ABSTRACT
We present an extremely rare case of a patient with intermediate-high risk pulmonary embolism treated with percutaneous mechanical thrombectomy, complicated with stroke as a form of paradoxical embolism through a previously unknown patent foramen ovale. We reviewed the literature for indications, efficacy, and safety of this procedure, as well as for experience on this technique in patients with patent foramen ovale.
LEARNING POINTS
- Some authors propose percutaneous mechanical thrombectomy as an aggressive treatment of intermediate-high risk pulmonary embolism.
- Pending clinical trials, percutaneous mechanical thrombectomy seems to reduce right ventricle overload in these patients, with rare adverse effects.
- To our knowledge, this is the first reported case of stroke as a complication of the procedure. These patients should be screened for patent foramen ovale before the procedure.
KEYWORDS
Intermediate-high risk pulmonary embolism, percutaneous mechanical thrombectomy, patent foramen ovale, paradoxical embolism, stroke
INTRODUCTION
Risk stratification of patients with acute pulmonary embolism (PE) is mandatory for determining the appropriate therapeutic approach[1]. Primary reperfusion treatments are theoretically limited to patients with high-risk PE[1,2]. Over the last decade, several studies have examined the use of these therapies in patients with intermediate-high risk PE[3,4]. Their use in patients with patent foramen ovale (PFO) is not often described[5,6]. We present an extremely rare case of a patient with intermediate-high risk PE treated with percutaneous mechanical thrombectomy, complicated with stroke as a form of paradoxical embolism through a previously unknown PFO.
CASE REPORT
A 37-year-old woman presented with a 3-day history of dyspnea and pleuritic pain in the right hemithorax. She was under treatment with combined oral contraceptives. She underwent a replacement of mammary prosthesis two months prior to admission and had made several transatlantic plane trips over the last month, the last one three days before consulting.
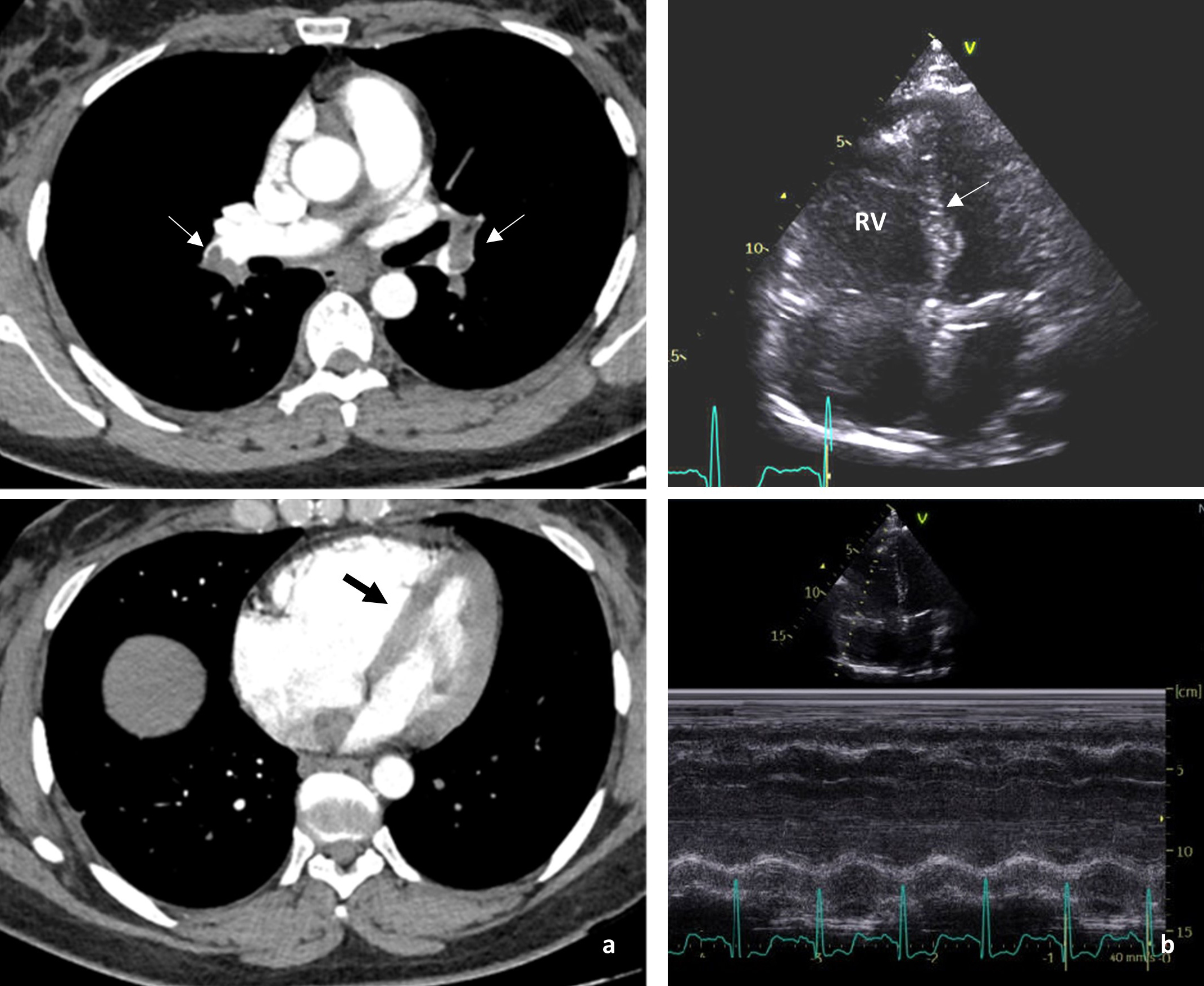
