ABSTRACT
Spontaneous periodic hypothermia (SPH) is an exceptionally rare condition characterised by paroxysmal episodes of spontaneous hypothermia. While commonly associated with Shapiro syndrome, which includes SPH, hyperhidrosis and agenesis of the corpus callosum, there are also cases of SPH that do not exhibit these defining characteristics, known as ‘Shapiro syndrome variant'. These variants may present with diverse brain imaging findings but no agenesis of the corpus callosum, suggesting different potential aetiologies. Notably, the association of SPH with epilepsy has only been reported in a few cases, and confirming epileptic activity in the context of SPH remains a challenge.
In line with this, our report presents two exceptional cases of SPH without significant brain malformation, where we successfully confirmed the presence of epilepsy. The confirmation of epilepsy in these cases is particularly noteworthy, as it adds to the limited documentation of SPH cases with confirmed epilepsy. These findings contribute valuable insights into the association between SPH and epilepsy, enhancing our understanding of this rare condition.
Our report also addresses the broader clinical presentations and the physiopathological mechanisms of SPH. By providing comprehensive insights into these aspects, we aim to advance the existing literature and improve our understanding of SPH and its association with epilepsy.
LEARNING POINTS
- SPH is a rare condition, characterised by paroxysmal episodes of spontaneous hypothermia.
- A dysregulation of the hypothalamic thermostat is thought to be involved in the pathogenesis.
- Epilepsy may contribute to the pathogenesis of SPH, potentially by involving the hypothalamus.
KEYWORDS
Spontaneous periodic hypothermia, Shapiro syndrome, epilepsy
INTRODUCTION
Normal oral body temperature ranges from 35.7 °C to 37.6 °C, and hypothermia is defined as a core temperature below 35 °C. Shapiro's syndrome, first described in 1969, is characterised by a clinical trial of SPH, hyperhidrosis and agenesis of the corpus callosum[1]. SPH is a rare condition marked by paroxysmal episodes of spontaneous hypothermia. With fewer than one hundred recorded cases over the years, its exceptional rarity is apparent[2]. While SPH is commonly associated with Shapiro's syndrome, there are also cases of SPH that do not exhibit the typical features, known as ‘Shapiro syndrome variants'. Within this subset, a distinct group shows diverse brain imaging findings but lacks agenesis of the corpus callosum, suggesting a broader spectrum of the disease.
One significant aspect of this case report is the confirmation of epilepsy in our patients, which adds to the limited documentation of SPH cases with confirmed epilepsy. Confirming epilepsy in the context of SPH has been infrequently reported, making our findings particularly noteworthy. Our report presents two extraordinary cases of SPH without significant brain malformation, both characterised by confirmed epilepsy, hypothermia and altered mental status. These cases provide valuable insights into the association between SPH and epilepsy, further enhancing our understanding of this highly uncommon condition.
The underlying cause of SPH – as well as its infrequent association with epilepsy – remains poorly understood, presenting challenges in management. Our study aims to contribute to the limited existing literature by providing detailed clinical presentations, and discussing the physiopathological mechanisms of SPH. By examining these exceptional cases, we seek to shed light on the complexities of this rare condition and its association with epilepsy.
CASE REPORT
We present the cases of two patients who presented with altered mental status accompanied by concomitant hypothermia.
Patient 1
A 72-year-old woman was admitted to our Internal Medicine department with a progressive decline in mental function. She experienced symptoms of apathy, bradypsychia, somnolence, confusion, and nausea, occasionally becoming speechless for short periods. Her medical history revealed a previous diagnosis of breast cancer, which had been treated with surgery, radiochemotherapy and hormonal therapy eight years prior. The patient also had a history of high blood pressure and hypothyroidism, and was taking amlodipine, levothyroxine, furosemide and letrozole as ongoing medications.
