ABSTRACT
Nerium oleander is a plant containing cardiac glycosides, and intoxication with its leaves is a medical emergency. We report,the case of a 73-year-old man who took a decoction of oleander leaves for a reckless purpose. Upon arrival in the emergency room, he presented an altered state of consciousness, drooling and vomiting. He was bradycardic with intermittent third degree atrioventricular block and typical downsloping ST-segment depression related to glycosides toxicity. Despite initial treatment with atropine, isoprenaline and repeated bolus of digoxin-specific antibody (Fab) fragments, symptoms were persistent 12 hours after admission. Suspecting that the patient not only drank the decoction but also ingested the leaves and had slow gastric emptying, we performed gastric lavage without benefit. We subsequently performed a gastroscopy that showed an oleander phytobezoar, and its removal permitted a rapid clinical improvement. Treatment with digoxin-specific antibodies for intoxication is well described and dosage should be adapted to the plasmatic level. Such an examination is useless in oleander intoxication because it does not represent the real quantity of toxin. The dosage of antibodies is empiric and should be guided by the clinical severity. In such intoxication, the presence of a phytobezoar from oleander leaves cannot be excluded, so we believe that a gastroscopy for its mechanical removal should always be considered to avoid persistent release of toxin.
LEARNING POINTS
- Ingestion of any part of the oleander plant can result in a severe cardioactive glycoside intoxication with potentially fatal arrhythmia and should be considered a medical emergency.
- Treatment consists of supportive care, correction of arrhythmias and electrolyte imbalance, and digoxin-specific antibody (Fab) fragments administration.
- Gastroscopy for mechanical removal of a phytobezoar responsible of persistent toxin release should be always considered.
KEYWORDS
Oleander poisoning, digoxin, digoxin-specific antibody fragments, phytobezoar
INTRODUCTION
Nerium oleander (common oleander) and Thevetia peruviana (yellow oleander) intoxication represents a toxicological emergency that manifests within few hours after ingestion. The reckless use of these plants is prevalent in South Asian countries with a very high frequency of morbidity and mortality[1]. All parts of these plants are toxic and contain a variety of cardiac glycosides, structurally similar to digoxin (neriifolin, thevetin A and B, oleandrin) that have a positive inotropic and negative dromotropic effect[2]. The mechanism of action of these substances is related to inhibition of the ubiquitous Na, K-ATPase pump that leads to an increase in extracellular potassium and intracellular sodium. The final consequence is a reduction of the elimination of intracellular calcium through the Na+/Ca2+ antiport resulting in greater activation of the contractile apparatus in cardiomyocyte (positive inotropic effect). The negative dromotropic effect depends on a direct action of the molecule on the vagus nerve (activation of the parasympathetic system)[3]. The main electrocardiographic manifestations are sinus bradycardia, atrioventricular block (any degree), atrial or ventricular fibrillation, and typical downsloping ST segment depression. Moreover, in association with heart effects, there are neurological symptoms (tremors, visual disturbances, fatigue, confusion, altered state of consciousness and coma), and gastrointestinal symptoms (abdominal pain, excessive salivation, nausea, vomiting and diarrhoea)[4]. Diagnosis is mainly based on the medical history. Although it is possible to measure the plasmatic concentration of cardiac glycosides, there is no correlation between their level and clinical effects in such intoxication[5]. Treatment is mainly supportive, but in the case of severe cardiac toxicity, the only specific therapy is the administration of digoxin-specific antibody (Fab) fragments that bind directly to the circulating cardiac glycosides, preventing them from binding to the site of action on the target cells and allowing their excretion via the kidney[6].
CASE REPORT
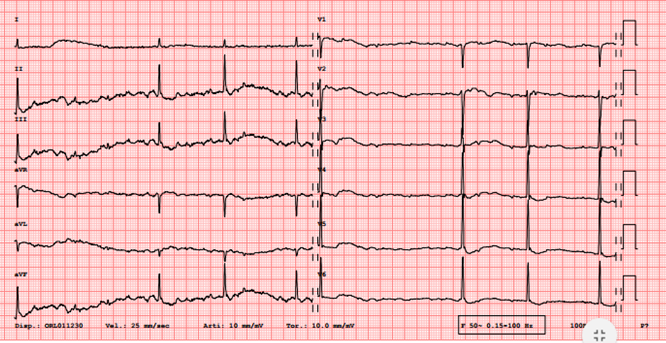
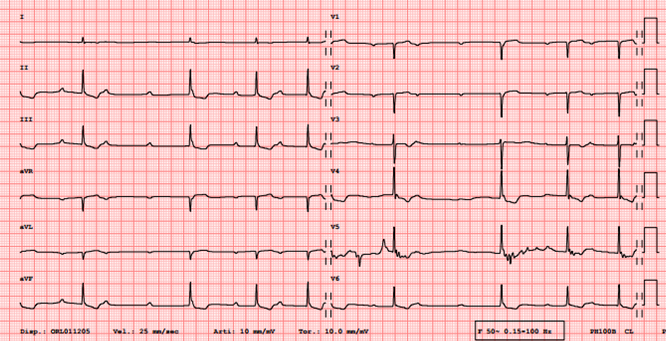
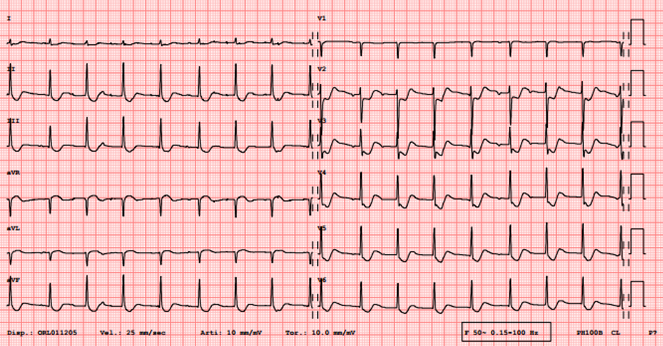
