ABSTRACT
Varicella-zoster virus (VZV) commonly causes benign skin manifestations in children; it then establishes a latent infection and may reactivate, causing herpes zoster. The most common zoster complication is postherpetic neuralgia, but complications can also occur without a rash. VZV infection may cause neurological manifestations and even vasculopathy may occur, in both primary and reactivated VZV infection. Thrombotic complications are mainly described in children, while a few case reports have described cerebral venous sinus thrombosis (CVST), deep-vein thrombosis of the lower limbs and pulmonary embolism in adults. In this article we report the case of a young woman who developed systemic thromboembolic sequelae due to a hypercoagulable state following VZV reactivation. She had deep venous lower-limb thrombosis extended to the inferior vena cava (IVC), massive pulmonary embolism and CVST. Moreover, VZV reactivation caused an acute hepatitis and clinical manifestations suggesting viral encephalitis.
LEARNING POINTS
- Varicella-zoster virus (VZV) commonly causes self-limiting skin manifestation, but even neurological manifestations and thrombotic complications may occur.
- Only few isolated cases of VZV-related cerebral venous sinus thrombosis (CVST) and other types of deep-vein thrombosis have been reported in adults.
- Early diagnosis of VZV-related thrombosis and prompt anticoagulant and antiviral therapy can prevent a potentially fatal outcome and produce a good prognosis.
KEYWORDS
Varicella-zoster virus, zoster sine herpete, cerebral venous sinus thrombosis, pulmonary embolism, encephalitis
INTRODUCTION
Varicella-zoster virus (VZV) is a double-stranded DNA alpha herpes virus, which commonly causes benign skin manifestation in children, known as chickenpox. Then the virus establishes a latent infection, by retrograde migration to the sensory neuron body of the ganglion[1]; it may reactivate and cause herpes zoster by reaching the skin via anterograde axon transport[1]. The most common zoster complication is the chronic pain of postherpetic neuralgia, but complications can also occur without a rash (zoster sine herpete) and lead to ocular disorders, and visceral and gastrointestinal diseases (including ulcers, hepatitis and pancreatitis)[2].
Although VZV infection is typically benign in children, the adult onset is associated with increased morbidity. Both varicella and herpes zoster may cause neurological manifestations including encephalitis, meningitis, Ramsay Hunt syndrome, cerebellitis, myelitis and stroke-related syndromes[3]. Even vasculopathy may occur in both primary and reactivated VZV infection: clinical presentation may be highly variable including ischaemic and haemorrhagic stroke, cerebral aneurysm, temporal artery involvement, arterial dissection, cerebral venous sinus thrombosis (CVST), and spinal and peripheral artery thrombosis[4].
Thrombotic complications are mainly described in children, while they are very rare in adults. A few isolated case reports of CVST, deep-vein thrombosis of the lower limbs and pulmonary embolism have been reported in adults[5-8].
CASE PRESENTATION
A 37-year-old woman referred to Spedali Civili's Emergency Room (ER) in Brescia (Italy) for the onset of fever, refusal to eat or drink, and psychomotor impairment for a few days. She had a history of bipolar disorder, was recently diagnosed after a psychiatric hospitalisation with an episode of psychosis and treated with lithium, and she had an oestro-progestins vaginal ring.
