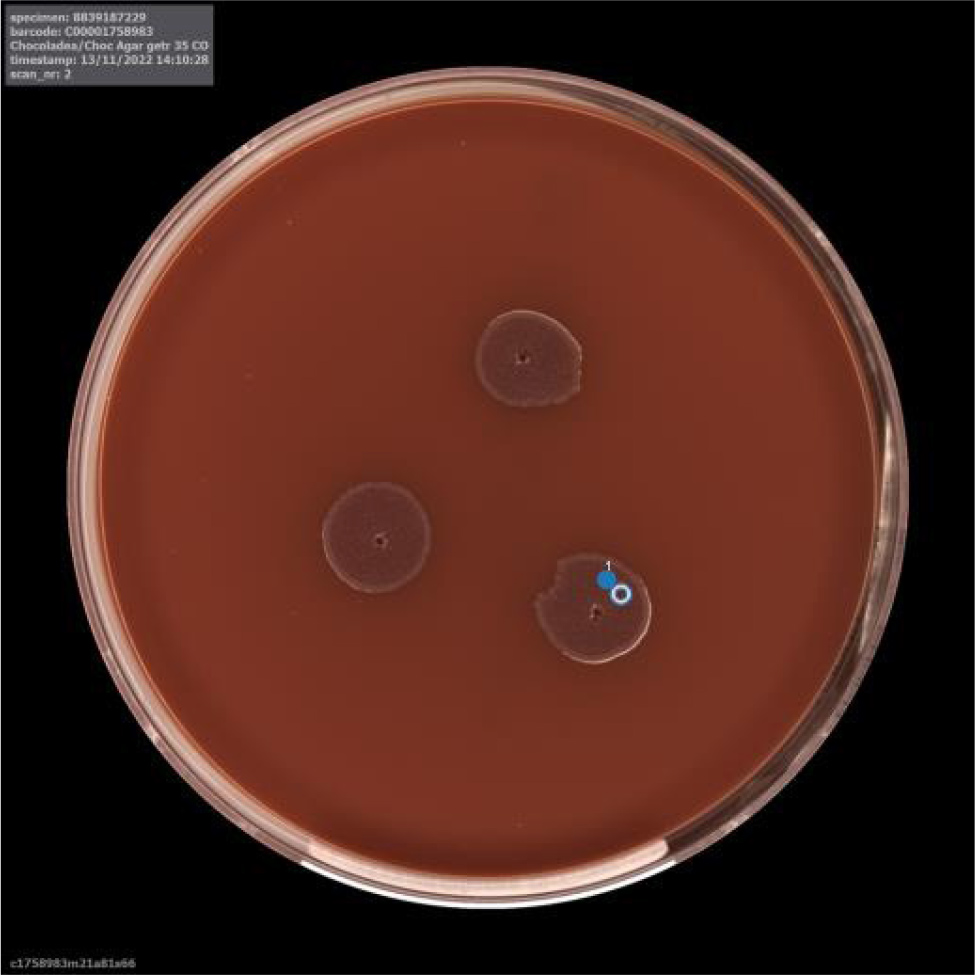
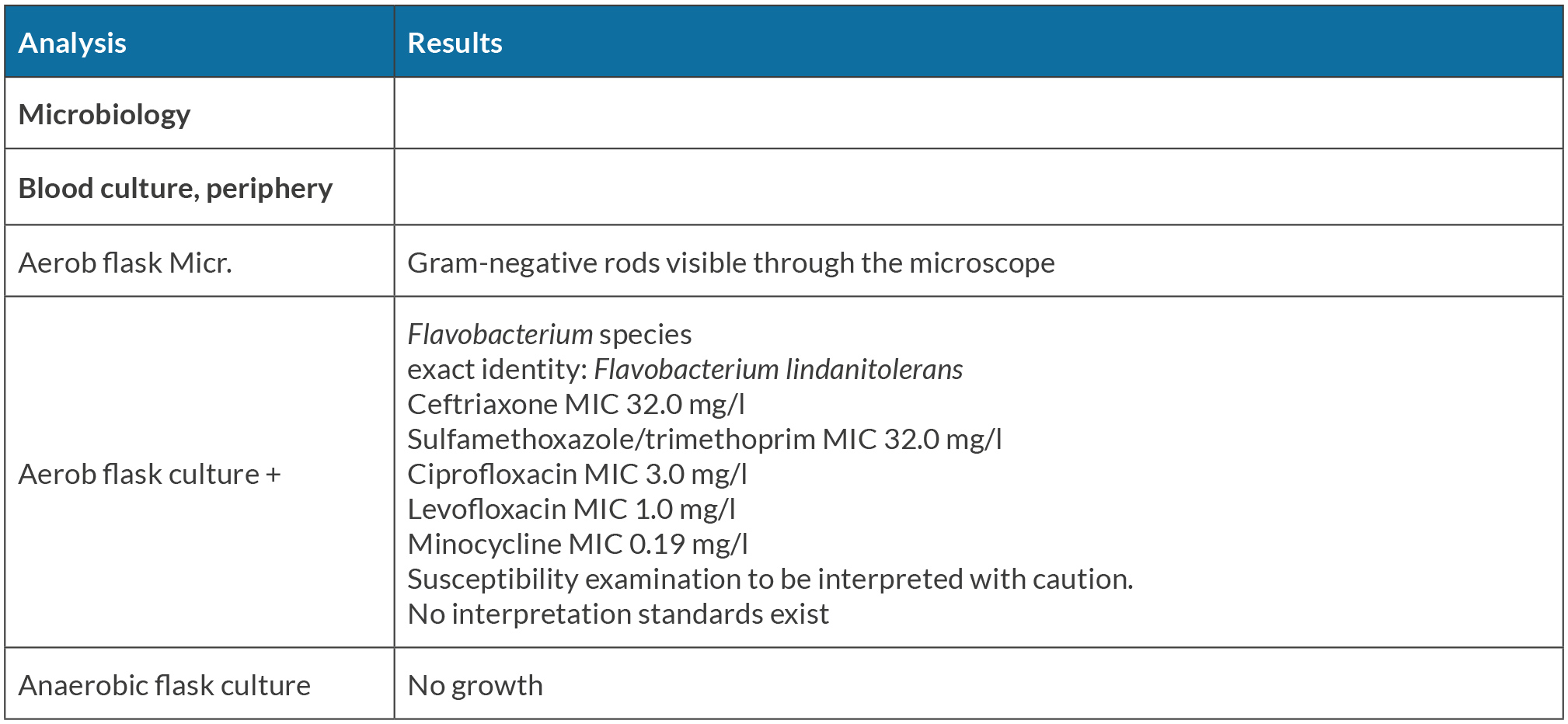
The laboratory findings demonstrated a leucocytosis (19 G/l) and an elevated C-reactive protein with a value of 50 mg/l. The cerebrospinal fluid (CSF) revealed a high cell count with 1078 white blood cells/m3 with 72% polymorphonucleocytes, hyperproteinorrachia (2.25 g/l), and a very high lactate level (8.0 mmol/l). A brain computed tomography image did not show relevant pathological findings. With the diagnosis of meningoencephalitis an empiric antibiotic therapy with ceftriaxone, amoxicillin and acyclovir was started. Dexamethasone was also administered. The patient showed a good response to the initial therapy, but some symptoms such as dysarthria, ataxia, slight left-leg paresis and a persistent meningism were still observed in the following days. A multiplex polymerase chain reaction of the CSF, including the varicella-zoster virus and the herpes simplex virus 1 and 2, identified no pathogen and therefore acyclovir was discontinued. Admission blood cultures became positive for Gram-negative rods (Fig. 1) and the microbiological laboratory later reported growth of a Flavobacterium species pending further identification. At this point, amoxicillin, dexamethasone and ceftriaxone were replaced by sulfamethoxazole/trimethoprim in combination with ciprofloxacin, as we found reports in the literature that these bacteria usually are resistant to beta-lactam antibiotics but show variable susceptibility to quinolones and sulfamethoxazole/trimethoprim. On the following day, Flavobacterium lindanitolerans was identified by MALDI-TOF mass spectrometry after 24h from bacterial growth on Columbia blood agar (Fig. 2). There was no growth on McConkey agar. Flavobacterium lindanitolerans was also found in the CSF after 48h incubation on Columbia blood agar and chocolate agar from CSF (Fig. 3). The minimal inhibitory concentration (MIC) was evaluated for amoxicillin, ceftriaxone, sulfamethoxazole/trimethoprim, ciprofloxacin, levofloxacin and minocycline (Table 1). There are no standardised interpretation criteria available for this pathogen. Based on these results, the antimicrobial therapy was again changed to intravenous levofloxacin 500 mg twice daily on the seventh day of hospitalisation, and continued by oral levofloxacin from day 13 until day 21.
