ABSTRACT
We report on a 70-year-old male patient admitted to the internal medicine department for evaluation of a right cervical mass. He had been treated with antibiotics as an outpatient by his primary care doctor. Upon admission the patient was asymptomatic, but within a few hours his cervical mass enlarged; this enlargement was confined to the right sternocleidomastoid muscle. Complete blood investigations including serology and autoimmunity were negative. The neck scan and MRI were in favour of myositis. No other lesions were found either in the nasal fibre-optic exam or in the thoracic-abdominal-pelvic scan. The biopsy of the muscle showed a lymphoplasmacytic inflammatory infiltrate of the perimysium. The diagnosis of focal myositis was made. The patient clinically improved during hospitalisation with complete resolution of symptoms without any specific intervention.
LEARNING POINTS
- A thorough clinical examination is essential in the evaluation and characterisation of cervical masses.
- The diagnostic approach must be rigorous in order not to ignore potentially serious diseases.
- A high level of clinical suspicion is needed in the diagnosis of focal myositis.
KEYWORDS
Neck masses, sternocleidomastoid muscle, magnetic resonance image (MRI)
INTRODUCTION
Cervical masses are extremely common. The most frequent aetiologies include oropharyngeal infections (viral or bacterial), systemic infections (such as HIV, EBV, bartonellosis, toxoplasmosis or tuberculosis), congenital disorders, tumours and thyroid diseases[1]. However, other uncommon entities such as focal myositis can present as cervical tumefaction and lead to misdiagnosis. At present, this inflammatory muscle disease remains a special entity due to its clinical-histological presentation and prognosis. It has not been included in the international classifications of idiopathic inflammatory myopathies; it therefore appears to be a rare entity that is still poorly understood[2].
CASE DESCRIPTION
A 70-year-old male patient was admitted to the internal medicine department for evaluation of a right cervical tumefaction. His past medical history was relevant for a non-invasive left lobe thyroid neoplasm treated by partial left lobe thyroidectomy in 2021, benign prostate hyperplasia, type 2 diabetes and sleep apnoea syndrome. He was on treatment with metformin 500 mg twice daily and tamsulosin 0.4 mg daily.
Upon admission, the patient reported a previously painful and soft right cervical mass spontaneously appearing and growing over the previous 2–3 weeks. He consulted his primary care doctor who suspected an oropharyngeal infection, and he started treatment with amoxicillin 1 gram three times per day for 7 days. The mass regressed during antibiotic treatment. The patient reported no history of dysphagia, night sweats, fever, chills, weight loss, asthenia or skin lesions. No oral, ocular or genital lesions, no arthritis or arthralgia, no Raynaud syndrome, no alopecia, no muscle weakness or another mass were reported. There was no history of recent travels, and his family history was non-contributory. The patient denied alcohol or illicit drug consumption. The patient has not been in contact with livestock, taken no walks in the forest, has no knowledge of an insect bite, and has not been swimming outdoors.
On physical examination, blood pressure was 120/70 mmHg, heart rate was 80 beats/minute, the patient was afebrile and oxygen saturation was 98% on room air. He was alert and oriented. The neck examination was normal. Mucous membranes were moist and well-coloured. No skin lesions were found. Heart sounds were regular without murmurs or rubs, pulses were normal and there was no oedema. Lungs were clear. The abdomen was tender but not distended, and without palpable masses.
Twenty-four hours after hospital admission the patient developed a spontaneous swelling, which was localised to the right sternocleidomastoid muscle. On examination the muscle was soft but slight painful on palpation, without any local inflammatory signs or local adenopathy.
The blood tests revealed discreet inflammatory syndrome (CRP 27 mg/l) with normal white cell count. Renal and liver function tests were within normal range. Electrolytes including total and corrected calcium were normal. Creatine phosphokinase (CPK) was normal. Serum electrophoresis was normal and angiotensin-converting enzyme was within the normal range. Serologies for HBV, HCV, HIV 1/HIV 2, bartonella, Lyme and syphilis were negative. CMV, EBV and toxoplasma titres were compatible with an old infection. QuantiFERON was negative. Calcitonin and thyroglobulin were within the normal range. Antinuclear, anti-dsDNA antibodies, p-ANCA and c-ANCA were negative. C3, C4 and total complement were within the normal range. The myositis panel (anti-Mi-2, anti-TIF1-gamma, anti-SAE1, anti-SAE2, anti-NXP-2, anti-MDA-5, anti-Jo-1, anti-PL-7, anti-PL-12, anti-EJ, anti-OJ, anti-KS, anti-Zo, anti-Ha and anti-HMGCR) came back negative. Blood cultures were negative.
