ABSTRACT
Legionnaire's disease can cause rare and severe complications such as rhabdomyolysis and acute kidney injury. This case report details a 45-year-old male patient who presented with features of Legionnaire's disease. Laboratory results showed a significantly elevated serum creatinine kinase level and an increased creatinine level. Imaging showed right lower lobe consolidation, and a positive urine antigen test confirmed Legionnaire's disease. The patient was administered azithromycin and underwent fluid repletion to manage the rhabdomyolysis and acute kidney injury, resulting in improved creatinine kinase levels and kidney function. He was discharged and continued on azithromycin for 10 days. His outpatient follow-up showed that creatinine kinase levels had further decreased. This case report emphasises the importance of early recognition and management of Legionnaire's disease and its rare but severe complications.
LEARNING POINTS
- Legionnaire's disease is a severe form of pneumonia caused by Legionella bacteria that can lead to rare complications such as rhabdomyolysis and acute kidney injury, which have high morbidity and mortality rates.
- The treatment for Legionnaire's disease complicated with rhabdomyolysis and acute kidney injury involves early fluid repletion, antibiotics and close monitoring of creatinine kinase levels, electrolytes and kidney function.
- For patients with creatinine kinase levels over 5000 U/l without hypocalcaemia or alkalaemia, urinary alkalinisation with bicarbonate therapy may be considered as a treatment option.
KEYWORDS
Legionnaires' disease, rhabdomyolysis, acute kidney injury
CASE PRESENTATION
The patient was a 45-year-old white male who presented with a one-week history of chills, a non-productive cough, dyspnoea on exertion, malaise, lack of appetite, watery diarrhoea and generalised myalgia. He had no headache, vomiting or abdominal pain. His symptoms had progressively worsened to the point where he felt unable to get out of bed, prompting him to seek immediate medical attention at the Emergency Department.
