ABSTRACT
We present a case of thyrotoxic periodic paralysis (TPP) presenting with stroke symptoms as a harbinger of Grave’s disease. A 61-year-old female presented with symptoms of abdominal pain and fatigue two weeks prior to admission and reported acute diarrhoea and unintentional weight loss. Investigation revealed thyrotoxicosis with undetectable thyroid stimulating hormone (TSH), elevated free T4 and elevated thyroid stimulating immunoglobulin (TSI). On the third day of admission, while undergoing physical therapy, code stroke was called on account of the onset of right-side predominant acute flaccid paralysis of upper and lower extremities, right-side facial droop, dysarthria and hyporeflexia bilaterally. The patient was alert and fully oriented with stable vitals with no increased labour in breathing at room air. An emergent head and neck CT, angiography, and magnetic resonance imaging (MRI) were negative. Serum potassium was 2.7 mmol/l, requiring prompt replacement. The patient’s paralysis and dysarthria improved over the following three days with a complete reversal of symptoms following the correction of serum potassium. Thyrotoxic periodic paralysis can occur in association with any of the causes of hyperthyroidism. It is due to a significant intracellular shift of potassium, subsequently manifesting clinically with hypokalaemia and muscle paralysis.
LEARNING POINTS
- Hypokalaemic periodic paralysis is an acute flaccid paralysis secondary to hypokalaemia, triggered by hyperthyroidism, environmental elements such as a high carbohydrate intake or rest after intense exercise, and an underlying genetic component with mutations in the muscle ion channels.
- The pursuit of code stroke protocol in the in-patient setting must bear in mind reversible but potentially fatal and disabling alternative diagnoses such as stroke mimics including hypokalaemic periodic paralysis.
- Stroke mimics defined as acute onset neurological deficits that are not related to vascular cause are a true challenge, multiple scales have been created to distinguish them from an actual stroke, such as the Recognition of Stroke in the Emergency Room (ROSIER) scale.
KEYWORDS
Hypokalaemic periodic paralysis, thyrotoxic periodic paralysis, thyrotoxicosis, pseudo stroke, stroke mimics
INTRODUCTION
Hypokalaemic periodic paralysis represents an acute flaccid paralysis secondary to hypokalaemia[1] that is often precipitated by resting after excessive exercise, fasting or high-carbohydrate meals[3]. The underlying aetiologies include inherited muscle ion channelopathies or thyrotoxicosis. The syndrome typically does not affect consciousness and may involve the bulbar or respiratory muscles. Few cases of cardiac arrhythmias have been reported. The clinical semblance to acute stroke poses a challenging race against time to diagnostically evaluate and intervene to avoid complications and disability. We present a case of thyrotoxic periodic paralysis (TPP) presenting with stroke symptoms as a harbinger of Grave’s disease.
CASE DESCRIPTION
A 61-year-old African American female with extensive cardiovascular history and insulin-dependent diabetes mellitus presented to the emergency department with initial symptoms of abdominal pain and fatigue two weeks prior to admission. She reported acute diarrhoea and unintentional weight loss. The initial evaluation demonstrated hypertension of 173/105, tachycardia at 131 and a non-acute but tender abdomen. The remainder of the physical exam was negative.
