ABSTRACT
Adult-onset Still’s disease (AOSD) is a rare autoinflammatory disorder that can lead to a cytokine storm, causing a range of symptoms. Acute intestinal pseudo-obstruction is another rare condition that results in intestinal obstruction without anatomical cause.
Although the two conditions are rarely reported together, we present the case of a 62-year-old male who developed acute intestinal pseudo-obstruction in the context of an AOSD flare. This led to severe hypokalaemia and a critical condition. Other symptoms included a high-spiking fever lasting for weeks, polyarthralgias and a typical salmon-coloured rash. After ruling out other potential causes, the patient was diagnosed with AOSD. Our findings suggest that the cytokine storm associated with this disease triggered the acute intestinal pseudo-obstruction and life-threatening hypokalaemia, establishing a causal relationship.
Only four other cases of AOSD complicated by intestinal pseudo-obstruction have been reported, and this is the first to present with life-threatening hypokalaemia.
This case serves as a crucial reminder that, despite being a diagnosis of exclusion, Still’s disease should be considered as a potential cause of intestinal pseudo-obstruction, as prompt recognition and treatment of the underlying cause is crucial in managing this potentially life-threatening condition.
LEARNING POINTS
- Acute intestinal pseudo-obstruction is one of the systemic complications that can occur in autoinflammatory diseases such as AOSD, although it has rarely been described.
- If AOSD presents with abdominal presentation, such as acute intestinal pseudo-obstruction, then amyloidosis should always be carefully considered.
KEYWORDS
Adult-onset Still’s disease, intestinal pseudo-obstruction, hypokalaemia
INTRODUCTION
Adult-onset Still’s disease (AOSD) is a rare autoinflammatory disease, with an incidence of 0.16 to 0.4 per 100,000 persons per year. It is characterised by a broad spectrum of symptoms including fever, polyarthritis, arthralgia, transient erythema and pharyngitis, as well as variable biological markers[1]. While acute intestinal pseudo-obstruction has numerous aetiologies[2], AOSD is not typically considered as a cause, despite sharing common mechanisms with some inflammatory diseases. This report aims to highlight the association between intestinal pseudo-obstruction, hypokalaemia and the challenging, exclusionary diagnosis of AOSD.
CASE DESCRIPTION