She was hemodynamically stable (BP 120/78 mmHg, HR 110 bpm), with tachypnea and mild hypoxemia (oxygen saturation 92%). Blood analysis revealed D-dimer levels of 2958 ng/ml and elevated Nt-proBNP and high-sensitivity troponin plasma levels. The EKG showed a S1Q3T3 pattern. An Angio-CT revealed bilateral filling defects affecting the left principal artery and right lobar branches and an elevated right ventricle/left ventricle (RV/LV) index (Fig. 1A). An echocardiogram confirmed severe RV dysfunction (Fig. 1B). She was considered intermediate-high risk PE, anticoagulant treatment was initiated, and she was admitted to the cardiac intensive care unit. A percutaneous mechanical thrombectomy (MT) using a FlowTriever® System was performed. During the procedure she presented a transitory ST elevation in EKG, and a previously unknown PFO was found when the catheter accessed the left atrium through the hole.
Figure 1. (a) CT angiography of pulmonary arteries. Filling defects in left principal artery and right superior lobar artery (thin arrows). Elevated RV/LV index and interventricular septum flattening (thick arrow) as signs of RV overload. (b) Transthoracic echocardiogram. Dilated RV with interventricular septum flattening (arrow) and tricuspid annular plane systolic excursion (TAPSE) of 10 mm as signs of RV dysfunction
Immediately afterwards she complained of stiffness in her left arm, and subsequently had left central facial paralysis and dysarthria. The patient was diagnosed with stroke (score NIHSS 6). An angio-CT showed a proximal occlusion of the M1 segment of the right middle cerebral artery. A cerebral mechanical thrombectomy was performed. Two days later, after hemorrhagic transformation was controlled, anticoagulation was restarted. A bubble test with transcranial doppler confirmed the presence of a massive right-left shunt consistent with PFO. Finally, the patient almost recovered from the stroke (score NIHSS 1). She was discharged 8 days after admission with rivaroxaban 20 mg daily, and PFO closure treatment was postponed.
DISCUSSION
The recommended treatment for patients with PE depends on the early (in-hospital or 30-day) mortality risk. In patients with high-risk PE, defined by hemodynamic instability, thrombolysis is indicated. If it is contraindicated or fails, other options are surgical embolectomy or MT[1].