We present the case of a 73-year-old man, known for essential hypertension, major depression, and a long-term indwelling urinary catheter for benign prostatic hyperplasia. His chronic medications were alprazolam, clomethiazole, candesartan and bisoprolol. He was admitted to the emergency room few hours after a suicide attempt with ingestion of 1728 mg of clomethiazole and a decoction of oleander leaves. At the initial physical examination, the patient was drowsy and normotensive, with intermittent bradycardia; moreover, there was an important hypersalivation. The rest of the physical evaluation was not relevant. The ECG showed bradycardia with sinus rhythm alternating with second- or third-degree atrioventricular block. Moreover, the characteristic scooped-shape ST segment depression was present (Fig. 1). Because of a rapidly progressive decay of the state of consciousness, the patient was intubated in the emergency room. Laboratory examinations showed only mild leukocytosis with neutrophilic prevalence without hyperkalaemia; arterial blood gas analysis showed an acute respiratory acidosis. Considering the severe intoxication with cardiac glycosides, the national poison centre hotline was contacted, which recommended the administration of digoxin-specific antibody (Fab) fragments at an empirical dose of 40 mg. As the clomethiazole and oleander decoction ingestion took place at least 2 hours before admission to the emergency room, a gastric lavage or activated charcoal administration were not performed. The specific antibodies had a partial and short positive effect. After admission to the intensive care unit and during the first 12 hours in hospital, the patient presented many recurrent episodes of haemodynamic instability with severe bradycardia caused by third-degree atrio-ventricular block (Fig. 2) for which he received iterative boluses of atropine and continuous infusion of isoprenaline. Moreover, considering the impossibility of evaluating the ideal dosage of specific antibodies to administer, two more boluses were given for a total dose of 120 mg. Electrolyte imbalances, in particular potassium, were also corrected promptly. During this monitoring period in the intensive care unit, the patient experienced some emetic episodes which revealed the presence of oleander leaf residue. We then suspected slowed gastric emptying with persistence of oleander leaves. For this reason, we performed gastric lavage which had no effect. We therefore proceeded with a gastroscopy that showed a large phytobezoar of oleander leaves. After effective removal of this compaction of leaves, the evolution was progressively and rapidly favourable. The patient completely normalised his neurological and cardiological clinical status and could be extubated after 2 days. The last ECG (Fig. 3) before discharge to a psychiatric clinic, 4 days after ingestion of the decoction, showed an improvement but not a complete resolution of the characteristic signs of the digitalis effect.
Figure 2. ECG after 12 hours day: persistence of signs of digitalis intoxication with downsloping ST segment depression and intermittent third-degree atrioventricular block
Figure 3. Before discharge ECG with typical digital alterations with characteristic ST segment depression
DISCUSSION
The case described summarises the clinical presentation of severe cardioactive glycosides intoxication secondary to oleander poisoning. Due to the altered state of consciousness (probably related to clomethiazole and digitalis effects), once the airways were secured with intubation and mechanical ventilation started, our treatment focused on haemodynamic support with the administration of an anticholinergic agent (atropine) and beta agonist (isoprenaline) aimed at counteracting bradycardia. Considering the severe clinical manifestations, we decided to administer digoxin-specific antibody (Fab) fragments as recommended in digitalis intoxication. The dosage in this latter condition is relatively well described[7]. In the case of intoxication with plants containing cardiac glycoside, no such precise recommendations are available probably because no correlation exists between the real quantity of toxin ingested and plasmatic levels. We chose to apply a trial-and-error strategy adding boluses of 40 mg depending on clinical response. The persistence or rapid relapse of the signs of intoxication should raise suspicion of continuous release of toxic substance somewhere in the digestive tract. In the situation of pills ingestion, pharmacobezoar formation is well described (and some risk factors are known) and its mechanical removal with gastroscopy is the part of the recommended management but clear evidence is scarce[2]. The mechanism of the phytobezoar’s formation is also well known but in the case of plant intoxication, no risk factors are clearly identified. Nevertheless, in situations of multiple drug intoxication or with severe clinical manifestations, we believe that an endoscopy should be considered urgently. It is a minimally invasive examination that carries little risk and, not only can identify presence of such vegetal compaction, but also allows its immediate removal[8]. In our case, a gastroscopy was decisive since it removed the phytobezoar still present in the stomach responsible for the persistence of symptoms. After a critical analysis of the case, this procedure could be performed earlier, perhaps in the emergency room soon after intubation. In conclusion, a gastroscopy should be considered and probably performed in the early stages in the case of intoxication with a plant, and possible phytobezoar formation and consequent sustained release of toxin, to limit complications and permit a quicker resolution.