Five days prior to admission, a 62-year-old male presented with acute signs and symptoms suggestive of mechanical intestinal obstruction, including severe abdominal distension, watery diarrhoea (10–15 stools/day) with a daily volume up to 3 litres of stool, nausea and vomiting. On clinical examination, his abdomen was swollen, and hyperactive bowel sounds were noted. However, he was not tender to the touch. He had no medical history besides obesity.
Prior to the onset of abdominal symptoms, the patient reported experiencing a high-spiking fever (> 39°C) for three weeks. Due to the life-threatening condition of the patient, he was transferred to the intensive care unit (ICU).
Diagnostic assessment
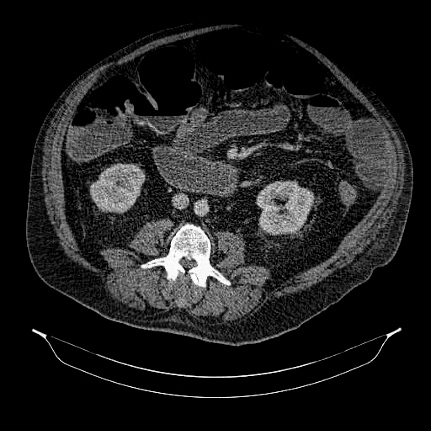
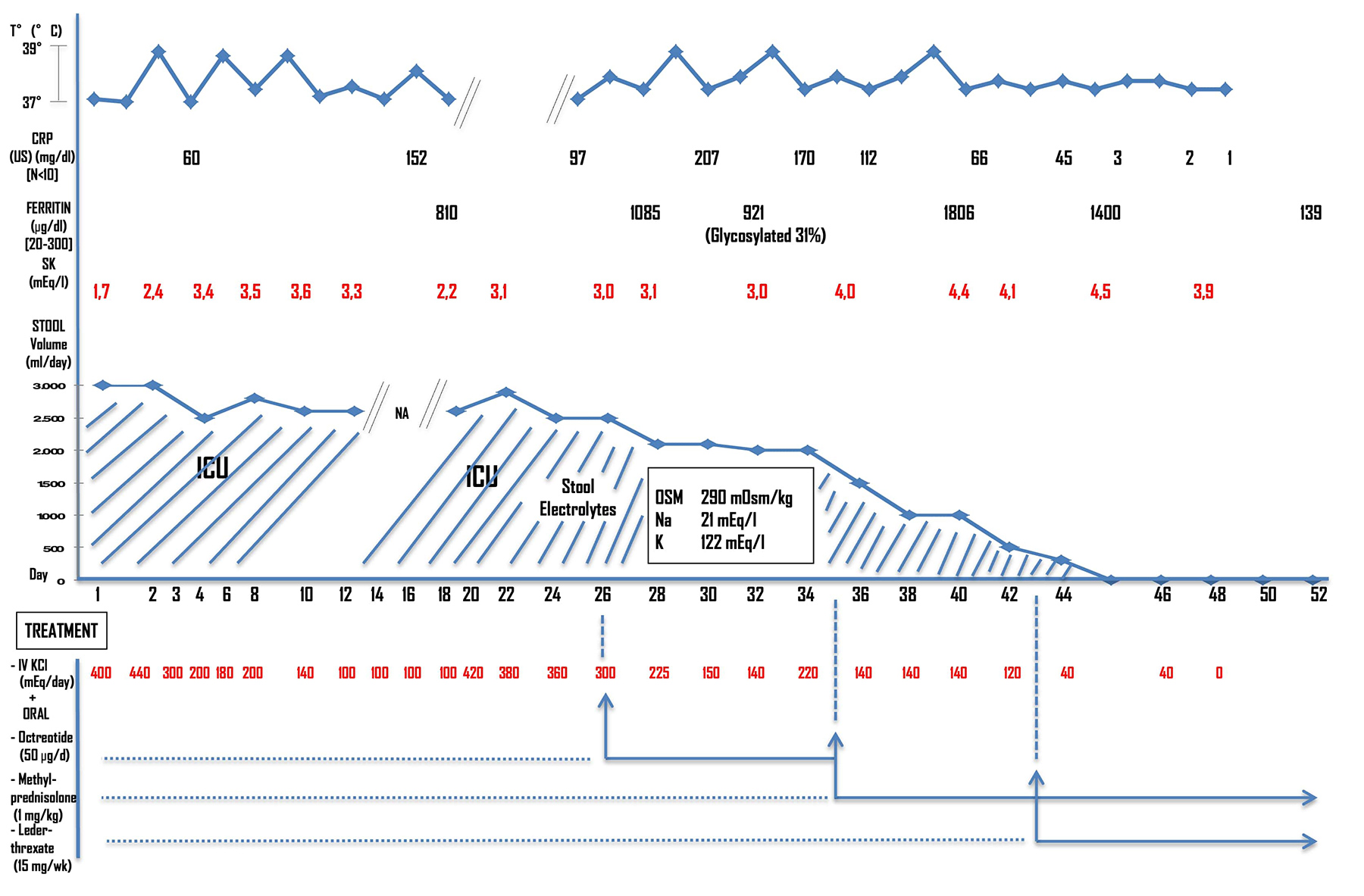
Laboratory tests conducted in the emergency department revealed high levels of inflammation markers: a white blood cell count of 14,000/µl (of which 88% was neutrophils) and a C-reactive protein level of 207 mcg/l. Ionogram values indicated severe hypokalaemia: 1.7 mEq/l [3.5–4.5], with low kaliuresis. An abdominal CT scan showed a distension of the small bowel and colon without any mechanical cause of obstruction, along with the presence of enteric adenopathies (Fig. 1). Based on the acute onset of symptoms and clinical presentation, a diagnosis of acute intestinal pseudo-obstruction was made. Peritonitis and pancreatitis were initially considered as possible causes but were ruled out based on the absence of corresponding signs, normal lipase levels and negative imaging indicating no inflammation in the pancreas or peritoneum. After the diagnosis of acute intestinal pseudo-obstruction, further investigation into the patient’s medical history was conducted. The patient reported symmetric polyarthralgia for one month (shoulders, wrists, phalanges, knees). Additionally, the patient had a vesperal fever, and a clinician spotted a non-pruritic, salmon-coloured rash on the patient’s torso during a fever spike. Additional laboratory tests revealed a negative antinuclear antibody and rheumatoid factor, a high ferritin level at 1,806 μg/l [20–250], and a low glycosylated ferritin level (31%).
Figure 1. Abdominal CT scan revealing small bowel and colonic distension, without evidence of mechanical obstruction
Low fractional sodium excretion ruled out renal potassium wasting, and stool electrolyte and osmolality measurements indicated secretory diarrhoea. Other examinations such as PET-CT and coloscopy were inconclusive, ruling out malignancy, systemic diseases, paraneoplastic syndromes, infectious aetiologies (including Tropheryma whipplei) and endocrinologic diseases. Amyloidosis was carefully excluded, notably by tissue biopsies of the abdominal fat and digestive tract.
