ABSTRACT
Tracheoesophageal prosthesis (TEP) is an artificial connection between the trachea and esophagus allowing air into the upper esophagus from the trachea thereby vibrating it. TEPs give patients who lose their vocal cords to laryngectomies a tracheoesophageal voice. A potential complication of this is silent aspiration of gastric content. We present a case of a 69-year-old female with a TEP placed after a laryngectomy for laryngeal cancer who presented to the hospital with shortness of breath and hypoxia. She was initially treated for a presumed diagnosis of chronic obstructive pulmonary disease (COPD) and congestive heart failure (CHF) exacerbations but continued to be hypoxic despite aggressive medical management. Further evaluation revealed silent aspirations as a consequence of TEP malfunction. Through our case report we urge clinicians to consider this differential diagnosis, as the clinical presentation of silent aspiration among patients with a TEP can be easily mistaken for a COPD exacerbation. A large number of patients with TEPs are smokers with underlying COPD.
LEARNING POINTS
- TEPs give patients who lose their vocal cords to laryngectomies a tracheoesophageal voice.
- A potential complication of TEPs is silent aspiration around or through the TEP, causing coughing and even recurrent aspiration pneumonitis or pneumonia.
- Patients with TEPs typically have extensive smoking histories and underlying COPD or CHF which can have exacerbations that are similar in presentation.
KEYWORDS
TEP prosthesis, Aspiration, Pneumonia, Hypoxia
CASE DESCRIPTION
Our patient is a 69-year-old female with a past medical history of chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), and laryngeal cancer status post laryngectomy, tracheostomy and placement of a tracheoesophageal prosthesis (TEP) ten years prior, and has not had her TEP changed since the initial insertion.
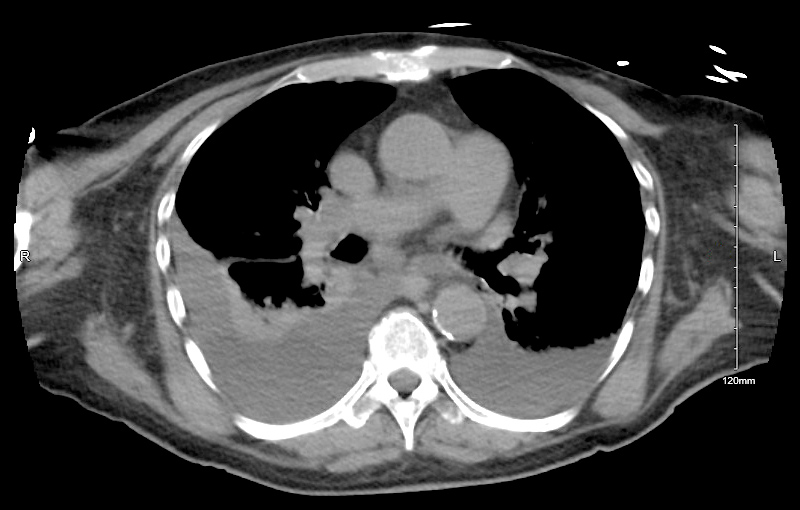
The patient presented with shortness of breath and cough for two days. She was noted to have a respiratory rate of 23 breaths per minute, a heart rate of 124 beats per minute, and an oxygen saturation of 80% while on supplemental oxygen with a fraction of inspired oxygen (FiO2) of 40% and 10 liters per minute (LPM). Over the next 6 hours, she required 100% FiO2 at 15 LPM. She was admitted to the Intensive Care Unit (ICU) due to her high oxygen requirements. A chest CT revealed a moderate right sided pleural effusion and a small left-sided pleural effusion. She was initially managed as a case of COPD exacerbation. She was treated with inhalers and intravenous steroids. She was also placed on broad-spectrum antibiotics as she had sputum cultures positive for pseudomonas. Her oxygen requirements normalized and she was discharged to a rehabilitation facility. She was readmitted with hypoxemia and increasing oxygen requirements nine days later. The patient was thought to have CHF exacerbation as she reported subjectively worsening edema and orthopnea. The CT scan also revealed stable pleural effusions from the prior scan, as depicted in figure 1. She underwent a thoracentesis as well, which yielded 500 ml of transudative fluid. However, in spite of adequate diuresis, her oxygen requirements remained high, and she was readmitted to the ICU. A repeat CT scan revealed stable effusions but multiple reticulonodular densities of the right upper and lower lobes. On further questioning, she stated that she had been noticing her tracheal secretions turning brown after she drank coffee for a few weeks prior to her presentation. This raised the suspicion of recurrent aspiration pneumonitis. This was confirmed when direct visualization of the TEP revealed leakage around the apparatus. With coordination from the speech pathology department, the patient was trained to self-cannulate her TEP with a small red rubber tube prior to meals. This is a known process to help reduce aspiration. She is currently stable after having her TEP replaced.
DISCUSSION
Tracheoesophageal speech is the most common voicing method used by patients with laryngectomies[1]. This is done by voice prosthesis implantation with the creation of a tracheoesophageal fistula. The TEP is a one-way valve inserted through a tract connecting the trachea and esophagus. When the patient occludes the stoma, the exhaled air is shunted through the TEP into the esophagus, where it induces vibration of the upper esophageal sphincter thereby producing clear and intelligible speech[1]. While TEPs provide patients with a voice post-laryngectomy, they also come with their set of challenges and complications. TEP leaks may occur either around or within the prosthesis. Rarely, a patient’s entire TEP may even dislodge and lead to the patient aspirating the TEP, requiring emergent removal[2]. Leakage through the voice prosthesis occurs when the valve can no longer close tightly due to, for instance, colonization of the valve by fungal-bacterial biofilm[3], the flap’s valve getting stuck in the open position, or a piece of food or object getting stuck in the valve. Leakage around the voice prosthesis is less common and is mainly due to TEP tract dilation or the inability to grip the prosthesis. This can occur when the puncture that houses the prosthesis widens due to loss of tissue elasticity. Risk factors for this include gastroesophageal reflux, poor nutrition, alcoholism, improper puncture placement, incorrectly-fitted prosthesis, TEP tract trauma, local granulation tissue, recurrent or persistent local or distant cancer, past radiation treatment, and radiation necrosis[1]. Aspiration around the TEP can present as persistent coughing and increased secretions from the stoma, and even hypoxia, as in the case of this patient. Our patient had been admitted twice for worsening hypoxia and was treated for CHF and COPD exacerbation. The persistence of her symptoms in spite of being adequately treated for both CHF and COPD raised the suspicion of another etiology contributing to her symptoms. This patient was having silent aspiration pneumonitis from her TEP which took an extended period of time to diagnose. Although rare now, several patients who have had TEPs may present with worsening oxygen requirements. Through our case report we urge clinicians to consider this differential diagnosis as the clinical presentation of silent aspiration among patients with a TEP can be easily mistaken for a COPD exacerbation. A large number of patients with TEPs are smokers with underlying COPD.