ABSTRACT
Hypersensitivity pneumonitis is understood to be a delayed allergic reaction to the repeated exposure of a usually innocent inhaled agent, causing inflammatory damage to the pulmonary parenchyma, alveoli and terminal bronchioles. With ongoing exposure, it can cause respiratory compromise and pulmonary fibrosis. Recognizing the heterogeneity of the causative agents and the low incidence of the disease, we considered it important to report the case of a greenhouse worker who developed aCladosporium sp. related hot-tub lung hypersensitivity pneumonitis. We believe it to be the first reported case of a greenhouse occupational hypersensitivity pneumonitis due to Cladosporium sp.
LEARNING POINTS
- Enquiring about environmental and occupational exposure during anamnesis is fundamental, particularly when addressing respiratory tract symptoms.
- The mainstay management of hypersensitivity pneumonitis is based on eviction of the offending agent and control of inflammation, currently with corticosteroids.
- Antigen source removal may entail important psychological, social and economic consequences for the patient and will need a multidisciplinary approach.
KEYWORDS
Hot tub lung, hypersensitivity pneumonitis, Cladosporium herbarum, greenhouse
CASE DESCRIPTION
We present the case of a 39-year-old non-smoker female who was a floriculture greenhouse worker, with an unremarkable medical history. She was admitted to our emergency department with recent irritative cough, dyspnoea on moderate effort and pleuritic chest pain. A chest X-ray showed bilateral reticular interstitial opacities. The patient was treated with inhaled LABA/ICS and discharged home. Ten days later, with no clinical improvement, the patient was evaluated in a private clinic, where a course of macrolide antibiotics was started. During the next 9 days, the symptoms worsened and the patient returned to our emergency department. Physical examination showed no major abnormalities, except for inspiratory fine crackles in both lung bases. A repeat chest X-ray showed diffuse fine nodular opacities (Fig. 1). The patient was then admitted to our internal medicine department.
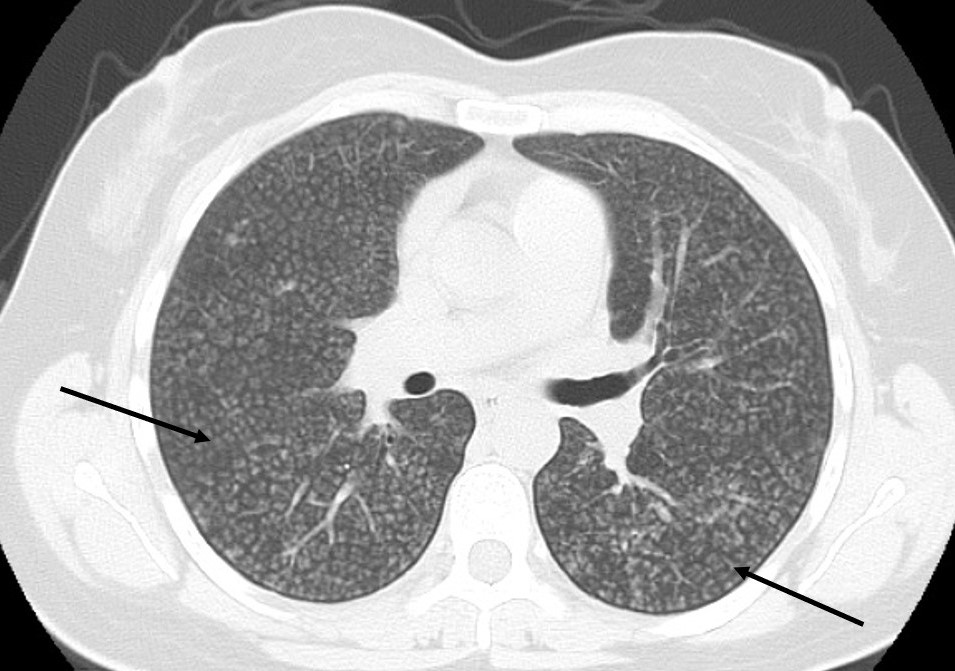
Blood work-up showed no relevant changes. Autoimmune disease screening was negative and sputum and blood cultures were sterile. A Mantoux test was anergic. A high-resolution computed tomography (HRCT) lung scan (Fig. 2) showed a diffuse micronodular pattern, suggesting atypical alveolar interstitial disease. Bronchoalveolar lavage analysis showed intense lymphocytic alveolitis; low CD4/CD8 ratio; polymerase chain reaction for Pneumocystis jirovecii, respiratory syncytial virus, adenovirus, influenza A and B virus, parainfluenza virus types 1, 2 and 3, cytomegalovirus and herpes simplex virus 1 and 2 were all negative; Mycobacterium smears and cultures were also negative.
Figure 1. Chest X-ray of patient at admission to emergency department, showing diffuse fine nodular opacities
Figure 2. HRCT lung scan showing a diffuse micronodular pattern, with numerous irregularly contoured micronodules
Give the high suspicion for hypersensitivity pneumonitis (HP) and inconclusive other tests, we carried out a precipitin assay that revealed positive precipitins against Cladosporium herbarum A lung biopsy showed a pattern of extrinsic allergic alveolitis, associated with well-defined granulomas suggesting hot-tub lung disease. Pulmonary function tests showed a mild restrictive defect and severe decrease in carbon monoxide diffusion capacity (57% of predicted).
Taking into account the epidemiologic background, all the findings in the evaluation and in the absence of pulmonary fibrosis, a diagnosis of subacute hot-tub lung HP was made. Corticosteroid therapy with prednisolone 1 mg/kg/day was started with significant clinical improvement. The patient was subsequently discharged to outpatient follow-up. Following total allergen eviction, the corticosteroids were slowly reduced until stopped completely.
At 2-year follow-up the patient was working at a textile factory, asymptomatic and had normalized pulmonary function tests.
DISCUSSION
HP is a pulmonary parenchymal syndrome characterized by an allergic/immune response triggered by the repeated exposure to an inhaled antigen in a patient with predisposing conditions and genetic factors. The association between environmental and occupational exposure and pulmonary disease has been reported for more than two centuries; however, diagnostic criteria are still lacking. The condition is usually divided into two categories: acute/subacute versus chronic HP, depending on the type of exposure and clinical presentation[1].
A poor prognosis is related to the presence of specific radiological patterns at diagnosis and current research has suggested a classification of acute/inflammatory HP versus chronic/fibrotic HP[1,2,3]. A good prognosis is associated with the prompt identification and removal of the offending allergen. Therefore, with a heightened clinical suspicion and characteristic pattern in CT lung scan or lung biopsy suggestive of HP, the antigen-specific plasma precipitins will determine the management of the disease, its recurrence and the requirement for professional or lifestyle changes[1].
The incidence of HP has been reported to range from ~0.9 to 2.71 cases per 100,000 person-years[4, 5] and over 200 causal agents have been identified[6], making this a rare and very heterogenic disease. Further research is needed to characterize possibly different clinical phenotypes depending on the antigen source and host factors.
Concerning the Cladosporium sp., it has been found in humidifiers, heating and ventilation systems, moldy tapestries and ceilings, and has been a reported causal agent of hot-tub lung HP, but also an agent of chronic HP, as it can easily develop in the household environment[6]. Our case appears to be the only one in the literature that describes C. herbarum HP developing in a greenhouse occupational environment.
In this case, as the patient’s symptoms did not recur after returning home, the suspected source for the inhaled spores was assumed to be the workplace and the patient made the decision to resign her job. In other cases, however, antigen sources can be more difficult to avoid and social care/support may play an important role in the eviction of the offending agent, especially when there is no clear association with occupational exposure[7].