Hemodynamically stable patients who present RV dysfunction and elevated cardiac enzymes are classified as intermediate-high risk PE. In these cases, intravenous anticoagulation with unfractionated heparin should be initiated with close monitoring for signs of instability[1]. However, there is much debate surrounding the treatment of these patients, and lately, more aggressive treatments have been proposed[7]. In the PEITHO trial, the use of systemic thrombolysis in these patients produced a faster recuperation of RV dysfunction, but with an increase in major adverse effects (11.5% had major bleeding; 2% had hemorrhagic stroke)[8]. Other studies corroborate an increased mortality in these patients when treated with systemic thrombolysis as opposed to conventional treatment[7]. Similar results were obtained with catheter directed thrombolysis (CDT)[9].
These results have led to the search of other therapeutic alternatives, such as MT. However, there is little return of experience on the use of MT in patients with PFO.
We conducted a narrative literature search in February 2023. PubMed database was searched using the terms “percutaneous mechanical thrombectomy”, “intermediate-high risk pulmonary embolism”, “patent foramen ovale”, “paradoxical embolism” in English. We found two prospective studies evaluating the efficacy and safety of mechanical thrombectomy in patients with intermediate-high risk pulmonary embolism, one prospective registry study evaluating the safety and effectiveness of percutaneous mechanical thrombectomy in pulmonary embolism, and one retrospective report of patients with patent foramen ovale and pulmonary embolism who underwent mechanical trombectomy. No single case report or case series were found of paradoxical embolism as a complication of the procedure in patients with PE and PFO. We thoroughly analyzed each of the articles, their appendices or supplementary material, and reference lists, to identify any other reported case of a similar complication, but did not find any.
Two prospective, multicentric, single-arm studies have evaluated the efficacy and safety of MT in patients with intermediate-high risk PE, including a total of 225 patients. Their primary endpoint was the reduction of RV/LV index 48 hours after the procedure. Both studies showed a significant reduction following MT, with lower major bleeding rates compared to systemic fibrinolysis (1.7% for the FlowTriever® System; 0.94% for the Indigo® Aspiration System). However, no clinical outcomes