ABSTRACT
Background: Diplopia is the double vision of a single object, and can be binocular or monocular. Binocular diplopia is caused by the misalignment of the visual axes, with images falling on the fovea of the fixating eye and on the extra-foveal retina of the non-fixating eye, as a consequence of both neurological (i.e., oculomotor nerve palsies, ocular myopathies, neuromuscular junction disorders) and ophthalmic disorders (i.e., decompensation of a pre-existing strabismus). In contrast, monocular diplopia is generally explained by intraocular pathology (i.e., refractive errors, ocular media abnormalities, dry eyes), causing the image of a single object to fall, at the same time, on the fovea and on the extra-foveal retina of the same eye.
Methods: We report the case of a 22-year-old woman presenting with acute-onset monocular diplopia.
Results: The diagnosis of idiopathic intracranial hypertension (IIH) was based on the presence of papilloedema and elevated cerebrospinal fluid (CSF) pressure. Monocular diplopia resolved after CSF subtraction.
Conclusions: We describe a case of monocular diplopia as a presenting symptom of IIH, and discuss diagnostic issues of this possibly underestimated symptom in neurology clinical practice. Careful ophthalmic and neuro-ophthalmic examination can identify clinical features of diplopia, and drive diagnosis and treatment.
LEARNING POINTS
- Monocular diplopia is mostly an ophthalmological condition but can occur in a number of neurological diseases.
- Idiopathic intracranial hypertension can present with monocular diplopia.
- Differential diagnoses of diplopia in neurology and ophthalmology settings need to account for headache disorders.
KEYWORDS
Idiopathic intracranial hypertension, diplopia, monocular diplopia, papilloedema
INTRODUCTION
Diplopia is the double vision of single objects. Neurologists need to differentiate between monocular and binocular diplopia, depending on whether it occurs with one eye or two eyes opened [1]. Binocular diplopia is a feature of both neurological (i.e., oculomotor nerve palsies, ocular myopathies, neuromuscular junction disorders) and ophthalmic disorders (i.e., decompensation of a pre-existing strabismus), and is due to misalignment of the visual axes, with images falling on the fovea of the fixating eye and on the extra-foveal retina of the non-fixating eye. Monocular diplopia represents up to 25% cases of diplopia [2, 3] and is usually caused by intraocular pathology (i.e., refractive errors, ocular media abnormalities) that cause the image of a single object to fall, at the same time, on the fovea and on the extra-foveal retina of the same eye.
Here, we report a case of monocular diplopia occurring as a presenting symptom of idiopathic intracranial hypertension (IIH), and then discuss diagnostic issues of monocular diplopia in neurology clinical practice.
CASE DESCRIPTION
A 22-year-old woman presented with abrupt-onset diplopia, along with recurring 15-minute episodes of tension headache, in the absence of a previous history of headaches, concomitant treatments or drug abuse. She was obese, with reported weight gain over the past months (body mass index was 40.8 kg/m2), and was recently diagnosed with binge eating disorder.
On examination, the patient presented with reduced visual acuity (6/15, unchanged on pinhole occluder), and reduced colour sensitivity (12/17 on Ishihara plates) in the left eye. She reported diplopia when the left eye was kept open (i.e., monocular diplopia), also when using the pinhole occluder. Grade 1 disc oedema was found on the left eye after dilation. Right eye examination was within normal limits. Neurological and ophthalmological examinations were otherwise within normal limits (e.g., dry eyes, eye movements). The patient was also seen by the psychiatry clinic as part of binge eating disorder management, but no conversion origin for her symptoms was suggested.
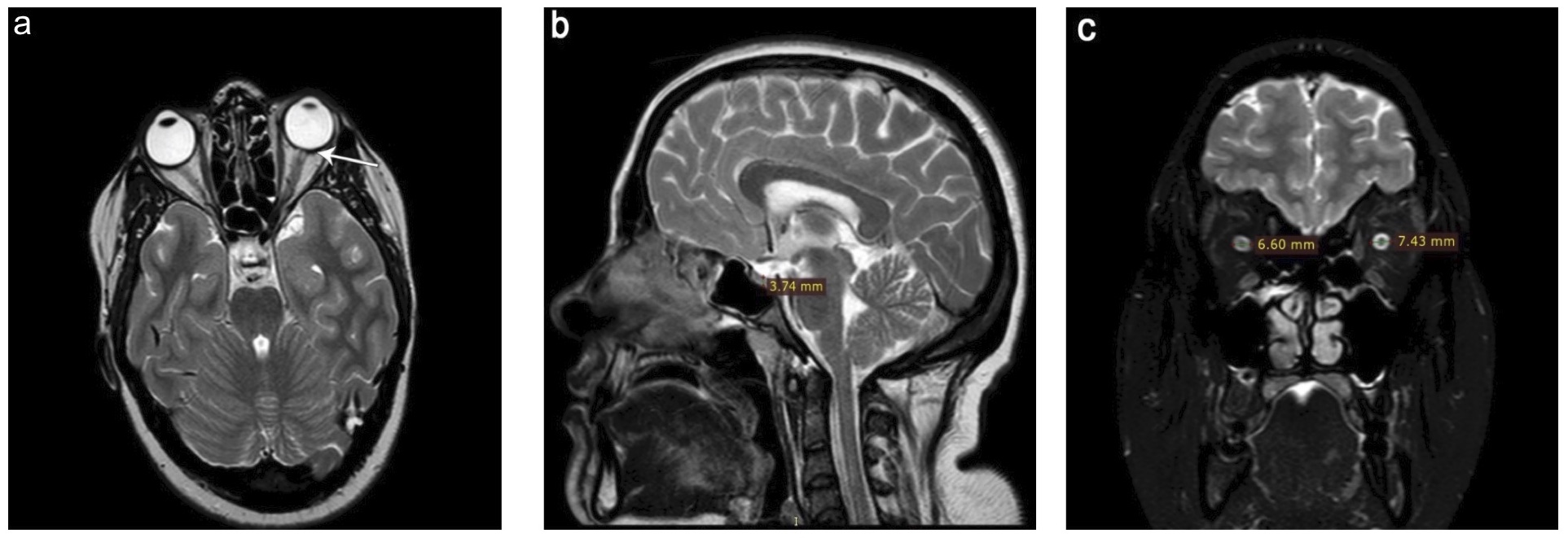
On ultrasound, the optic nerve looked enlarged, measuring 4.72 mm and 4.65 mm on the left and right eye, respectively. Brain MRI showed flattening of the left posterior globe, empty sella and optic nerve sheath enlargement (Fig. 1).