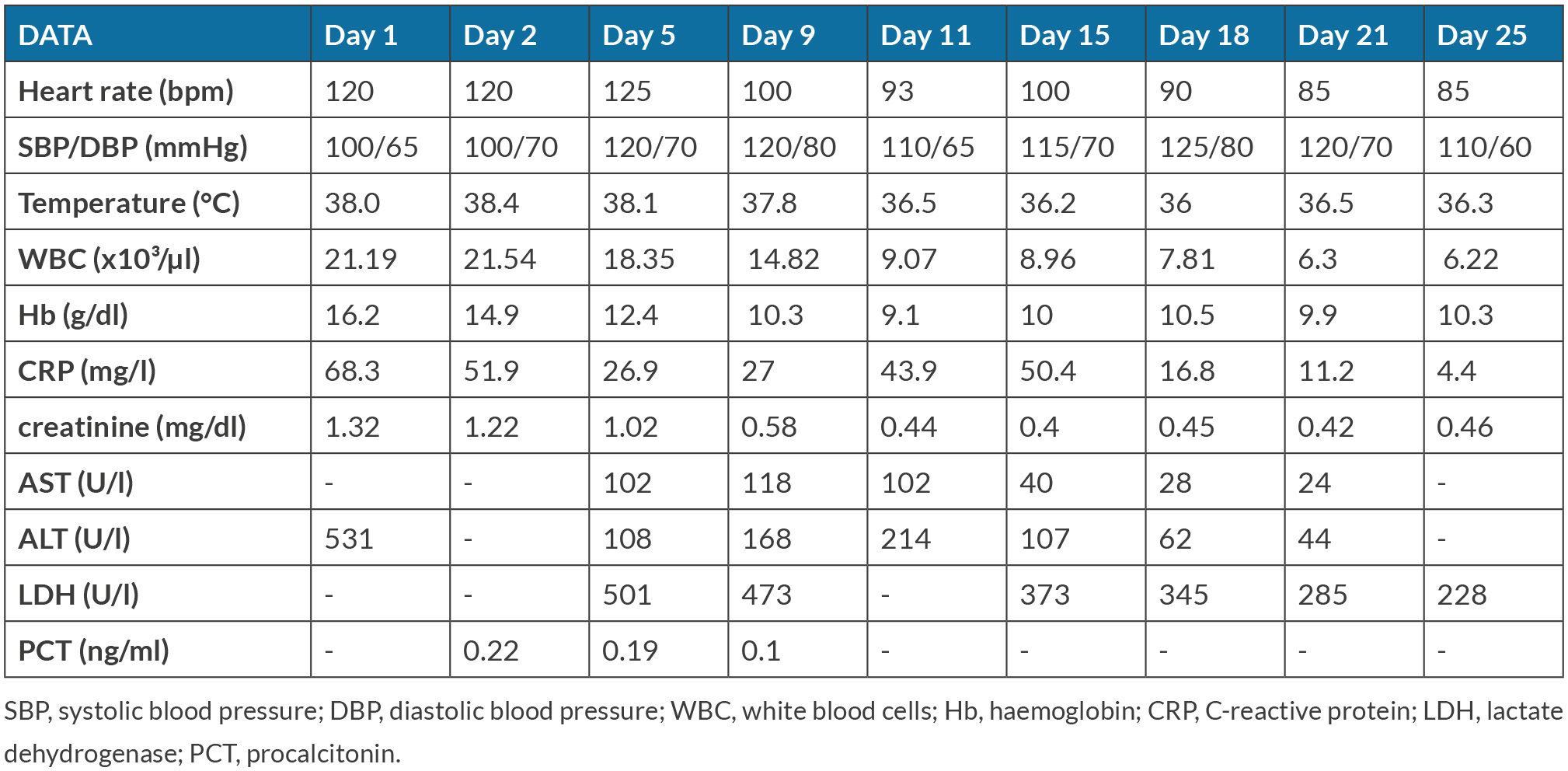
At ER admission an increase of C-reactive protein, abnormal liver function, haemoconcentration, hypernatriemia and a pre-renal acute kidney injury were detected. According to the neurological status, lithiemia was tested and lithium poisoning was excluded. Vital signs and laboratory parameters are reported in Table 1.
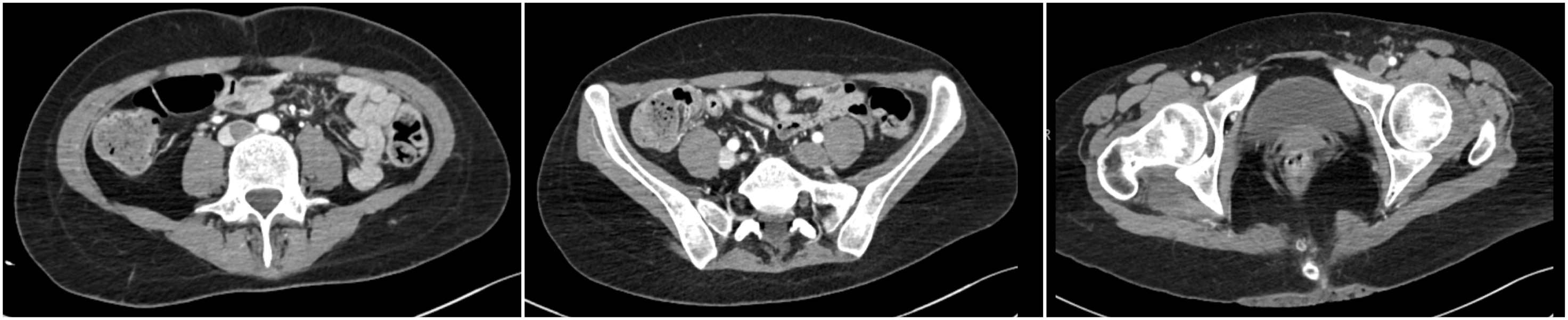
A computed tomography (CT) with contrast agent of the abdomen was performed because of a mild abdominal pain. This showed IVC thrombosis, occlusive thrombosis of the left lower-limb venous system and a focal right common femoral vein thrombosis (Fig. 1).
