ABSTRACT
Introduction: The incidence of vertebral artery (VA) injury during cervical spine surgery is rare. Even though tamponade is effective in many cases, early consultation of an endovascular team is recommended if bleeding cannot be controlled. We report a case of emergent endovascular embolisation of left VA due to iatrogenic injury during anterior cervical disc removal and fusion.
Case: A 47-year-old woman was admitted to our emergency department with serious arterial bleeding from the neck only hours after undergoing anterior cervical disc removal and fusion surgery. She was intubated and mechanically ventilated, however hemorrhage could not be successfully controlled by packing with surgical hemostatic agents. Cranial computed tomography, computed tomography of the cervical spine and CT angiography confirmed the suspected diagnosis of injury to the VA. Emergent endovascular embolisation successfully stopped the bleeding. Occlusion of the vessel was achieved by vascular plugging. The patient was discharged from our hospital 14 days after the intervention, receiving a revision surgery of the cervical spine on the day of embolisation. At the date of discharge she presented without any focal neurological deficit.
Conclusion: Pre-operative radiographic imaging of the cervical spine should be used routinely to identify anatomic abnormalities of the vertebral arteries. Endovascular embolisation appears to be effective in treating acute iatrogenic dissection of the vertebral arteries.
LEARNING POINTS
- There have been huge advances in endovascular (therapeutic) interventions in the last few decades.
- In selected cases, treatment of iatrogenic vertebral artery dissection with a primary endovascular approach and not with (open) surgery can be an option.
- Before permanent occlusion of a vertebral artery by endovascular embolization, it is important to check that the contralateral vertebral artery can provide adequate collateral circulation.
KEYWORDS
Vertebral artery injury; embolisation.
BACKGROUND
The incidence of vertebral artery injury during cervical spine surgery is low, with reported incidences of 0.07% to 1.96%[1-5]. Nevertheless, in case of a vertebral artery injury, prompt recognition and management are important[2,6]. Bleeding can usually be controlled with topical haemostatic agents[1]. However, if bleeding is uncontrollable, a surgeon or an endovascular team should be consulted[4,5,7]. We report a case of emergent endovascular embolization of the left vertebral artery due to iatrogenic injury during anterior cervical disc removal and fusion.
CASE REPORT
A 47-year-old woman was admitted to our emergency department with serious arterial bleeding from the neck a few hours after undergoing anterior cervical disc removal and fusion surgery. She was intubated and mechanically ventilated, but haemorrhage could not be successfully controlled by packing with surgical haemostatic agents. The patient therefore underwent further medical imaging by cranial computed tomography (CT), CT of the cervical spine and CT angiography.
CT imaging showed an occlusion of the left vertebral artery as well as laterodorsal dislocation of the cage which had been placed between 5th and 6th vertebrae (Fig. 1). No early ischaemic changes in the brain were detected.
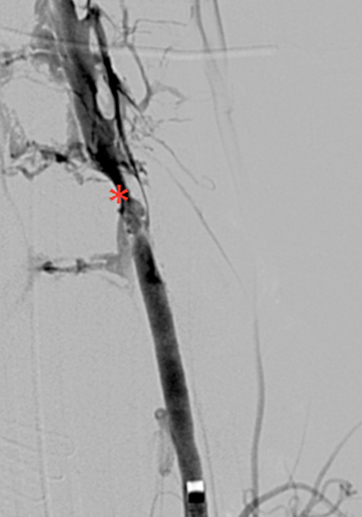
It was decided to take an endovascular approach. Selective angiography of the left vertebral artery showed stasis of contrast flow (occlusion of the artery) after 2–3 cm (Fig. 2). We first attempted to probe the distal entry of the damaged artery in order to implant a covered stent (Fig. 3).
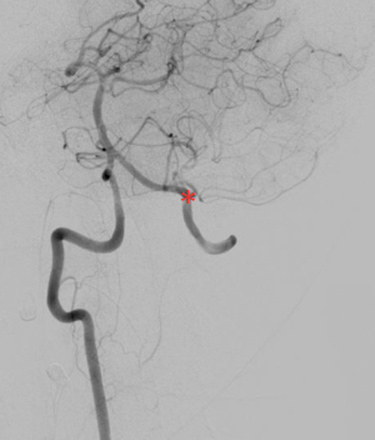
However, this was impossible due to serious damage as well as spasm of the distal fraction of the vertebral artery. We therefore decided to embolize the proximal fraction to stop the bleeding by using an AMPLATZER© vascular plug (Fig. 4). Before occlusion of the artery we demonstrated adequate collateral flow by using selective angiography of the right vertebral artery to show retrograde filling of the distal part of the left vertebral artery (Fig. 5).
The patient was discharged from our hospital 14 days after the intervention, and having received revision surgery of the cervical spine on the day of embolization. At discharge she had no focal neurological deficits.
Figure 1: CT scan: occlusion of the left vertebral artery (arrow) and cage dislocation (red asterisk).
Figure 2: Digital subtraction angiography: occlusion of the left vertebral artery (red asterisk).
Figure 3: Arteriovenous fistula due to massive damage to the left vertebral artery (red asterisk).
Figure 4: Implantation of a 5 mm AMPLATZER© vascular plug (red asterisk).
Figure 5: Retrograde filling of the distal part of the left vertebral artery (red asterisk).
DISCUSSION
Preoperative magnetic resonance imaging or CT angiographic imaging of the cervical spine should be used routinely to identify anatomical anomalies of the vertebral arteries and to avoid postoperative neurological sequelae[4-6].
Deep anatomical knowledge and close attention to surgical landmarks are obligatory when performing cervical spine surgery[2,7,8].
There have been huge advances in endovascular (therapeutic) interventions in the last few decades. Some pathologies which had been treated surgically until recently are now being increasingly addressed by interventionalists in angiology, cardiology and radiology. In our case, iatrogenic vertebral artery dissection was managed with primary intervention and not with (open) surgery.
Endovascular embolization appears to be effective in treating acute iatrogenic dissection of the vertebral arteries[9]. However, before permanent occlusion it is important to check that the contralateral vertebral artery can provide adequate collateral circulation[9].