ABSTRACT
A 57-year-old male with heart failure and decompensated alcoholic liver cirrhosis presented with recurrent haematochesia due to rectal varices. After multiple failed therapy with endoscopic band ligation and surgical sclerotherapy, a discussion with an interventional radiologist was arranged. A transjugular intrahepatic portosystemic shunt (TIPS) was deferred due to a history of heart failure. A shared decision to proceed with transhepatic Gelfoam® slurry embolisation with coiling was made. During the procedure, a variant anatomy of the superior rectal vein was identified. The superior rectal vein was found to drain directly into the left portal vein with no connectivity between the inferior mesenteric vein and the rectal varices. As planned, Gelfoam slurry embolisation and coiling was done to the left and right superior rectal vein along with the common trunk it drains. The patient did not develop any further episodes of gastrointestinal bleeding or worsening ascites on follow-up after 6 months. This case represents a successful treatment of bleeding rectal varices when TIPS is contraindicated.
LEARNING POINTS
- Rectal varices are an infrequent outcome of portal hypertension formed by portocaval anastomosis between the superior rectal vein with the inferior mesenteric vein of the portal system upstream, and the middle and inferior rectal vein draining into the internal iliac and internal pudendal vein of the systemic circulation, respectively. Portal system variations are extremely rare.
- Most common modality of recurrent rectal varices bleed is a transhepatic intrajugular portosystemic shunt. The absolute contraindications to this include congestive heart failure among others.
- In the presence of multiple co-morbidities and contraindication for TIPS, various interventional radiological modalities on a case-by-case basis are available including percutaneous transhepatic rectal varices obliteration.
KEYWORDS
Rectal varices, embolisation, varices coiling
CASE DESCRIPTION
A 57-year-old African American male presented to the interventional radiologist for elective ultrasound guided angiogram of the portal system due to recurrent rectal variceal bleed. He had a medical history significant for systolic heart failure on an automatic implantable cardioverter defibrillator, persistent atrial fibrillation, cardiac sarcoidosis, chronic kidney disease and decompensated cirrhosis. He had a long-standing history