ABSTRACT
Pancreatic pseudocysts are a frequent complication of chronic pancreatitis. Nonetheless, they seldom extend beyond the peripancreatic region. However, migration towards the mediastinum may cause heterogeneous and non-specific symptoms, such as dysphagia, chest pain and dyspnoea, which depend on the localization and extension of the cysts. We present the case of a patient with chronic pancreatitis who was admitted to our ward for low-grade fever and mild dyspnoea and who rapidly developed bilateral laterocervical swelling associated with acute dyspnoea and trismus. A total body CT scan showed multiple abdominal pancreatic pseudocysts, one of which had migrated to the mediastinum and towards the retropharyngeal space. Clinicians should always consider the possibility of extra-pancreatic pseudocysts in patients with known pancreatitis so that uncommon clinical presentations with a potentially fatal outcome will be recognized.
LEARNING POINTS
- Mediastinal pancreatic pseudocysts are a rare manifestation of acute and chronic pancreatitis.
- The clinical presentation of mediastinal pancreatic pseudocysts is variable, and they may rarely have a fatal outcome.
KEYWORDS
Chronic pancreatitis, mediastinal pancreatic pseudocysts, dyspnoea, trismus, mediastinitis
INTRODUCTION
A pancreatic pseudocyst is defined as an encapsulated fluid collection with a well-defined wall, occurring outside the pancreas and without necrosis. The most common cause in adults is acute pancreatitis and the most common location is the abdominal peripancreatic region[1]. However, pancreatic pseudocysts may rarely migrate to the mediastinal space.
CASE DESCRIPTION
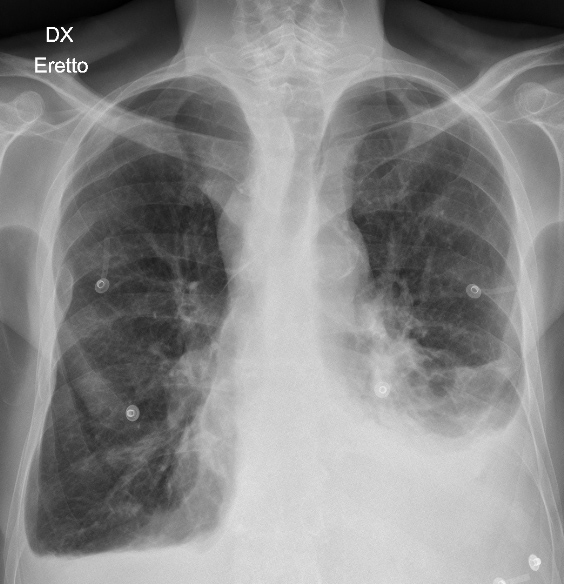
A 57-year-old Caucasian man was admitted to our emergency room with low-grade fever associated with increasing fatigue and mild dyspnoea. The patient reported that the symptoms had started a few days before admission. His medical history was remarkable for chronic alcoholic pancreatitis, with a recent exacerbation requiring hospitalisation and complicated by pneumonia and a perihepatic and subphrenic abscess, currently treated with ciprofloxacin. On admission, the patient was in a poor physical state, slightly tachycardic (heart rate 104 bpm) and subfebrile (temperature 37.7°C). Physical examination revealed the presence of jugular vein distension at 45° and reduced breath sounds at the left pulmonary base. The liver was palpable 4 cm from the arch, but without tenderness. Laboratory examinations showed a substantial increase in C-reactive protein (151 mg/l, normal <5 mg/l) with normal procalcitonin and an already known moderate elevation of amylase and lipase levels (amylase 534 U/l, normal <46 U/l and lipase 540 U/l, normal <60 U/l). A chest X-ray (Fig. 1) showed the presence of bilateral pleural effusions, with a left-sided predominance.