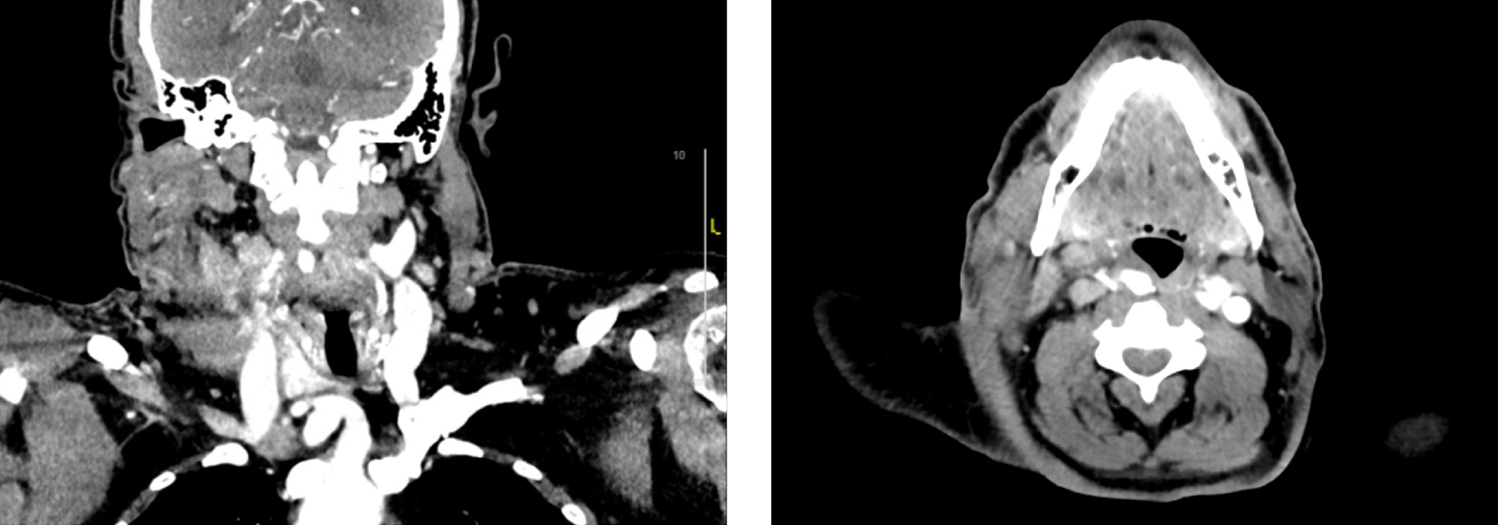
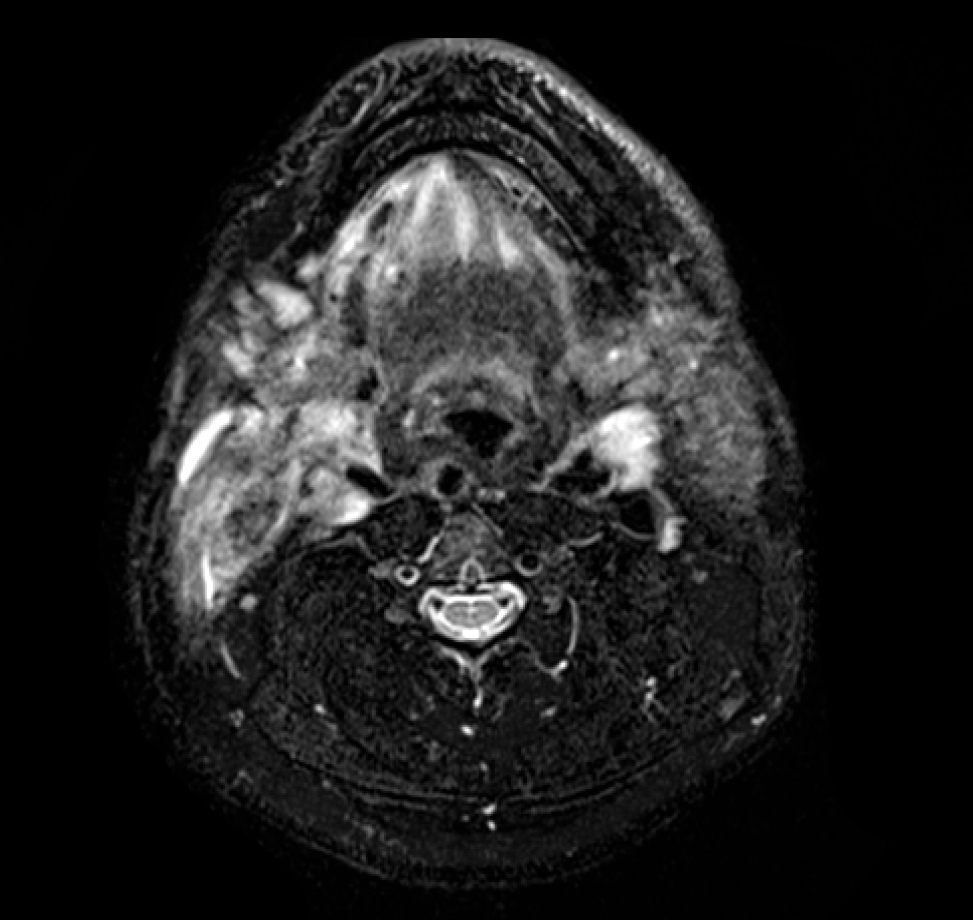
The neck scan described a thickening of the right sternocleidomastoid muscle and slight perilesional infiltration. The muscle enhancement remained homogeneous without focal fluid collection, and right jugular-carotid adenopathy in sectors III and IV, presumed to be reactive, was noted (Fig. 1). Imaging studies were completed by a thoracic-abdominal-pelvic scan, which was normal, and neck MRI showed an enhancement of almost the entire sternocleidomastoid muscle (Fig. 2). Nasal fibre-optic assessment by otorhinolaryngology was normal. In light of these clinical and radiological results the diagnosis of focal myositis was made, and biopsy of the right sternocleidomastoid muscle was performed. The biopsy showed a lymphoplasmacytic inflammatory infiltrate of the perimysium; special PAS, GMS and Ziehl stains did not reveal any specific infectious agents.
The diagnosis of focal myositis was made. The patient clinically improved during hospitalisation with complete resolution of symptoms without any specific intervention. The patient will be followed up in the outpatient clinic.
DISCUSSION
Neck masses, defined as abnormal lesions (congenital or acquired) that are visible, palpable or evident through diagnostic imaging studies, are very common reasons for consultation in adult patients[1,3]. Age is one of the most important clinical factors during evaluation of neck masses[4]. Asymptomatic neck mass in adult individuals has been reported as the first manifestation of a malignant disease[1,3]. The medical literature has frequently reported malignant lesions as the most common cause of neck masses in patients over 40 years of age, but the prevalence varies (between 16% and 80%)[5,6].
In the case presented, the clinical examination was important in the evaluation since it allowed us to specify that the swelling was contained within the sternocleidomastoid muscle and the ENT examination did not reveal any suspicious lesions. After all the investigations were performed, we made the diagnosis of focal myositis. This is an inflammatory and benign disease of unknown origin. It could affect one single muscle (as in our patient) or a muscle group and can present in patients of all ages. Clinically, patients report a subcutaneous mass progressively increasing in size (for weeks or months) and mostly affecting lower limbs – contrary to the case presented – and it is painful in approximately half of the reported cases[2,7].