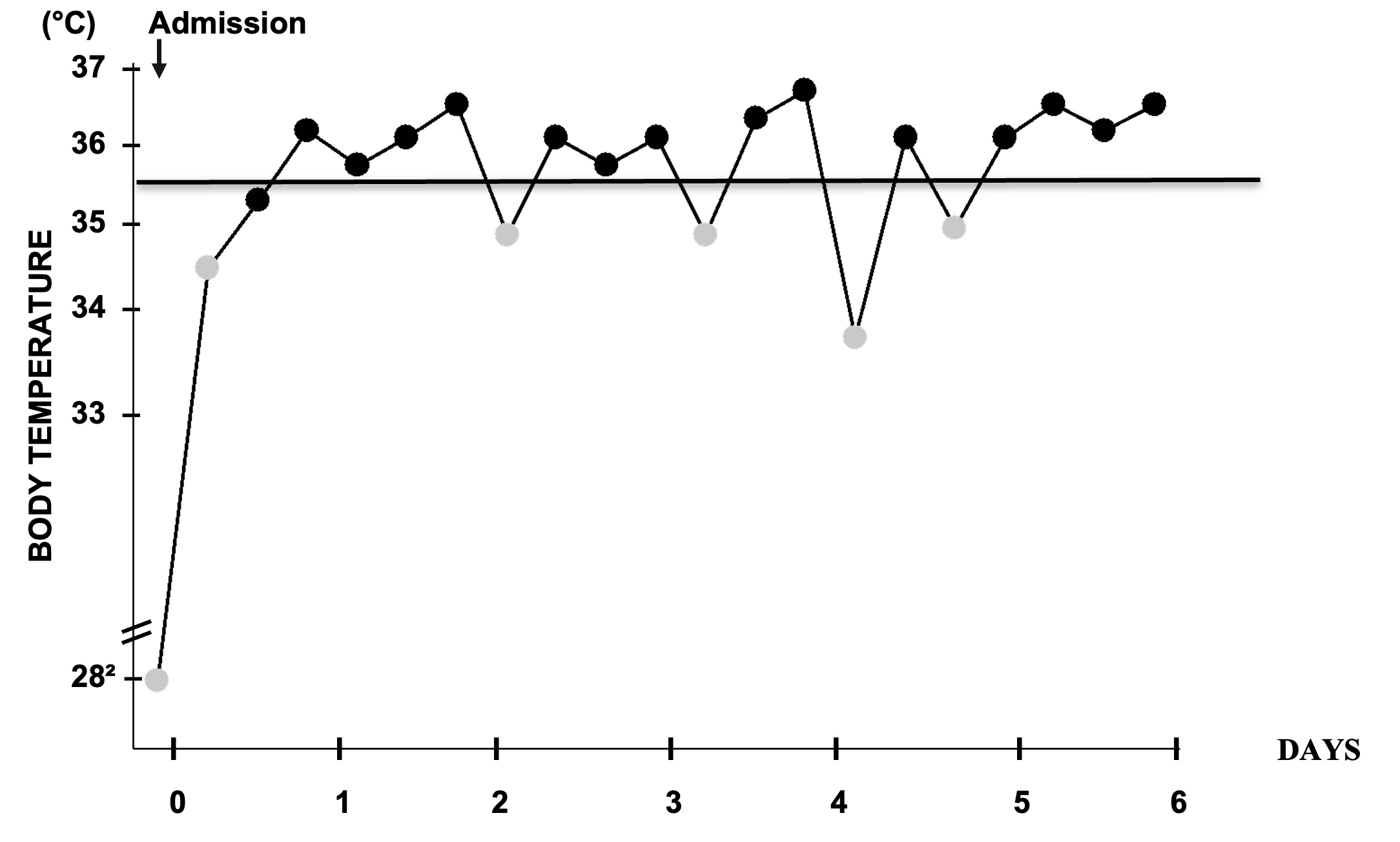
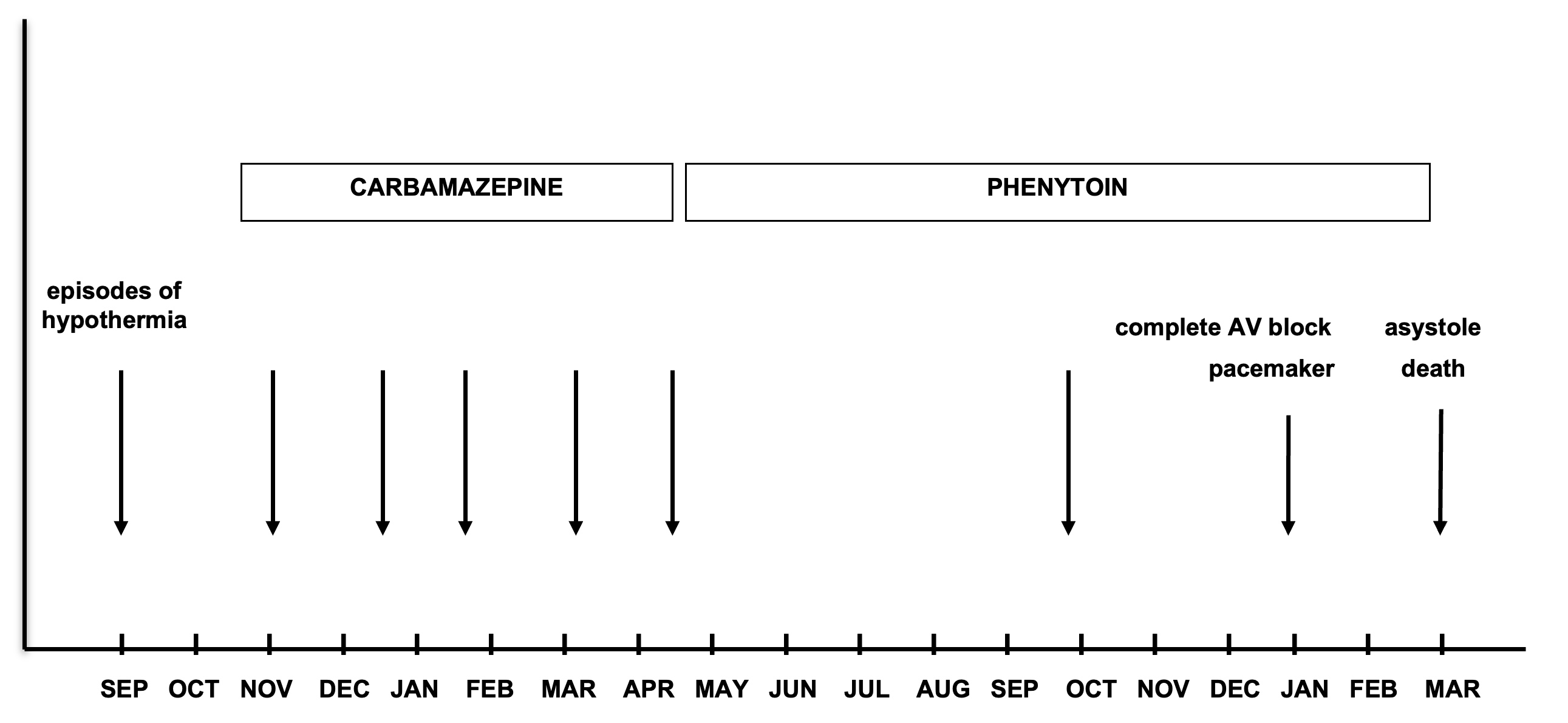
Upon examination, the patient exhibited fluctuating consciousness. Neurological findings included dysarthria, unsteady gait, and myoclonus in the arms. These neurological abnormalities correlated with spontaneous episodes of hypothermia, with recorded temperatures lower than 35 °C, including one episode as low as 28.2 °C, which resolved spontaneously (Fig. 1). Further review of her medical records revealed previous hospitalisations within the past year for similar symptoms, all of which resolved spontaneously (Fig. 2). Brain magnetic resonance imaging (MRI) did not show any abnormalities except for ischaemic lacunar lesions. Fluorodeoxyglucose brain positron emission tomography and computed tomography did not reveal any hyperactive lesions.
Figure 2. Records of hypothermia episodes and treatment history throughout the previous year. Each episode of hypothermia lasted between 5 and 7 days, with body temperature ranging from 28.2°C to 34.6°C
Importantly, the patient's electroencephalogram (EEG) confirmed the presence of epileptic activity, which is a unique finding in this case. Blood work-up showed mild pancytopenia, which normalised after resolution of hypothermia. Despite treatment with carbamazepine and phenytoin, three years later the patient developed a third-degree atrioventricular block during a hypothermic episode, which eventually proved fatal.
Patient 2
The second patient, also a 72-year-old woman, was admitted with symptoms of lethargy, apathy, and an unsteady gait. She had a history of essential tremor and depression, for which she was being treated with clonazepam and escitalopram. Physical examination revealed a pale, disoriented woman who was intermittently unresponsive. Increased deep-tendon reflexes and tremors were observed in her head and hands. Over the course of eight days following admission her neurological state fluctuated, and she experienced repeated episodes of hypothermia, with the lowest recorded temperature reaching 30.1 °C and subsequently resolving spontaneously. The patient had previously encountered two similar episodes without a diagnosis within the past six months, with a recorded temperature of 35 °C during one of those episodes. Routine laboratory tests did not reveal any significant findings.