The patient had a past medical history of hypertension and hyperlipidaemia. He was an alcohol user, consuming two hard liquor drinks per day, and was an active smoker with a 30-pack-year smoking history. However, he had not consumed alcohol or smoked in the past week due to his illness. He lived with his wife in his house and worked as a locksmith. His body mass index (BMI) was 29.4. Additionally, he had no sickness contact or recent travel history.
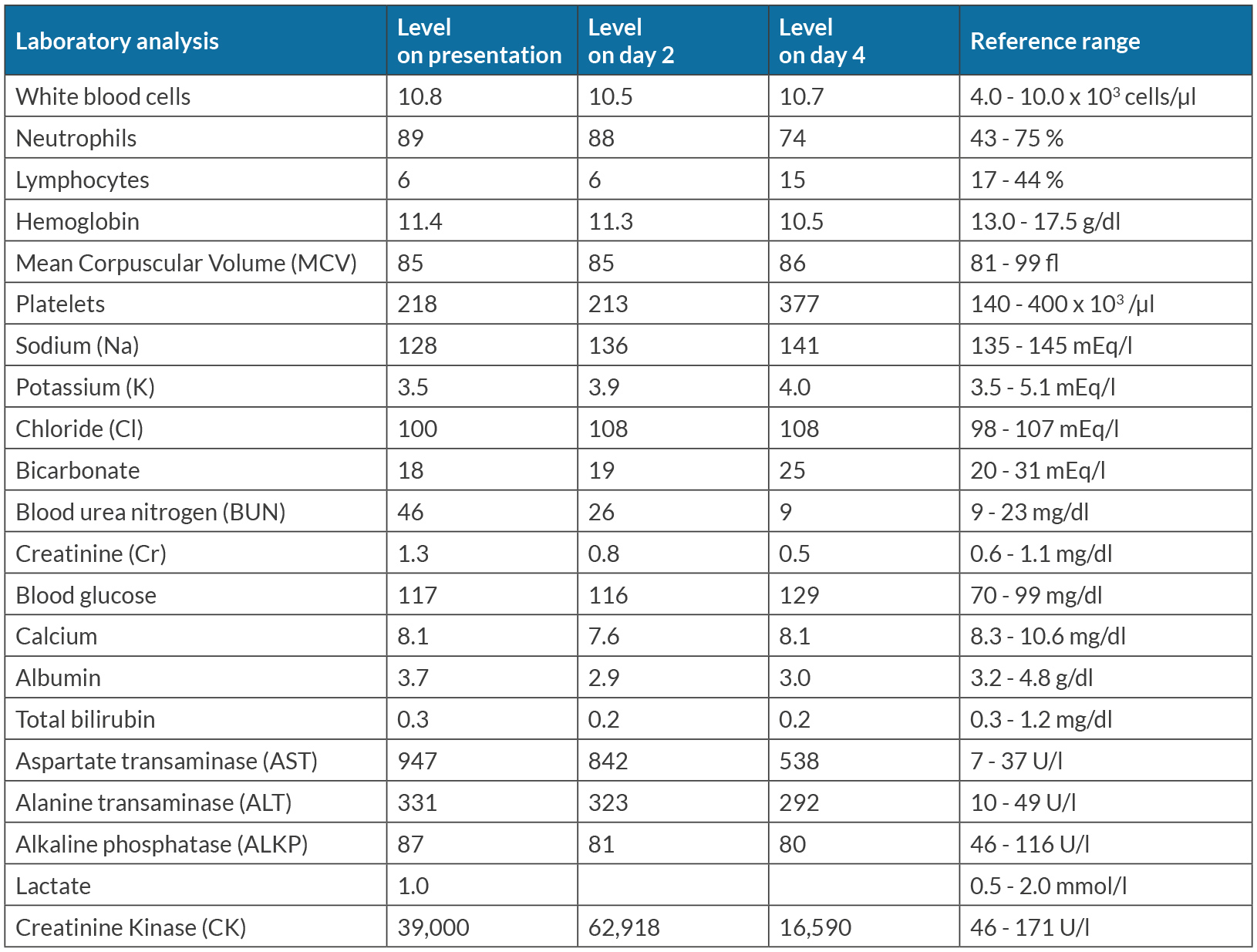
On examination, the patient was tachycardic at 110 bpm and tachypneic with a respiratory rate of 30. His blood pressure was 115/67 mmHg, and oxygen saturation was 92% on room air. He was febrile with a temperature of 38.1˚C (100.6 ˚F). The patient appeared ill, had dry oral mucous membranes and rhonchi over the right lower lung. Lab tests revealed leukocytosis, hyponatraemia, azotaemia, transaminases, creatinine elevation and a serum creatine kinase (CK) level of 39,000 U/l (Table 1). An electrocardiogram showed sinus tachycardia, and a chest x-ray revealed right lower lobe consolidation concerning for pneumonia (Fig. 1). His liver ultrasound showed fatty infiltration of the liver but a normal gallbladder. His viral hepatitis panel, acetaminophen and alcohol levels were unremarkable.
The patient was given intravenous ceftriaxone and azithromycin for presumed community-acquired pneumonia. Lactated Ringer bolus was given and continued at a rate of 200 ml per hour for rhabdomyolysis and acute kidney injury. His Legionella urinary antigen test came back positive, and ceftriaxone was therefore discontinued. The patient's CK level continued to rise, with a peak level of 62,918 U/l. Bicarbonate was not given due to hypocalcaemia.
By the end of the second day, the patient's condition had improved with a resolution of fever, improved CK level at 35,263 U/l, improved liver function tests and resolved acute kidney injury. Lactated Ringer's solution was continued due to the persistent high level of creatine kinase. On the fourth day of hospitalisation, his shortness of breath and myalgia had resolved, and his CK level had decreased to 16,590 U/l. Blood cultures remained negative and the patient requested discharge. Oral hydration and a total 10-day course of azithromycin were recommended. One week after discharge, he remained stable and his CK level had further decreased to 449 U/l.