CT imaging was extended to the chest and a bilateral massive pulmonary embolism was identified (Fig. 2). During echocardiography biventricular function was normal, without right ventricular dilatation.
Table 1. Patient’s clinical and laboratory parameters over the hospitalization period
Figure 1. CT scan with contrast agent of the abdomen performed in the Emergency Room: inferior vena cava thrombosis and deep venous lower-limb thrombosis
Figure 2. Chest CT scan with contrast agent performed in the Emergency Room: massive pulmonary embolism
Antithrombotic therapy with enoxaparin 6000 IU bid (patient's weight 60 kg) was immediately started and the patient was hospitalised; the oestro-progestins vaginal ring was then removed. Empirical antibiotic therapy with ceftriaxone was added; results from blood cultures (carried out before starting the antibiotic therapy) were negative.
The prolonged psychomotor impairment was further investigated by electroencephalogram, which described the presence of non-epileptiform abnormalities with slow central-anterior waves, and by magnetic resonance imaging (MRI) which revealed CVST involving the superior sagittal sinus, right lateral sinus and right internal jugular vein. A rachicentesis could not be performed because of the ongoing anticoagulant therapy.
Differential diagnoses of multiple deep venous thrombosis were evaluated. Results of thrombophilia tests were negative for factor V Leiden or prothrombin mutation; levels of protein C, protein S and homocysteine were normal. Autoimmunity diseases were ruled out by finding normal levels of anti-nuclear antibodies and by excluding antiphospholipid syndrome. Moreover, myeloproliferative disorders were excluded: JAK2 mutation and paroxysmal nocturnal haemoglobinuria were absent.
Results from a positron emission tomography were negative for vasculitis. Among the risk factors associated with venous thromboembolism, only the oestro-progestin therapy (promptly removed at admission) was present in our patient. Even dehydration could have played a role in the onset of thrombosis.
In summary, our patient was affected by acute hepatitis, neurological clinical manifestations suggesting encephalitis, multiple deep venous thrombosis and persistent fever, despite antimicrobial therapies. Since the unifying diagnosis could have been a viral infection, intravenous acyclovir was started empirically and specific serological examinations were performed. At the same time, the antibiotic therapy was stopped.
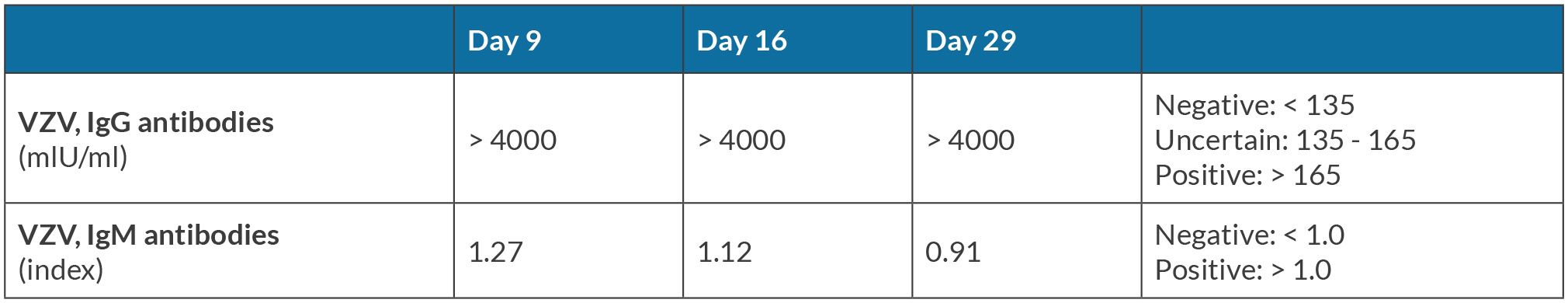
Serology confirmed a VZV reactivation, detecting a level of anti-VZV IgG antibodies over the upper limit of normal and a slight increase in IgM titre. Serology was repeated during the hospitalisation, as reported in Table 2: the IgG level remained over the upper limit of detection and the IgM titre progressively became negative, as described in the literature, during VZV reactivation[9]. Our patient had been extensively studied to find possible conditions that could have caused VZV reactivation. Among the risk factors described in the literature[10] that were related to VZV reactivation, including age over 50 years, immunocompromised status, immunosuppressive drugs and infections, only mental stress was present in our patient. Our patient had a history of bipolar disorder, recently diagnosed after a psychiatric hospitalisation for an episode of psychosis, and her husband described the period before hospital admission as especially stressful due to the diagnosis of psychiatric disorder and the therapy undertaken.
