ABSTRACT
A previously healthy adolescent male was admitted with paraesthesia of his arms and legs. He admitted to daily recreational nitrous oxide use for the previous 3–4 months. He was found to have severe vitamin B12 deficiency, while magnetic resonance imaging of his spine showed T2 hyperintensity within the dorsal columns. This was suggestive of subacute combined degeneration of the spinal cord. He was treated with intramuscular injections of hydroxocobalamin and showed moderate improvement 1 month post-discharge.
LEARNING POINTS
- It is important to take a full history of illicit drug use, especially in young patients presenting with unusual symptoms.
- In cases of suspected nitrous oxide-induced neurological dysfunction with normal vitamin B12 levels, serum levels of methylmalonic acid and homocysteine can be measured to aid diagnosis.
- Prompt treatment of nitrous oxide-induced subacute combined degeneration of the spinal cord with B12 injections and discontinuation of nitrous oxide use allow for a gradual recovery, although in some cases patients may be left with residual symptoms.
KEYWORDS
Nitrous oxide, B12 deficiency, subacute combined degeneration of the spinal cord
CASE DESCRIPTION
A 19 years old male was referred to ambulatory emergency care by his general practitioner (GP) with a 1 week history of loss of sensation in his arms and legs that was worse in distal areas. He also had generalised numbness across his chest and abdomen, loss of balance while walking, and inability to complete fine motor skill tasks with his hands, such as getting dressed. He was normally fit and well and had no significant past medical history. There was no relevant family history of note. He was unemployed. He smoked five cigarettes per day and smoked cannabis occasionally, but did not drink alcohol. Upon further questioning, he admitted to using between 1–2 cylinders of nitrous oxide (N2O) every day for the previous 3–4 months. Each cylinder contained 640 g of N2O gas and could fill approximately 40 balloons.
Detailed neurological examination revealed distally impaired light touch, proprioception, and vibration sense in all four limbs. On the Medical Research Council (MRC) muscle power grading scale, a score of 4 out of 5 distally in both upper limbs and both lower limbs was recorded. Muscle power was otherwise normal proximally in all four limbs. All deep tendon reflexes were normal. Intention tremor and past-pointing were present in both upper limbs as well as 5/6 beats of ankle clonus bilaterally. He had a positive Romberg test and was unable to perform the heel-to-toe test. The patient was reviewed by the neurology team who advised he be admitted for further investigations.
Routine blood tests showed a normal haemoglobin with a mildly elevated mean cell volume. Inflammatory markers were normal. He was negative for COVID-19 and urine culture showed no growth. A computed topography (CT) scan of his brain was normal with no evidence of any space-occupying lesions. His vitamin B12 levels were found to be very low at <150 ng/L (reference range 180–650 ng/L). At this point, the clinical features, along with his history of heavy and prolonged N2O use and the laboratory findings of severe B12 deficiency, led to a suspicion of subacute combined degeneration (SCD) of the spinal cord.
Immunological tests were performed to rule out autoimmune disease, including antinuclear antibodies (ANA) and intrinsic factor (IF) antibodies, all of which were negative. Gastric parietal cell antibodies were weakly positive. Immunoglobulins were unremarkable, other than a mildly low IgM. No paraproteins were detected. All neuroimmunology tests were negative, including GM1, GM2, GD1a, GD1b, GQ1b, myelin oligodendrocyte glycoprotein, and aquaporin-4 antibodies. His HIV and syphilis screen were also negative.
The patient also had a lumbar puncture and a cerebrospinal fluid (CSF) sample sent for analysis, which showed normal glucose, protein, and Gram staining. CSF was also negative for oligoclonal bands, and no organisms were detected on CSF viral polymerase chain reaction (PCR) testing. Nerve conduction studies showed evidence of a very mild demyelinating sensorimotor peripheral neuropathy in the lower limbs only.