DISCUSSION
Legionnaire's disease is a severe form of pneumonia caused by Legionella bacteria. It typically presents with fever, cough, dyspnoea, muscle aches, gastrointestinal symptoms, hyponatraemia and elevated hepatic transaminases. Risk factors include men who aged over 50, smoking, chronic lung disease, immunocompromised state and recent travel history[1]. Diagnostic tests mainly include sputum culture, polymerase chain reaction (PCR) and urine antigen testing[1,2]. Sputum culture and PCR on a lower respiratory tract sample have high accuracy to detect all Legionella species and serogroups. However, it may be challenging to obtain an appropriate sputum sample, especially in patients with atypical pneumonia[2]. Urine antigen testing can be obtained concurrently or served as an alternative if other tests are not available, or if sputum cannot be obtained. It is more rapid and has a high specificity approaching 100% but detects only Legionella pneumophila serogroup 1, which comprises over 80% of reported cases[1,3]. However, if urine antigen testing is negative and Legionella infection is still suspected, PCR or culture should be sent for.
Our patient was a 45-year-old male who did not have any known risk factors for developing Legionnaire's disease, except for his smoking habit. However, he presented with typical symptoms of Legionnaire's disease, which prompted further workup with a urine antigen testing leading to diagnosis. Azithromycin or levofloxacin are the recommended antibiotics for treating Legionnaire's disease, but the optimal duration of treatment remains undetermined. Treatment duration may range from 3 to 21 days depending on factors such as the selected antibiotic, illness severity, immune status and clinical response[4].
Legionnaire's disease can rarely lead to rhabdomyolysis, a condition where muscle breakdown releases substances into the bloodstream that can cause electrolyte imbalances, elevated creatinine kinase levels and metabolic acidosis. The exact mechanism behind this is not fully understood, but it is believed to be due to a combination of bacterial endotoxins and direct invasion of the bacteria into the muscle tissue[5,6]. Overall, our patient did not have other significant risk factors for developing rhabdomyolysis, such as prolonged immobilisation, physical exertion, heat exposure, trauma, and use of lipid-lowering agents or illicit drugs. Although the patient had a history of alcohol use, he had completely abstained from drinking for a week prior to presentation. He reported a decrease in oral intake and mild watery diarrhoea (less than three episodes per day, with a mild to moderate amount), which could potentially be contributing factors increasing the likelihood of rhabdomyolysis. However, considering the amount and frequency of his diarrhoea, we believe that the level of dehydration would not have been severe enough to be the primary cause of rhabdomyolysis. Instead, Legionella infection is more likely to be the main contributing factor in his condition.
Patients with Legionnaire's disease and rhabdomyolysis are also at risk of acute kidney injury (AKI), with up to 55.5% of cases requiring dialysis and a mortality rate of 51% compared to 15% in patients without AKI[7]. The mechanism of AKI is likely due to the accumulation of myoglobin in the renal tubules and renal vasoconstriction[8]. Direct invasion of bacteria into renal tissue may also contribute to AKI in cases of rhabdomyolysis caused by Legionnaire's disease[7].
Early recognition and management of rhabdomyolysis is crucial in preventing irreversible kidney injury and the need for dialysis. The mainstay of prevention is early volume resuscitation with crystalloid fluids, which should be continued until the patient's CK levels decrease to less than 5000 U/l. Studies have shown that a CK level below 5000 U/l has a lower risk of AKI[8,9]. Urinary alkalinisation with bicarbonate therapy may be considered as a treatment option for patients with CK levels over 5000 U/l to prevent renal impairment, provided they have no hypocalcaemia or alkalaemia[8,10]. However, its effectiveness is uncertain, and bicarbonate was not administered in this case due to hypocalcaemia.
The patient's early diagnosis of Legionnaire's disease, rhabdomyolysis and AKI allowed for prompt management with azithromycin and early fluid repletion. This led to a significant reduction in CK levels and resolution of his symptoms and AKI within 4 days. Since the patient requested discharge, we did not continue intravenous fluid repletion until his CK level decreased to less than 5000 U/l. Instead, we recommended oral hydration and a 10-day course of azithromycin, and monitored his CK levels on an outpatient basis. A sustained improvement was observed, with CK levels decreasing to 449 U/l one week after discharge.
CONCLUSION
We report on a case of Legionnaire's disease with rare complications of rhabdomyolysis and acute kidney injury, which may lead to high morbidity and mortality. Timely diagnosis and prompt treatment are crucial for better outcomes, and close monitoring is required.