or long-term results were reported, and there was no comparative arm. A single case of cerebral infarction was described during 30-days follow-up after Indigo® Aspiration System use, with zero reported procedure-related stroke[3,4]. The FLASH registry, a prospective multi-center registry evaluating the safety and effectiveness of percutaneous MT for treatment of PE in a real-world patient population, provided preliminary evidence of excellent safety (1.2% presented major adverse events; 0.4% of all-cause mortality) with no stroke reported[10].
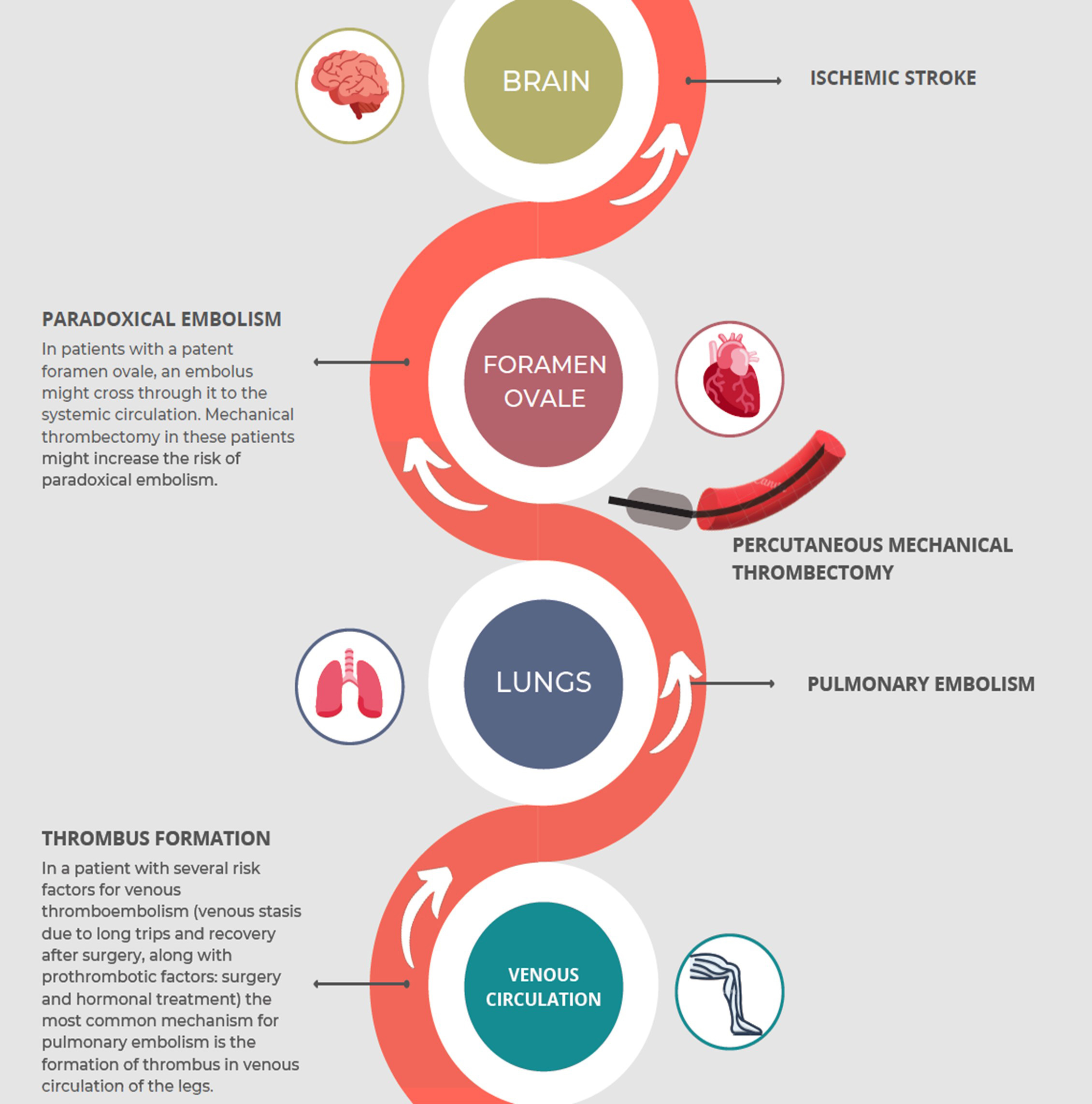
PFO is a prevalent condition that is usually asymptomatic. It can lead to paradoxical embolisms or passage of thrombus from venous circulation or right chambers to systemic circulation[11]. An observational retrospective study reported nine patients with PFO and PE who underwent MT using the Inari FlowTriever® System. The case of one patient who developed a stroke the day after the procedure was described, but it is unclear whether the stroke was related to it since the patient had altered mental status predating the procedure[5]. It has been hypothesized in previous studies that MT could favor paradoxical embolisms through a PFO due to thrombus manipulation and the passage of the catheter containing thrombotic material through right chambers (Fig. 2). Some authors propose to carry out a screening for PFO prior to MT. A positive result can indicate other therapeutic options, such as anticoagulation or surgical embolectomy with simultaneous PFO closure[5,6]. Moreover, screening for femoral deep venous thrombosis could be advisable before the femoral vein puncture for the procedure to avoid the risk of thrombus migration. However, there is no evidence yet to support the hypothesis that MT favors paradoxical embolisms in patients with PFO, nor to implement the mentioned changes in management for patients undergoing MT.
Figure 2. Thrombus path from its formation to the brain through the patent foramen ovale, causing a paradoxical embolism
CONCLUSION
We report an unusual case of periprocedural stroke due to paradoxical embolism through a PFO. In some patients with intermediate-high risk PE, mechanical thrombectomy might prevent early complications. Available evidence shows promising results of this preventive procedure, with a high success rate and low incidence of complications. Further studies are needed to evaluate the efficacy and safety of mechanical thrombectomy in this group of patients.