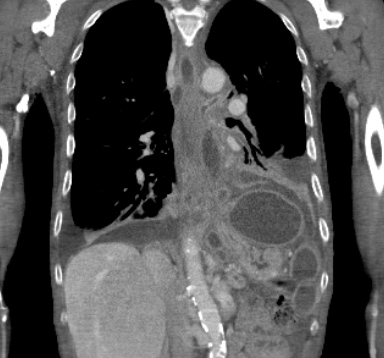
The patient was started on antibiotic treatment with ceftriaxone for suspected pulmonary infection, as the pleural effusion showed typical exudative characteristics. A few hours after admission, the patient rapidly developed bilateral neck swelling, with worsening dyspnoea and massive trismus. A total body CT scan was immediately performed and showed the presence of multiple abdominal pancreatic pseudocysts, one of which had possible fistulous continuity with the duct of Wirsung. Furthermore, this pseudocyst had migrated cranially through the diaphragmatic hiatus to the mediastinum (in both anterior and posterior spaces) where multiple cystic concamerations were seen, with an extension towards the retropharyngeal space. This pseudocyst migration was the cause of anterior dislocation of the trachea and oesophagus (Figs. 2–5).
Figure 2 -5. CT scan showing mediastinal migration of pancreatic pseudocysts
The patient was transferred to the intensive care unit for airway management. Percutaneous drainage of the abdominal portion of the migrated pseudocyst was performed, followed by a clamshell thoracotomy with pleuro-mediastinal decortication and right cervicotomy. Because of the worsening C-reactive protein levels (263 mg/l with an increase in procalcitonin levels to 2.63 µg/l, normal <0.25 µg/l), broad-spectrum antibiotic therapy with piperacillin/tazobactam was started to treat a possible infection of the mediastinal space.
The clinical course during the following weeks included relapse of a significant left pleural effusion, which was ascribed to a pancreatico-pleural fistula. A new thoracotomy with pleural cleansing and a laparotomy with caudal spleno-pancreatectomy were performed to close the fistula. The intervention was successful and the patient recovered fully and was discharged home after 4 weeks of hospitalisation.
DISCUSSION
Pancreatic pseudocysts occur in up to 40% in all cases of pancreatitis, but the prevalence of mediastinal localization has not been fully determined[2, 3]. Symptoms of abdominal pancreatic pseudocysts include local pain, nausea, vomiting, jaundice and possibly bleeding[4]. The symptoms of mediastinal pseudocysts can be very variable. In addition to the typical abdominal presentation, pleural effusion, dysphagia, posteriorly radiating chest pain, congestive heart failure, dyspnoea and airway obstruction have been described in the literature[5–7].
Treatment for pancreatic pseudocysts depends on the clinical presentation, pseudocyst size, localization and clinical expertise. Treatment for abdominal pseudocysts varies from a conservative approach (observation, naso-enteric nutrition or somatostatin receptor agonists) to drainage (endoscopic, percutaneous or possibly surgical). The approach is less defined for migrated pancreatic pseudocysts as they occur very rarely. Cases of spontaneous remission have been reported after initiation of total parenteral nutrition, and some patients have been successfully treated with octreotide therapy, but often percutaneous, endoscopic or surgical drainage is required[8–11]. Thoracotomy is usually needed for mediastinitis, but only a few cases of thoracoscopic drainage of mediastinitis secondary to pancreatic pseudocyst have been described[12].
In light of the rapidly evolving clinical picture, with high-risk airway obstruction and the simultaneous hypothesis of mediastinitis, a conservative approach was not considered for our patient. A combined approach of percutaneous drainage, thoracotomy and urgent cervicotomy was adopted. Furthermore, due to the early recurrence of left-sided pleural effusion, a new thoracotomy and an exploratory laparotomy with caudal spleno-pancreatectomy were undertaken.
Acute or chronic pancreatitis associated with abdominal symptoms may suggest a complicated pancreatic pseudocyst. However, this case report shows that pancreatic pseudocysts can migrate towards the mediastinum and present in a subtle, non-specific manner with atypical and unexpected symptoms. Clinicians should always consider the possibility of the presence of extra-abdominal pancreatic pseudocysts in patients with known pancreatitis, so that uncommon clinical presentations with a potentially fatal outcome will be recognized.
Treatment can differ greatly from case to case, depending on localization, extension and clinical presentation. In our case, because of high-risk airway obstruction and the hypothesis of mediastinitis, a more invasive approach was undertaken. Furthermore, given the early recurrence of pleural effusion, caudal spleno-pancreatectomy was indicated in order to permanently close the pancreatico-pleural fistula.