Table 2. Varicella-zoster virus (VZV) serology during the hospitalization period by chemiluminescence immunoassay (CLIA)
The patient clinically improved after the introduction of antiviral therapy and the discontinuation of antibiotic therapy: she no longer had fever and she gradually showed a neurological improvement, which allowed her to start physiotherapy treatment. Biochemical examinations (including transaminases, white blood cell count and C-reactive protein) started to normalise (see Table 1) and a brain MRI described partial CVST recanalisation.
Acyclovir was administered over a three-week period and antithrombotic treatment was shifted from enoxaparin to direct oral anticoagulant (apixaban 5 mg bid). The patient was discharged after about 35 days of hospitalisation, with indications for anticoagulation follow-up. A venous echo-colour Doppler, performed three months after discharge, revealed a partial recanalisation of venous lower-limb thrombosis. She is now receiving long-term anticoagulant therapy and she recovered her normal neurological status.
DISCUSSION
This article describes the case of a patient affected by an atypical VZV reactivation. She had a zoster sine herpete, with systemic thromboembolic sequelae, acute hepatitis and clinical manifestations suggesting viral encephalitis.
Our patient's laboratory and radiological examinations showed the viral infection as the unique cause of both fever and hepatitis; VZV is known to cause hypercoagulable states leading to thrombotic complications[6]. The entrapment resulting from the altered mental status and the oestro-progestins vaginal ring may have contributed to the hypercoagulable state.
Thrombotic complications are mainly described in children[6], but a few isolated cases of VZV-related CVST and other deep-vein thromboses have been reported in adults[7,11-13]. The first case report of pulmonary embolism associated with zoster sine herpete was described by Sahra et al. in 2021[14].
The exact pathogenetic mechanism of venous thrombosis following VZV infection is not completely known. The postulated theories include vasculitis, direct endothelial damage and acquired protein S deficiency secondary to molecular mimicry[6,15].
Josephson et al. showed that 43 out of 95 children included in a cross sectional study had antiphospholipid antibodies and some of them had a reduction in protein S levels post varicella infection[16].
Transient reduction in natural anticoagulants levels may rarely appear in adults with VZV infection, thereby contributing to thromboembolic phenomena[5].
Sudhaker et al. described one patient affected by CVST with transient low protein S levels and positive antiphospholipid antibodies, normalised after a six-month period[5]. Siddiqi et al. reported two cases of CVST with low protein S and C levels after primary VZV infection[13].
In any case, the frequency by which antibodies to S proteins are induced is unknown. Our patient was extensively studied for possible prothrombotic underlying diseases, but the diagnostic workup produced negative results. This underlines the importance of further studies on pathogenetic mechanisms.
As far as treatment is concerned, VZV-associated vasculopathy is traditionally treated with intravenous acyclovir, and a prompt anticoagulation can prevent a potentially fatal outcome[14]. Early diagnosis and management help to prevent associated morbidity and mortality, and produce a good prognosis[6,8].
This case report is aimed to raise awareness on rare VZV infection manifestations and to underline the importance of clinical multidimensional evaluation to recognise and promptly treat the disease. Better insight into possible mechanism responsible for development of VZV-related thrombosis would improve these patients' management.