ABSTRACT
The most common cause of vasoplegic shock in critical care is sepsis. However, although rarely and only in specifically sensitised individuals previously bitten by a tick, red meat may provoke a delayed allergic reaction called an alpha-gal syndrome. We present a case of a protracted life-threatening manifestation of alpha-gal syndrome, which, due to an unusual absence of typical features of anaphylaxis can masquerade as septic shock and calls attention to the premature diagnostic closure as a contributor to diagnostic error. Alpha-gal syndrome is a relatively new, but increasingly recognised health issue. We propose that alpha-gal syndrome should be considered in the differential diagnosis of vasoplegic shock of unclear aetiology even in the absence of typical allergic symptomatology and typical allergen exposure since alpha-gal is present in a wide variety of carriers.
LEARNING POINTS
- Alpha-gal syndrome, otherwise known as “red meat allergy”, is a potentially life-threatening allergic syndrome induced by the immunological properties of tick saliva.
- A typical case of alpha-gal syndrome is a patient bitten by a tick who develops an allergic reaction, anaphylaxis or anaphylactic shock even after an ingestion of a significant amount of alpha-gal, typically present in red mammalian meat or organs.
- As global warming continues, we may expect tick-borne diseases to spread wider around the globe and due to the possibility of complete absence of typical allergic symptomatology and the delayed onset of symptoms, this syndrome needs to be considered when encountering vasoplegic shock of uncertain origin.
KEYWORDS
Alpha-gal Syndrome, anaphylactic shock, sepsis mimics, meat allergy, tick allergy
INTRODUCTION
The most common cause of vasoplegic shock in critical care is sepsis. However, although rarely and only in specifically-sensitised individuals previously bitten by a tick, red meat may provoke a delayed allergic reaction called an alpha-gal syndrome. We present a case of a protracted, life-threatening manifestation of alpha-gal syndrome, which, due to an absence of typical features of anaphylaxis, can masquerade as a septic shock and calls attention to the premature diagnostic closure as a contributor to diagnostic error in a patient with severe vasoplegia in the emergency department.
CASE DESCRIPTION
A 68-year-old heavy smoker with no previous medical history and no known history of allergy or asthma was brought to the emergency department after an episode of near cardiac arrest and with persistent severe hypotension. On the day of admission, the patient had made spicy pork kidneys for a dinner. Approximately an hour later, he was found by his wife gasping on the armchair. Telephone-assisted cardiopulmonary resuscitation (CPR) was performed for 15 minutes. Upon the arrival of an ambulance, spontaneous circulation had already been restored, although the patient remained severely hypotensive requiring norepinephrine administration. On physical examination the patient was afebrile, tachycardic and tachypneic with an oxygen saturation of 85% while breathing room air. He was drowsy yet awake with Glasgow coma scale of 4-5-6. Auscultation of the heart failed to reveal any murmurs, lung sounds were clear, and the abdomen was soft with no tenderness or guarding. Skin examination did not reveal any efflorescence, although a tick embedded in the skin was extracted. Due to insufficient mechanics of breathing caused by CPR-associated rib fractures, mechanical ventilation was initiated.
An electrocardiogram showed sinus tachycardia without signs of acute ischaemia. Laboratory results came back with a white cell count of 14,700 per cubic millimetre with predominantly neutrophils; C-reactive protein was elevated to 64 mg/l with grey-zone procalcitonin (0.1 ng/ml). Renal functions and hepatic enzymes were normal, but lactate was markedly elevated (6.3 mmol/l). Bed-side echocardiography failed to reveal hypovolemia or any regional dyskinesis or akinesis, there were no signs of right ventricular strain or left ventricular outflow tract obstruction (LVOTO) – only high left ventricle ejection fraction consistent with hyperkinetic circulation. Whole-body CT showed only a consolidation of the lower lobe in the left lung, leading to suspicion of pneumonia.
While treating the patient empirically for pneumonia and septic shock, the medical team continued to obtain thorough history. His wife noted that her husband started to feel itches all over after eating his lunch. The precipitous speed of deterioration as well as the postprandial timing together with the additional information about itchy skin prompted us to seek an alternative diagnosis. Since protracted anaphylaxis had become a compelling unifying diagnosis, a serum tryptase sample was obtained, which came back significantly higher than normal (52.9 mcg/l; reference value is 11 under mcg/l) and total IgE levels were also elevated.
An investigation of the potential trigger left only two options – spices or pork kidneys. Taking into account the delay of the allergic reaction and the tick extracted on admission, we started to consider alpha-gal syndrome. We obtained specific IgE against alpha-gal which were highly positive (85 kIU/l, normal value 0.35 kIU/l). An allergologist consultation was requested, and the patient was diagnosed with alpha-gal syndrome as a causative factor of vasoplegic shock with rapid progression to cardiac arrest.