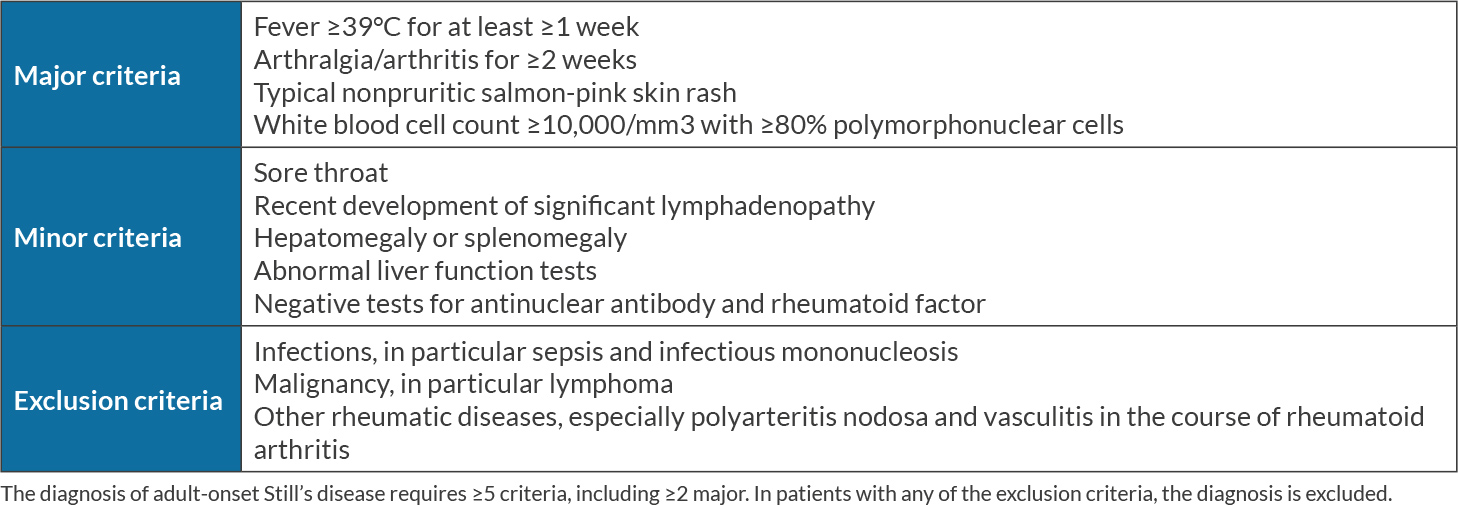
After ruling out other potential causes, the patient was diagnosed with AOSD, using the Yamaguchi criteria[3] (Table 1). The patient’s AOSD phenotype appeared to be a crossover between the two subtypes recently described in the literature (systemic and arthritic forms), and joint damage was confirmed by Tc-99m articular scintigraphy.
Based on these findings, we suggest a causal relationship between the hypercytokinemia that occurred during the AOSD flare and the acute intestinal pseudo-obstruction.
Additionally, we determined that the hypokalaemia was solely a result of the acute pseudo-obstruction. Initial treatment consisted of prokinetic drugs, a nasogastric tube and high-dose intravenous potassium (up to 440 mEq/day). Octreotide showed little effect. Upon diagnosing AOSD, corticosteroids (methylprednisolone 1 mg/kg/d) were administered, resulting in a rapid reduction in stool volume, abdominal symptoms and hypokalaemia. Fever spikes subsided (Fig. 2). Methotrexate was subsequently added for arthritis symptoms. Notably, the lack of improvement with standard treatment for paralytic ileus, but dramatic improvement following the introduction of steroids and methotrexate, strongly supported our hypothesis that the inflammation associated with AOSD was a triggering factor for the patient’s intestinal pseudo-obstruction. The patient was discharged from the ICU and followed up at six-months and one year, during which no electrolyte disturbance or abdominal symptoms were observed, and AOSD was in remission. Corticosteroid doses were decreased during this period.
DISCUSSION
AOSD is a disorder that results from dysregulated inflammation, leading to a cytokine storm[1]. Among the many systemic symptoms that can occur in AOSD, abdominal pain is a common manifestation, with estimates of its frequency varying widely from 1% to 48%[4]. In this case report, we highlight acute intestinal pseudo-obstruction as a rare complication of AOSD. Only four other cases with pseudo-obstruction have been previously reported[5-8]. Additionally, a recent case report described duodenojejunal inflammation causing chronic vomiting[9], suggesting that further investigation into potential gastrointestinal involvement in AOSD may be warranted. Previous reports have implicated an affectation of the sympathetic tone of the bowel and an imbalance in the autonomic enteric nervous system, leading to colonic distension[8]. However, recent literature suggests that other mechanisms, such as a high level of IL-18 associated with AOSD, may also play a role. Given that Crohn’s disease is also associated with high IL-18 and abdominal presentation[10], it is possible that common mechanisms are involved, including mucosal inflammation and a disruption of the intestinal barrier, contributing to gastrointestinal complications in AOSD. Additionally, AOSD may cause the development of multiple enteric adenopathies[11], which can worsen bowel motility impairment.
Notably, severe hypokalaemia is a precipitating factor that can reinforce the pseudo-occlusion, leading to a vicious circle that amplifies the phenomenon[2].
CONCLUSION
In this case, the lack of improvement with standard treatment for paralytic ileus, but dramatic improvement following the introduction of steroids and methotrexate, supports the causality relationship between AOSD and pseudo-obstruction.
While further investigation is needed to confirm these assumptions, it is important to consider the possibility of AOSD in patients presenting with concomitant features of a pseudo-obstruction and an inflammatory disease. Early recognition and treatment of this aetiology can be life-saving and reversible.