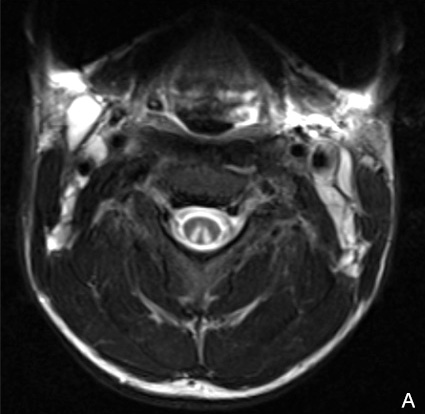
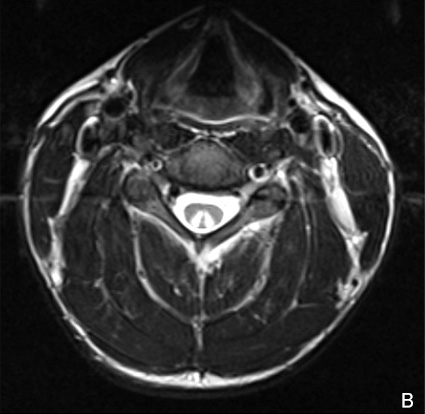
Magnetic resonance imaging (MRI) of the brain showed T2/FLAIR (fluid-attenuated inversion recovery) periventricular hyperintense lesions within the white matter on the right side of the brain. However, these lesions did not enhance post-contrast. MRI of the cervicothoracic spine showed a long segment of bilateral T2 hyperintensity within the dorsal columns between C2 and C6, with post-contrast enhancement noted at the C3/4 level (Fig. 1). Although degraded by motion artefact, there was also some T2 hyperintensity within the dorsal columns extending to at least the T7 level. However, there was no enhancement of these lesions post-contrast. Overall, these appearances were highly suggestive of SCD of the spinal cord.
The patient was started on intramuscular injections of 1 mg hydroxocobalamin on alternate days for six doses. He received physiotherapy input and made some improvement regarding his balance but still had difficulty in doing fine motor skill tasks with both hands. He was discharged 12 days after admission, with outpatient neurology follow-up and hydroxocobalamin injections every 3 months to be arranged with his GP.
The patient was followed up 1 month post-discharge. He reported that his walking had much improved, but he was still experiencing pins and needles in his hands and feet and needed help with daily activities such as getting dressed and eating. Neurological examination was largely the same as at initial presentation, except that the Romberg test was now negative and there were no beats of ankle clonus. The patient confirmed that he had stopped taking N2O since he was discharged.
Figure 1. Magnetic resonance imaging of the cervical spine at the level of C3 (A) and C3/C4 (B) showing hyperintensity within the dorsal columns bilaterally in both images, demonstrating the classical 'inverted V' sign
DISCUSSION
Vitamin B12 (cobalamin) is a water-soluble vitamin derived from animal produce such as meat, eggs, and dairy[1]. It serves as a cofactor in two important enzymatic processes which are responsible for metabolising methylmalonic acid and homocysteine[1]. It is the deficiency of cobalamin within these pathways that is thought to produce the neurological manifestations of B12 deficiency[1].
Although the exact mechanism is not entirely clear, B12 deficiency results in demyelination, specifically within the dorsal columns, lateral corticospinal tracts, and spinocerebellar tracts. This is otherwise known as SCD of the spinal cord and results in impaired distal proprioception, vibration sense and paraesthesia, spastic paraparesis, and ataxia. The demyelination can be seen on MRI of the spine as symmetrical T2 hyperintensity within the dorsal columns, with or without involvement of the lateral columns, commonly referred to as the 'inverted V' sign[1] (Fig. 1).
N2O use is becoming increasingly prevalent among teenagers and young adults, being popular in particular on the festival and clubbing scene[2]. Recreationally, infrequent and modest use of N2O is mostly unproblematic and results in the desired effect of euphoria and excitability, which is short-lasting and disappears within 2 minutes[2]. However, prolonged and heavy use can result in serious psychiatric, neurological, and haematological disturbances[2].
N2O causes gradual vitamin B12 deficiency as well as inactivating vitamin B12 via irreversible oxidation of its cobalt centre[3]. It is important to note that vitamin B12 levels are not always low in cases of N2O-induced SCD of the spinal cord, as evidenced in a 2016 systematic review by Garkani et al., which reported that B12 levels were only low in 46% of patients with N2O-induced neurological symptoms[2]. This implies that N2O can also cause a functional B12 deficiency rather than an absolute depletion[3,4]. If there is suspicion of N2O-induced neurological symptoms and vitamin B12 levels are normal, serum levels of methylmalonic acid and homocysteine can be measured instead, which accumulate if B12 is inactive or levels are low[1].
Clinical improvement typically occurs over weeks to months provided there is discontinuation of N2O exposure and prompt vitamin B12 supplementation. However only 14% of patients fully recover[1,4]. The British Society for Haematology guidelines for the treatment of cobalamin deficiency recommend 1 mg of intramuscular hydroxocobalamin to be administered on alternate days until there is no further improvement[5]. Maintenance treatment should continue with intramuscular 1 mg hydroxocobalamin every 2 months[5].