DISCUSSION
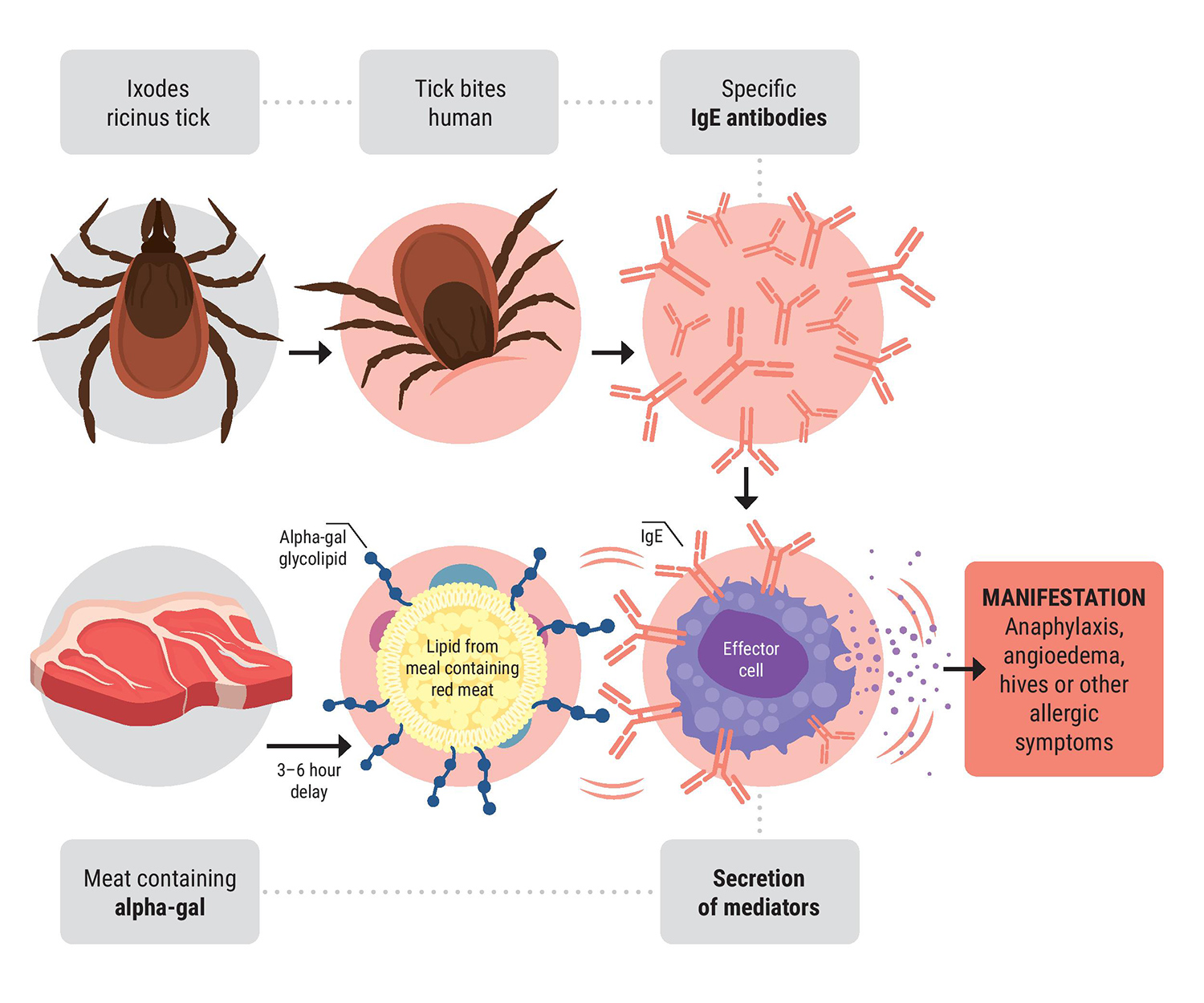
Galactose-alpha-1,3-galactose is a disaccharide expressed on glycoproteins and glycolipids of mammals, except Old World monkeys, apes and humans[1]. The immunological background behind the formation of specific IgE antibodies is not well understood. We now know that some species of ticks play a crucial role; their saliva contains a large spectrum of immunologically active substances that skew the adaptive immune response to the Th2 phenotype. The abundance of IL-4 then causes isotype switching to IgE antibodies production[2]. However, the majority of patients sensitiSed to alpha-gal will never develop the alpha-gal syndrome (Fig. 1).
A typical case of alpha-gal syndrome has an adult-life onset without any previous allergy-related problems. Clinical symptoms are usually delayed and start 3–6 hours after ingestion; some patients may experience the onset of symptoms in less than 2 hours[3]. The range of possible symptomatology is vast and includes not only typical allergic reactions, but also abdominal pain without skin involvement, anaphylaxis or anaphylactic shock as described in our case.
Diagnosis is mainly based on a history of eating red meat and detecting specific IgE antibodies. Prick tests with extracts of beef or pork are unreliable[4]. Not only is red (mammalian) meat a source of alpha-gal, it is also contained in milk and milk-based products, butter, sweets containing gelatine and some medicaments (mainly cetuximab). Treatment of acute allergic reaction does not differ from standard practice. All patients should know that any further tick bite can increase the titres of alpha-gal antibodies and worsen their allergy. At the same time, all patients are advised to avoid mammalian meat products from their diet altogether. Avoidance of dairy products and other mediators of alpha-gal mentioned above is not routinely advised although might be implemented in severe cases[5].
Our case report describes a life-threatening protracted delayed vasoplegic shock following animal organ consumption and a tick bite, which was initially mistaken for sepsis. Later on, with all dots connected, we recognised that the primary problem was a tick-borne anaphylaxis due to alpha-gal syndrome. To the best of our knowledge, there are no case reports on severe protracted anaphylaxis in this type of allergy. Alpha-gal is a potentially life-threatening syndrome to disaccharide galactose-alpha-1,3-galactose. The primary source of this IgE–binding epitope are mammalian products, but sensitisation to this antigen requires a tick bite. Typical cases present as a delayed anaphylaxis after red meat consumption but atypical clinical manifestation without common allergic symptomatology and trigger may occur, which can lead to diagnostic errors. We believe this case report has the potential to expand knowledge of this unusual cause of seemingly idiopathic anaphylaxis and vasoplegia and underscores how important is to avoid mental shortcuts in the diagnostic process. As tick-borne diseases tend to rise in incidence and prevalence for various reasons, we can expect the same phenomena in this yet rare syndrome.