of decompensated alcoholic liver cirrhosis with rectal varices causing bleeding of the rectum, and multiple emergency department visits. Given the recurrent gastrointestinal bleed, anticoagulation therapy for atrial fibrillation was deferred. Rectal varices were treated with rubber band ligation of three varices 2 months previously, with rebleeding at 2 weeks post-procedure. Hence, he underwent sclerotherapy 3 weeks later following which he was free of bleeding, but started rebleeding after 3 weeks. A transjugular intrahepatic portosystemic shunt (TIPS) was deferred due to heart failure. The patient’s condition was discussed with interventional radiologists, and he was considered for evaluation with an elective ultrasound guided visceral angiogram.
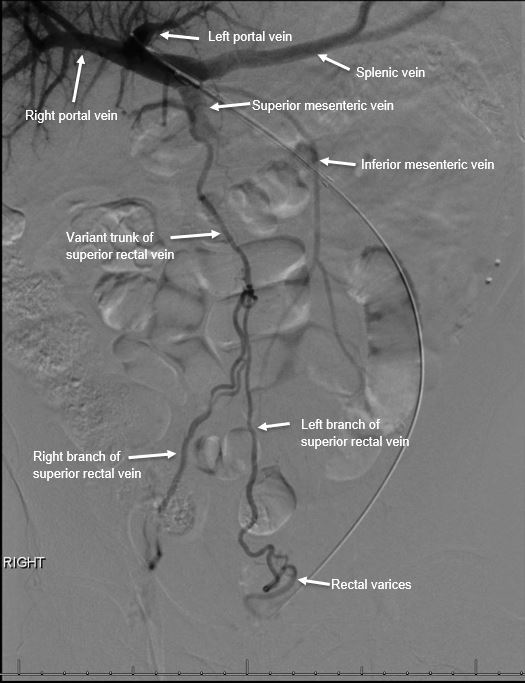
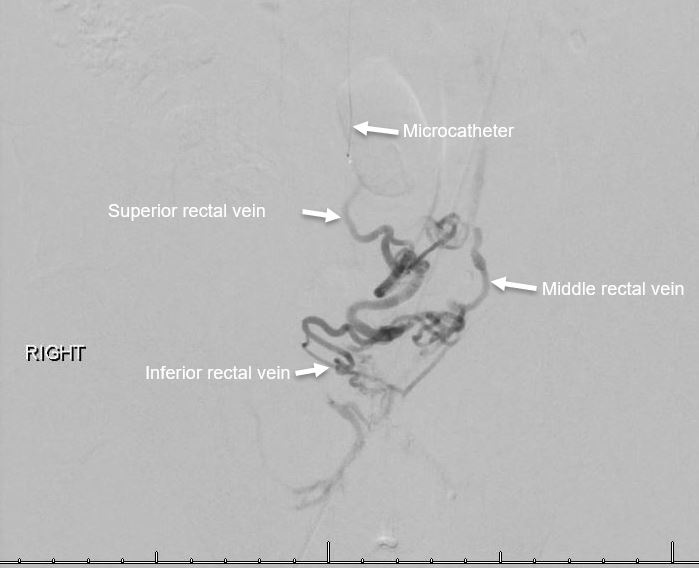
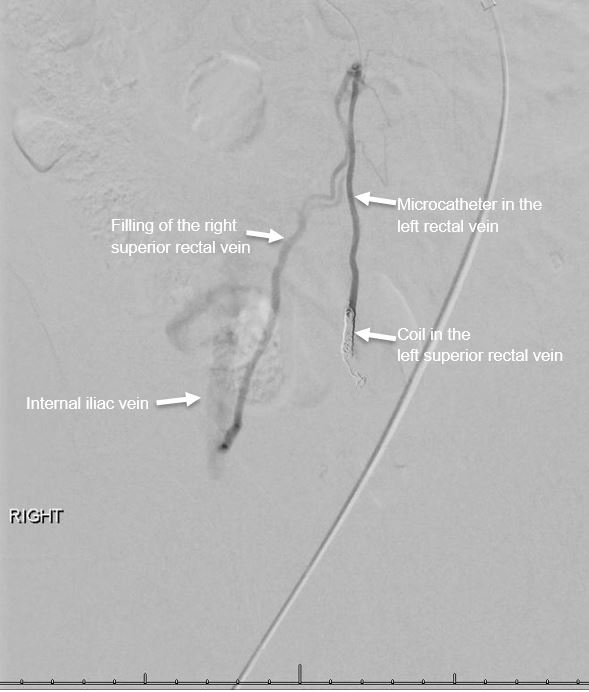
Through a percutaneous transhepatic approach, the left portal vein was accessed and an abnormal branch arising from it travelling caudally to supply the superior rectal vein, predominantly the left superior rectal vein, was identified (Fig. 1). It was also noted that the inferior mesenteric vein did not supply the superior rectal vein or the rectum. A venogram confirmed that the rectal varices arose from the superior rectal vein and drained into the middle and inferior rectal veins bilaterally (Fig. 2). The rectal varices were then embolised using Gelfoam slurry under continuous fluoroscopy until a significant reduction in the flow was noted. This was followed by embolisation of the left superior rectal vein with multiple detachable microcoils. A subsequent angiogram revealed complete cessation of the flow in the left superior rectal vein, with contrast refluxing to the right superior rectal vein (Fig. 3). The right superior rectal vein was then embolised with Gelfoam slurry with significant reduction in the flow, which was followed by embolisation of the common trunk vein supplying both the left and right superior rectal veins with multiple detachable coils. A post-coiling angiogram revealed complete occlusion of the flow to the bilateral superior rectal veins (Fig. 4). The vascular sheath in the left hepatic lobe was removed and the access tract embolised using a coil. The procedure was completed without any immediate complications. On follow-up at 6 months, the patient continued to be free of rectal bleeding, and without worsening of ascites.