Figure 1. Flavobacterium lindanitolerans in the light microscopy on a Gram preparation
Figure 2. Flavobacterium lindanitolerans growth on Columbia blood agar after 42 hours
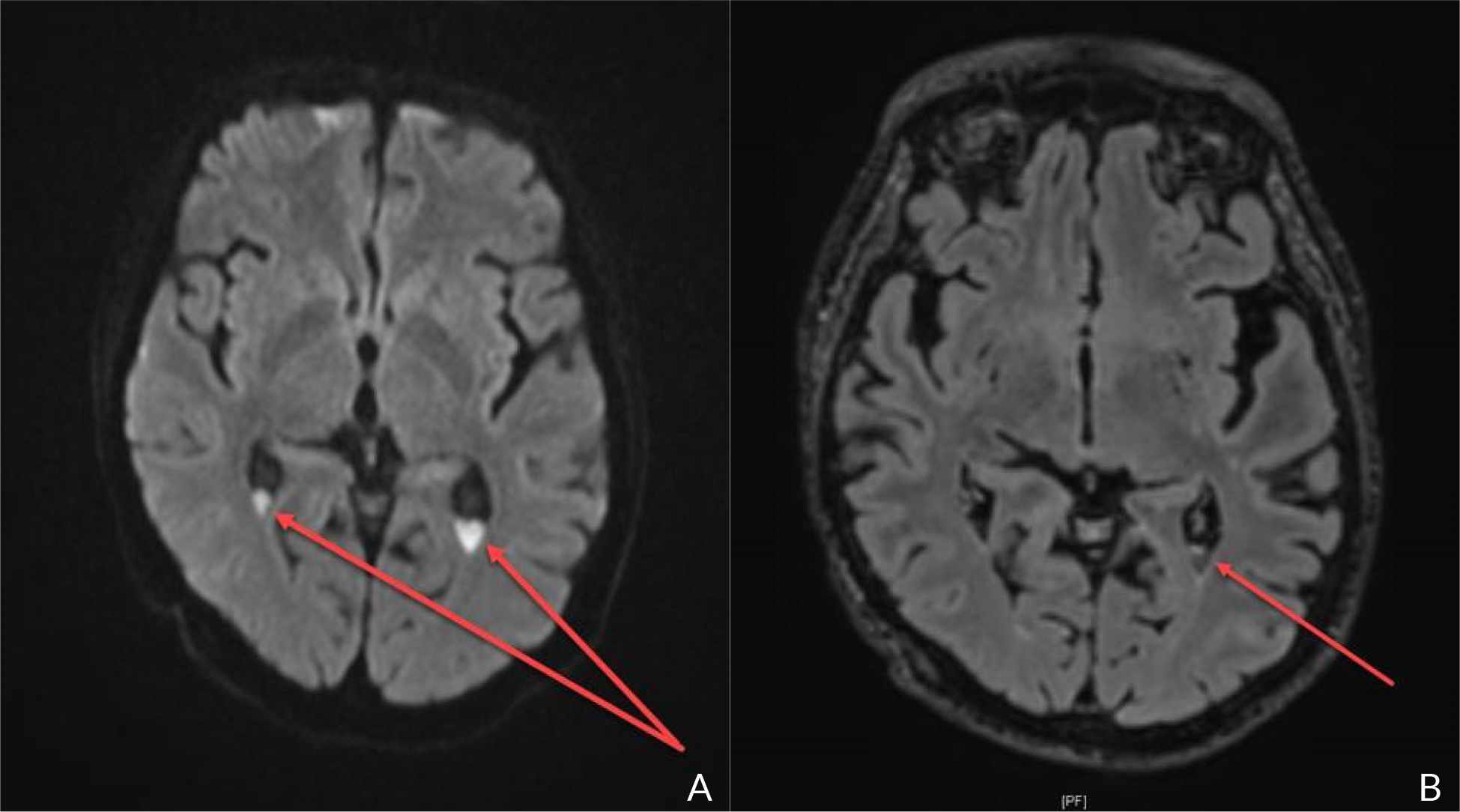
A brain magnetic resonance imaging (MRI) was also performed and showed purulent sediments in the lateral ventricles, and leptomeningeal inflammation without signs of encephalitis (Fig. 4). Therapeutic response to treatment was good. Apart from splenectomy and type 2 diabetes mellitus, no other cause of immunosuppression was found. The patient was discharged from the hospital into a geriatric rehabilitation facility after 14 days. During the first 20 days of rehabilitation, the patient showed improvement of mental status, dysarthria and gait with a slight imbalance and disorientation remaining.