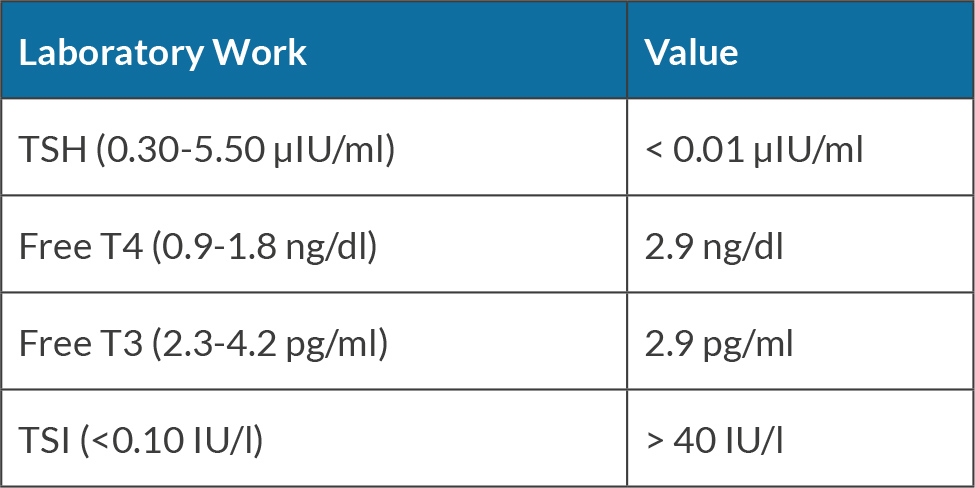
Investigation revealed biochemical thyrotoxicosis (Table 1) with undetectable thyroid stimulating hormone (TSH), elevated free T4 and elevated thyroid stimulating immunoglobulin (TSI). Computed tomography (CT) of the abdomen and pelvis showed mild diffuse colonic wall thickening. Stool leukocytes, ova, parasites, and cultures were unremarkable; however, the patient tested positive for Clostridium difficile toxin requiring initiation of oral vancomycin, beta-blockers and antithyroid medications.
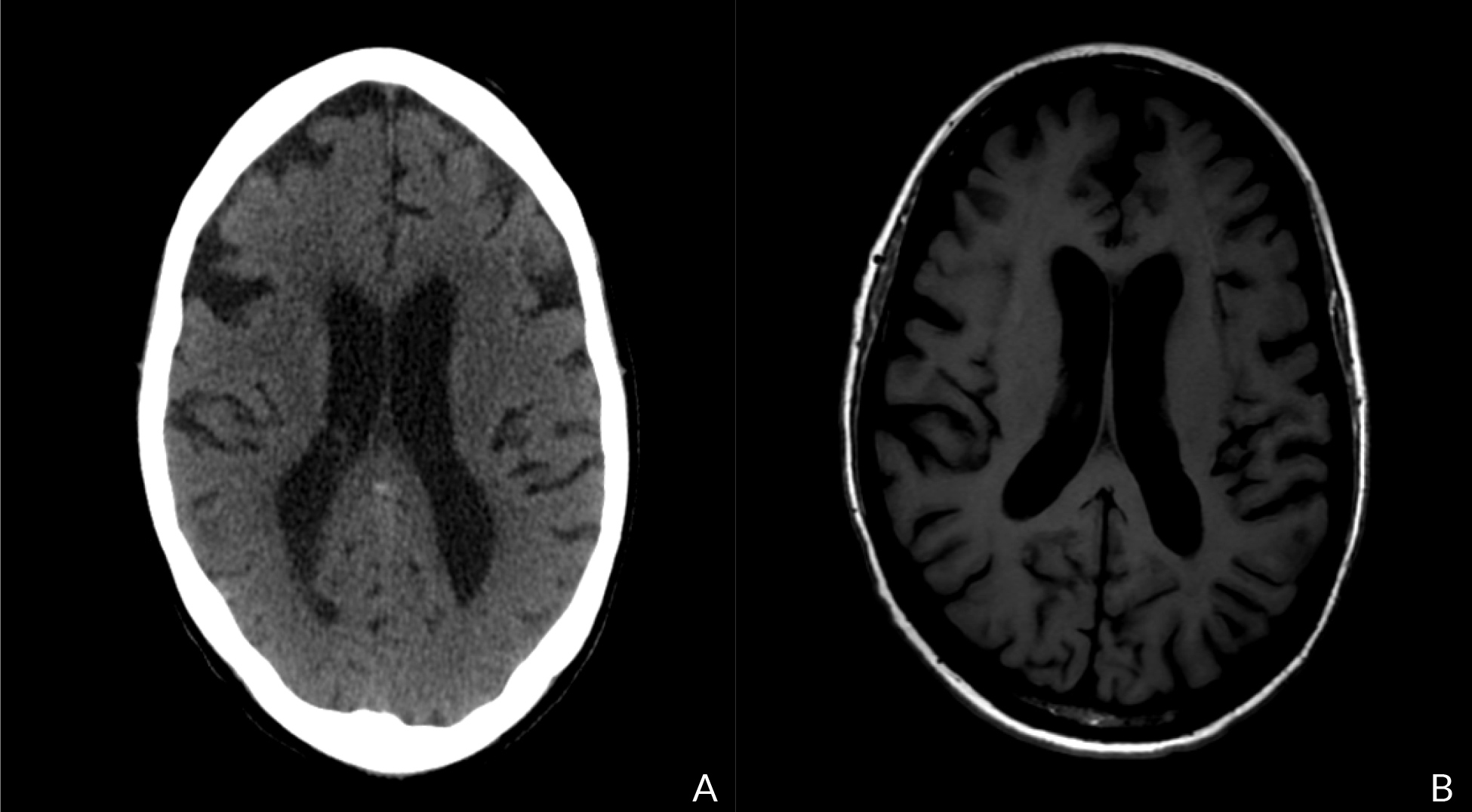
On the third day of admission, while undergoing physical therapy, code stroke was called on account of the onset of right-side predominant acute flaccid paralysis of upper and lower extremities, right-sided facial droop, dysarthria and hyporeflexia bilaterally. The patient was alert and fully oriented with stable vitals and no increased labour in breathing at room air. A head and neck non-contrast CT, angiography and magnetic resonance imaging (MRI) (Fig. 1) were negative for acute intracranial haemorrhage, midline shift or mass effect. No major arterial distribution of acute infarct or large vessel occlusion was seen. There were chronic changes of mild diffuse cerebral volume loss.
Figure 1. CT head without contrast (A) and MRI negative for acute intracranial bleed, midline shift or mass effect (B). No major arterial distribution acute infarct. There are changes of mild diffuse volume loss
Serum potassium was 2.7 mmol/l, requiring prompt oral and parenteral replacement. The patient’s paralysis and dysarthria rapidly improved over the following three days resulting in a full reversal of symptoms with the correction of serum potassium. There was no evidence of arrhythmic changes on the electrocardiogram (EKG). However, there was an inverted T wave in the inferior lateral leads as well as a prolonged QTc duration related to hypokalaemia (Fig. 2). Troponins remained normal as were creatinine kinase (CK) and liver function tests. Electroencephalography (EEG) reported essentially normal awake findings. Subsequently, the antithyroid medication was adjusted to optimise hyperthyroid symptoms based on the initial TSH. The patient was later discharged to outpatient rehabilitation.
Figure 2. EKG with inverted T wave in the inferior-lateral leads as well as a prolonged QTc duration. No evidence of arrhythmic changes
DISCUSSION
A call for code acute stroke represents a race against time for focused diagnostic evaluation, imaging, and appropriate interventions to avoid stroke-related mortality and disability. Similarly, identification of hypokalaemic periodic paralysis and prompt correction of serum potassium will not only reverse motor weakness but reduce the risk of respiratory compromise due to diaphragmatic paralysis and fatal cardiac arrhythmias.