Further examination of the second patient showed lacunar ischaemic lesions and mild leukoencephalopathy on brain MRI. No agenesis of the corpus callosum or other brain malformations were noted. Importantly, diffuse epileptiform activity was also observed on EEG in this case.
The patient initially failed treatment with topiramate and was subsequently switched to levetiracetam. She experienced one recurrent episode lasting three days, but has been free from any further recurrences for the past four years.
In both cases, thorough investigations were conducted to rule out endocrine and autoimmune disorders, accidental exposure to cold and toxic causes, such as medication-related intoxication. As the hypothalamus is the main structure responsible for regulating body temperature, special attention was given to assessing for any lesions in this region, but none were identified.
DISCUSSION
Symptoms and associated conditions
SPH presents with nonspecific symptoms similar to other forms of hypothermia. It can affect patients of all ages, with a higher prevalence observed in children[3]. Episodes can last from hours to days, and occur sporadically or multiple times per day[4]. Common symptoms include neurological disorders, hyperhidrosis (observed in approximately 75% of patients), pallor, hypotension, bradycardia and occasional biological abnormalities such as cytopenia[2].
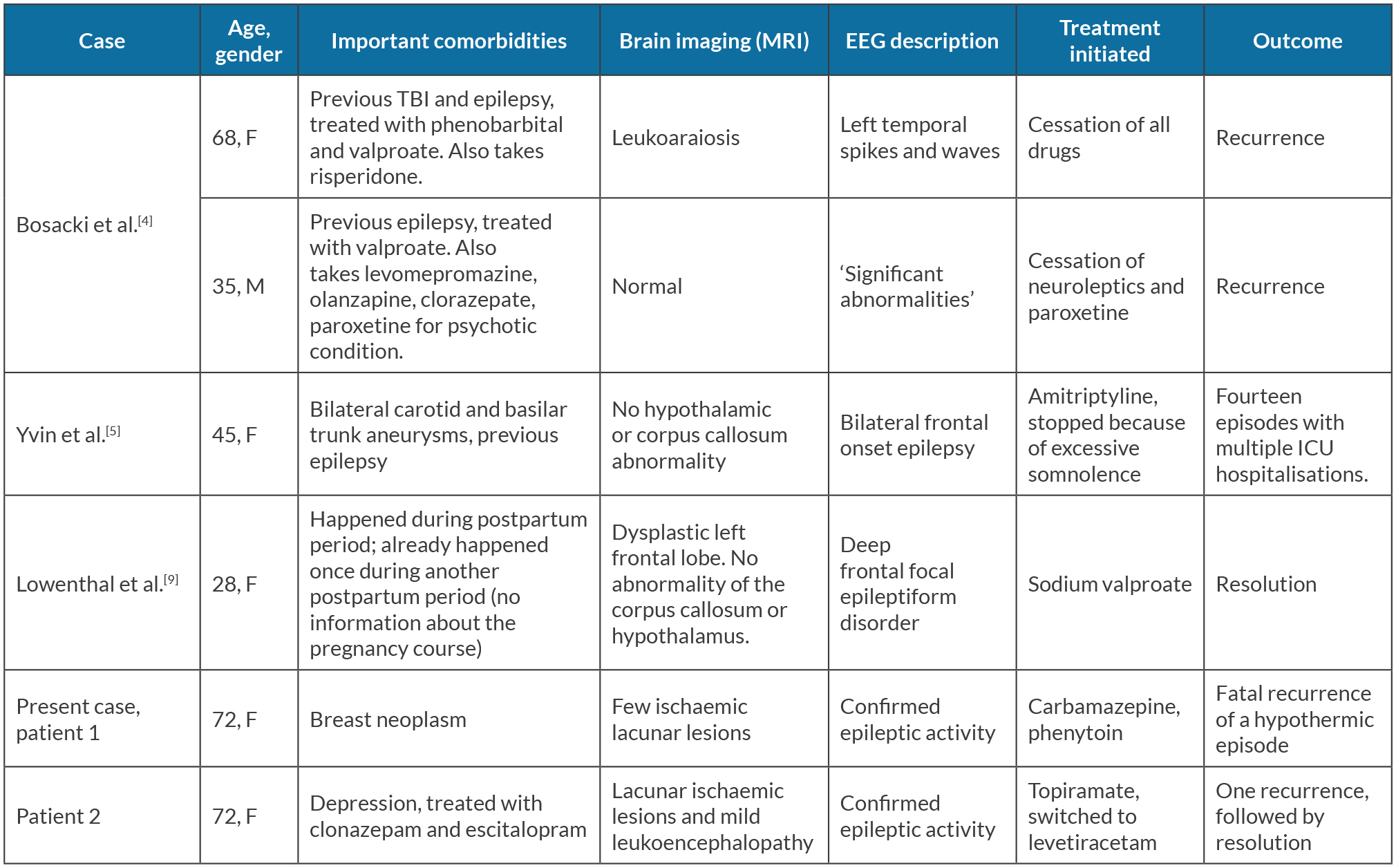
Regarding the association with epilepsy, a comprehensive review of the literature identified 51 reported cases of SPH that underwent cerebral morphology assessment using computed tomography or MRI techniques, revealing no agenesis of the corpus callosum[2,5-8]. Among these cases, only four exhibited documented epileptiform activity on EEG monitoring[4-5,9] (Table 1). However, it should be noted that a significant number of cases did not explicitly mention whether epilepsy had been definitively ruled out. This uncommon association and its physiopathological implication will be further discussed below.