Figure 1. Transhepatic portal venogram showing the trunk of the superior rectal vein arising from the left portal vein and its anatomy with other portal vessels
Figure 2. Venogram with microcatheter in the left superior rectal vein, showing the rectal varices formed by the superior rectal, middle rectal and inferior rectal veins
Figure 3. Venogram of the left superior rectal vein post coiling and Gelfoam slurry embolisation, showing absence of flow into the left superior rectal vein and reflux into the right superior rectal vein
Figure 4. Post-coiling angiogram showing complete occlusion of the flow to the bilateral superior rectal veins
DISCUSSION
Variceal bleeding is one of the life-threatening complications of increased portal hypertension from cirrhosis. The stomach and oesophagus are the most common sites of varices, accounting for approximately 50% of patients with liver cirrhosis. The varices at any other site of portocaval anastomosis are called ectopic varices[1]. Rectal varices are the most common site of ectopic varices[2]. In a study, the prevalence of rectal varices among patients with cirrhosis was found to be 44%[3]. Bleeding from rectal varices contributes to 1–5% of all variceal bleeding. Though the risk of life-threatening bleeding is low in rectal varices compared to gastroesophageal varices, recurrent bleeding increases mortality and morbidity.
Rectal varices are venous collaterals formed at the site of portosystemic anastomosis due to portal hypertension. When the portal pressure is high, blood flows from the portal system through the superior rectal vein into the systemic circulation through the middle and inferior rectal veins into iliac veins. Commonly, rectal varices occur in cirrhosis when intervention to gastroesophageal varices is done, which diverts the pressure towards other sites of portosystemic anastomosis. This is supported by the study conducted in Japan which reported that 94.8% of patients with rectal varices had oesophageal varices and 87% received endoscopic treatment for oesophageal varices[2]. Isolated rectal varices as such are rare.
In normal anatomy, the superior rectal vein continues as an inferior mesenteric vein, a tributary of the portal vein[4]. Anomalies of the superior rectal vein are sparsely reported. During the visceral angiogram, we identified that the superior rectal vein drains into the left portal vein, instead of draining into the inferior mesenteric vein. This variation could have possibly contributed to the recurrent variceal bleed without occurrence of other variceal bleed in this patient, as the portal pressure directly from the left portal vein can be high compared to that from the inferior mesenteric vein.
Unlike for gastroesophageal varices, there are no widely defined guidelines for the treatment of rectal varices. The management of rectal varices is on a case-by-case basis and usually involves a multidisciplinary approach including a gastroenterologist, surgeons and an interventional radiologist[5]. Medical management includes non-selective beta blockers to reduce the portal hypertension and decrease the risk of bleeding. Endoscopic options include sclerotherapy and band ligation. Endoscopic sclerotherapy is superior to endoscopic band ligation, which has a high recurrence rate of 55.6% compared to 33.3% with sclerotherapy[6], but sclerotherapy has a risk of pulmonary embolism if it enters the systemic circulation. Surgical management with suture ligation or portocaval shunt surgery can be done but as most of the patients are in poor health, they are considered to be unsuitable candidates[7].
Finally, interventional radiology has the options of embolisation, TIPS or balloon-occluded retrograde transvenous obliteration (BRTO)[5,8]. TIPS is considered a good choice in patients who are not candidates for surgery as it is a minimally invasive procedure. TIPS has contraindications of congestive heart failure, severe pulmonary hypertension and severe tricuspid regurgitation, among others. TIPS in patients with congestive heart failure increases the venous return, which in turn causes cardiac overload. BRTO is another endovascular procedure, which has many advantages over TIPS being less invasive and with a low rebleeding risk, performed in poor hepatic reserve patients as well as those with encephalopathy[9]. BRTO is most commonly performed in gastric varices and its use in rectal varices still needs further study[7].
Embolisation is performed alone or with one of the procedures mentioned above, especially TIPS. It is done using various materials such as Gelfoam, coils, collagen, ethanol, autologous blood clot and thrombin. There is no recommendation regarding the superiority of one material over another[10]. Embolisation interrupts the communication between the portal vein and the superior rectal vein; this results in an increase in portal hypertension, resulting in worsening ascites and high recurrence rates[11]. In the presence of contraindication to TIPS or failed TIPS, embolisation is chosen for rectal varices. Our patient had heart failure with reduced ejection fraction, which is a contraindication for TIPS. Hence, he underwent transhepatic embolisation with both Gelfoam slurry and coiling of the left and right superior rectal vein along with the common trunk, resulting in complete obliteration and no reflux post intervention. At the 6-month follow-up he did not have recurrent bleed or worsening ascites which gives us a ray of hope. Standardisation of the technique along with guidelines for treatment of rectal variceal bleeds, especially when TIPS or other surgical options are contraindications, needs to be established with further extensive studies.