Thyrotoxic periodic paralysis (TPP) is a complication of hyperthyroidism that is not very common. It can occur in association with any of the causes of hyperthyroidism, the most common of which is Graves disease[1]. TPP is frequently mentioned in the medical literature to be mainly affecting the East Asian male population[1,2,4]; cases of TPP in the African American male population are rare, and it is much rarer in African American females. It usually occurs in middle age compared to the familial form, which generally occurs in the early teenage years[1] and is passed on in an autosomal dominant form[4]. The attacks are indistinguishable between thyrotoxic and familial forms. Prodromal symptoms that are often missed and blamed on other reasons include muscle pain, cramping and stiffness. It is due to a significant intracellular shift of potassium subsequently manifesting clinically with hypokalaemia and muscle paralysis[2]. Recent data suggest that the condition is due to a combination of factors including hyperthyroidism, environmental elements such as a high carbohydrate intake or rest after intense exercise, and an underlying genetic component with mutations in the muscle ion channel, which eventually lead to increased activity of the sodium-potassium adenosine triphosphatase (Na+/K-ATPase) pump[1-5]. Our patient with hyperthyroidism and the occurrence of the attack shortly after physical therapy supports these findings. The Na+/K+-ATPase pump is also activated with insulin, which can explain the relationship between an acute attack and high-carbohydrate meals[5]. Other studies have suggested other mechanisms for the attacks other than potassium such as low phosphorus levels, and abnormalities in calcium and magnesium[5]. However, those were not frequently reported. Heart dysrhythmias as well as EKG changes related to hypokalaemia such as ST segment depression, QT interval prolongation, U waves and T-wave flattening are common. Atrial arrhythmias were reported to be the most common; however, ventricular arrhythmias such as ventricular fibrillation have been documented[4]. Restoration of normal sinus rhythm usually occurs with the treatment of hypokalaemia.
The traditional treatment of a severe attack is immediate intravenous or oral potassium chloride administration to hasten muscle recovery, and to prevent cardiac arrhythmia and respiratory arrest while monitoring for rebound hyperkalaemia[2,4]. After managing the acute attack, controlling and maintaining a euthyroid state in those patients can prevent recurrence[2,4]; thus, education about medication compliance and avoidance of the precipitating factors should be provided and reinforced strongly. Definitive treatment of hyperthyroidism such as radioactive iodine or thyroidectomy can be pursued after stabilisation of patients.
The acute onset of paralysis in the setting of hypokalaemia and thyrotoxicosis, and improvement in motor symptoms with correction of hypokalaemia, supported the diagnosis of thyrotoxic hypokalaemic periodic paralysis. Stroke mimics, which are defined as acute onset neurological deficits not related to vascular aetiology, are a true challenge that physicians encounter to differentiate between them and can lead to unnecessary medical interventions that can cause harm rather than benefit. Multiple stroke scales have been created to aid physicians in their quest for an accurate diagnosis. In a cohort study that was conducted to evaluate stroke mimics in patients presenting with sudden neurological deficits, 27.4% were related to peripheral vestibular disorder, followed by psychogenic causes[6]. Other conditions that can be included in the stroke mimics are disturbances in blood glucose, electrolyte imbalance, uraemia, migraine and seizures[6].
Conditions that mimic stroke include metabolic disorders such as hypoglycaemia, hyperglycaemia, hypernatraemia, hyponatraemia, uraemia, metabolic encephalopathy and hyperthyroidism[4,6-8]. Other conditions that might also mimic stroke are migraine, seizures, psychological disorders, demyelinating diseases, and brain tumours.
In a systematic review and meta-analysis of the famous validated scales used to identify stroke, it is reported that in an emergency department setting using the Recognition of Stroke in the Emergency Room (ROSIER) tool should be the scale of choice due to its high sensitivity (88% with a 95% confidence interval of 84% to 91%)[7]. In our patient, although that scale was not used as the patient was in an in-patient setting during the event, she would have scored a 4, indicating a possible stroke.
The pursuit of code stroke protocol in the in-patient setting must bear in mind reversible but potentially fatal and disabling alternative diagnoses including thyrotoxic hypokalaemic periodic paralysis to avoid risks of respiratory compromise and fatal cardiac arrhythmias. Knowledge about stroke mimics can prevent further morbidity and mortality in patients.