Table 1. Characteristics of the cases without brain malformation and confirmed epilepsy. TBI: traumatic brain injury
Furthermore, other associated conditions have been described in relation to SPH[2,10]. These conditions include multiple sclerosis, diverse neurological insults, HIV infection, SARS-CoV-2 infection and vaccination[7,8], and various other factors. The presence of these associated conditions adds to the complexity of the disease.
Physiopathological mechanisms
Several hypotheses have been proposed to elucidate the mechanism underlying this condition; however, the precise aetiology remains elusive. Among the hypotheses, the most favoured one is the ‘set point theory', which suggests a dysregulation of the hypothalamic thermostat, leading to the initiation of thermolysis through sweating, followed by thermogenesis through shivering[2]. This theory posits that hypothalamic dysfunction plays a central role in the development of SPH. Hypothalamic lesions resulting from various aetiologies, such as structural abnormalities, vascular insults or immune-mediated processes, have been postulated to contribute to the broad spectrum of clinical presentations observed in SPH. These lesions may disrupt the intricate regulation of body temperature, thereby leading to the manifestation of hypothermic episodes. While imaging studies have not consistently identified hypothalamic lesions in the majority of cases, it is important to consider the potential involvement of the hypothalamus in the pathogenesis of SPH and its associated conditions.
Recent clinical observations have provided further support for the set point theory. A noteworthy case involves a woman diagnosed with Shapiro syndrome variant, whose symptoms significantly worsened following a mild COVID-19 infection[7]. This observation suggests a potential link between COVID-19 infection and the exacerbation of hypothalamic dysfunction. It has been demonstrated that SARS-CoV-2 or its reactive inflammation can invade the hypothalamus through the olfactory tracts, thus might contribute to the disruption of thermoregulatory mechanisms. Furthermore, another case report described the development of Shapiro variant symptoms following vaccination against SARS-CoV-2[8]. These emerging cases highlight the need for further investigation into the potential interactions between viral infections, vaccination and the hypothalamic dysfunction observed in SPH.
While epilepsy has been considered as a potential causal mechanism in SPH this theory lacks robust support, primarily due to the typically normal findings on ictal and interictal electroencephalogram (EEG) recordings and the limited effectiveness of anti-epileptic treatments. However, it is important to note that the occurrence of epilepsy, as observed in our cases, is not entirely incompatible with the set point theory. Some authors have proposed that epileptic activity could directly propagate and involve the hypothalamus, suggesting a possible association between SPH and epileptic involvement of the hypothalamus[9,11]. This connection is particularly significant in the context of our presented cases, which demonstrate epileptic activity on EEG. Although further research is warranted to elucidate the precise relationship, these findings contribute to our understanding of the complex interplay between SPH, epilepsy and the hypothalamic dysfunction underlying the set point theory.
Another hypothesis proposes a potential association between SPH and cerebral neurotransmitter disorder. Abnormal levels of serotonin and dopamine metabolites in the cerebrospinal fluid of two paediatric patients support this hypothesis[6]. However, further research is needed to validate this hypothesis conclusively.
CONCLUSION
In summary, our case report presents two unique cases of SPH without agenesis of the corpus callosum, highlighting the broader spectrum of manifestations within the Shapiro syndrome variants. Importantly, both cases showed confirmed presence of epilepsy, which is a rare finding in SPH. These findings contribute valuable insights into the association between SPH and epilepsy, expanding our understanding of this rare condition and its underlying mechanisms. Further research is needed to explore the complex interplay between SPH, epilepsy and hypothalamic dysfunction.