In contrast to other rheumatic or idiopathic myopathies, extramuscular manifestations are not common as in our case, and patients remain in a good general condition. There is no diagnostic biological tool as the creatine kinase level and autoantibodies are normal, and inflammatory markers can be slightly elevated[2,7,8]. Differential diagnosis is wide and includes among others venous thromboembolic disease, soft tissue infection, malignant soft tissue tumours (liposarcoma, undifferentiated sarcoma, leiomyosarcoma, myxofibrosarcoma, angiosarcoma and fibrosarcoma), benign tumours, trauma, calf myositis, myositis ossificans and diabetic myonecrosis[2]. There has been controversy over whether idiopathic focal myositis was a part of systemic polymyositis. In this sense, Sekiguchi et al. described a series of four patients with focal myositis accompanied by the same HLA typing (HLA typing common to all patients were A2, B62, Cw3 and DQ3). They highlighted that at least some focal myositis may be considered to be a new medical condition with a common genetic background but not a part of systemic polymyositis[9]. The diagnostic approach must be rigorous because potentially serious diseases that can be life-threatening must not be ignored. Differentiation is based in particular on the topography of the lesion, its mode of presentation and its morphological characteristics on MRI, as well as the existence of associated signs.
MRI shows an inflammation restricted to a muscle, and muscle biopsy shows inflammatory infiltrates composed of macrophages and lymphocytes without any specific distribution within the muscle, permitting the clinician to rule out malignancy or infection. Evolution is spontaneously favourable without any treatment, and relapse is unusual[2,7].
CONCLUSION
The evaluation and work-up of neck masses must be rigorous. The diagnosis of focal myositis requires a high level of clinical suspicion, and potential life-threatening conditions must be ruled out.