Figure 1. Brain MRI. On brain MRI, we found flattening of the left posterior globe (arrow) (a), empty sella (maximum pituitary gland height on the midsagittal T2w images was reduced to 3.74 mm, with a suggested cut-off of 4.80 mm) (b), and optic nerve sheath enlargement (maximum diameters of the optic nerve sheath on coronal T2w images were increased to 7.43 mm on the left and 6.60 mm on the right, with a suggested cut-off of 5.60 mm) (c). Neither dural venous sinus stenosis or parenchymal abnormalities were found
On lumbar puncture (lateral decubitus), opening pressure was 610 mmH2O, and we subtracted 36 ml of cerebrospinal fluid (CSF), until CSF pressure was 80 mmH2O. CSF biochemical analysis and cell count were normal. After lumbar puncture, the patient reported resolution of monocular diplopia, colour desaturation and headache. She was commenced on acetazolamide (up to 250 mg three times daily) and on a weight-loss diet plan. Benefits were sustained at the most recent (6-month) follow-up.
DISCUSSION
TWe described a case of monocular diplopia which responded to CSF subtraction, in the absence of any other neurological, ophthalmological or psychiatric causes, suggesting this was directly due to IIH. In particular, we made the diagnosis of IIH based on current diagnostic criteria[4], and on morphometric changes on brain MRI [5]. This case was made more difficult by the presence of unilateral papilloedema, which only occurs in 10% patients with IIH [6], and is more frequently caused by anterior ischaemic optic neuropathy, and optic neuritis, which we excluded on ophthalmology examination and brain imaging [7].
The increase in CSF volume and pressure in IIH can result into both monocular and binocular diplopia. The latter is a well-established symptom of IIH, and occurs as a consequence of downward displacement of the brainstem, with stretching of the VI cranial nerve within the Dorello canal [1]. However, the mechanisms of monocular diplopia in IIH are unknown. We could hypothesize that transudation of the CSF, through nerve fibres, into the macula, might be responsible for changes in dioptric media and subsequent monocular diplopia [1, 8].
We observed this on fundus exam, optic nerve ultrasound and MRI, although we did not perform refractive error testing and OCT, which could have been helpful to better understand the actual aetiology of monocular diplopia in our case.
Monocular diplopia is less common than binocular, but might still account for 11.5% to 25.1% cases of diplopia and, thus, should be carefully evaluated in neurology clinical practice [2, 3]. Neurological causes of monocular diplopia include certain tumours (i.e., pituitary neoplasms), causing compression of macular nerve fibres, and midbrain stroke, resulting in changes in the patient’s eyelid position and in the tear film interaction with the corneal surface [9]. Monocular diplopia can be seen in disorders of the visual cortex, cerebellum or vestibular nuclei (e.g., stroke, epilepsy, occipital migraine), although frequently with superimposition of multiple images and with bilateral features (cerebral polyopia)[10, 11]. Antiepileptic drugs, such as carbamazepine, lacosamide, lamotrigine, zonisamide and phenytoin, may be associated with diplopia, sometimes being monocular [12]. In addition, monocular diplopia is often misdiagnosed as a functional condition [1].
This paper is based on a single case, and a literature review only revealed a few reports; however, increased awareness of monocular diplopia among neurologists might lead, in the future, to better knowledge of its epidemiology and physiopathology. Careful ophthalmic and neuro-ophthalmic examination can identify clinical features pointing to a diagnosis of diplopia, and preventing unnecessary diagnostic testing. In neurology clinical practice, comprehensive eye examination, looking for ocular causes of diplopia before any neuro-diagnostic testing (e.g., morphometric evaluation of brain MRI), should identify IIH, which can present with visual disturbances from the very beginning. Monocular diplopia should be considered an ophthalmic manifestation of raised intracranial pressure.