Figure 4. Cranial MRI DWI (A) and T2 (B) – sequences showing hyperintensities and fluid level in the ventricular system, compatible with pus formation (red arrow)
Given the absence of data in the literature, we chose a treatment duration of 21 days analogous to other Gram-negative meningitis pathogens[1]. Before discontinuation of the antibiotic therapy, a follow-up MRI showed the absence of abscess and a reduction of the ventricular sediments. In the laboratory parameters performed, no signs of systemic inflammation were evident.
Taking into account that the entry point of the bacteria remains unknown, a colonoscopy is planned.
DISCUSSION
We report the first case of meningoencephalitis and bacteraemia caused by Flavobacterium lindanitolerans in an adult female patient.
Flavobacterium species are nonfastidious, glucose non-fermenting, oxidase positive, Gram-negative rods widely distributed in the environment[2] and are commonly isolated from soil, freshwater and marine water ecosystems, microbial mats, and infected fish and whales[3,4]. Although Flavobacterium species can cause disease in fish, human infections are extremely rare. Only a few cases of opportunistic infections have been described in humans including pneumonia, septicaemia and spontaneous bacterial peritonitis[5-8]. Only one case of meningitis by Flavobacterium ceti has been described[7]. However, this case report refers to a patient who had neurosurgery, craniotomy with clipping and wrapping of aneurysms in cerebral arteries, and as such was at risk for the development of healthcare-associated meningitis[9].
Flavobacterium lindanitolerans is routinely found in freshwater fish or soil[10]. To the best of our knowledge, this is the first reported case of meningoencephalitis and bacteraemia due to Flavobacterium lindanitolerans, and the second case in which this pathogen was isolated from clinical specimens. The first documented case involved a 5-year-old child with an enterovirus infection with pulmonary oedema and haemorrhage. In this case, Flavobacterium lindanitolerans grew in the cultures of the ascites[6]. Our patient presented typical clinical symptoms and laboratory findings of a bacterial meningoencephalitis. With the exception of diabetes mellitus and splenectomy, we could not identify other secondary immunodeficiencies in our patient.
Identification of Gram-negative, non-fermenting rods represented a diagnostic challenge in the era before MALDI-TOF, due to results provided by commercial systems and traditional methods not always being reliable, and thus there was a possibility of misidentifications and underestimation of the pathogen[5]. MALDI-TOF mass spectrometry improved the identification of rare bacteria, such as Flavobacterium and made it possible to identify other relevant new species of this genre[11].
The Flavobacterium lindanitolerans central nervous system infection in our patient was successfully treated with levofloxacin. Due to the lack of data in the literature there is no standard treatment regimen for infections caused by this pathogen. In the first reported case there is no information concerning treatment, because the patient died within the first 24 hours following hospital admission[6]. In our case Flavobacterium was resistant to sulfamethoxazole/trimethoprim, in contrast to other reported Flavobacteria, which were susceptible to this therapeutic agent. Based on the antimicrobial susceptibility testing with a low MIC and given the excellent central nervous system penetration of levofloxacin[12], we chose this agent to treat the patient. Regarding duration of therapy, we treated the patient based on the guidelines for community acquired Gram-negative meningitis, according to which an antibiotic therapy of at least 21 days is recommended[1]. Yet, the length of the therapy should be ultimately adapted to the individual clinical, laboratory and bacteriologic responses of the patient. Finally, performance of repeat analysis of the CSF could be considered to assess the response to therapy, something we did not do because of the overall good clinical and laboratory results.
Summing up the case, the patient diagnosed with a meningoencephalitis with Flavobacterium lindanitolerans showed a good response to the antibiotic treatment with levofloxacin for 21 days with only slight dysfunctions remaining 2 months after the infection.
As often observed in rare pathogens, the route of entry of the bacteria in the human body remains unknown in our patient.