ABSTRACT
A masquerade syndrome is an ophthalmological entity where a neoplasm mimics an inflammatory condition. Ocular melanoma (chiefly uveal) may present with symptoms suggestive of intraocular inflammation such as endogenous endophthalmitis. Ocular melanoma is most commonly found in middle-aged and older caucasian patients. One-third of all uveal melanoma cases present asymptomatically. Early diagnosis facilitates treatment before ocular melanoma reaches metastatic stage IV. Current therapy options for stage IV patients are palliative care and clinical trial participation.
LEARNING POINTS
- Masquerade syndrome and intraocular haemorrhage can hide a neoplastic aetiology.
- A biopsy should be carried out for correct diagnosis if intraocular haemorrhage is present and a neoplastic pathology is suspected.
- A multidisciplinary approach should be adopted to enhance the quality of life of patients with metastatic ocular melanoma.
KEYWORDS
Ocular melanoma, intraocular haemorrhage, endogenous endophthalmitis, masquerade syndrome, metastasis
CASE REPORT
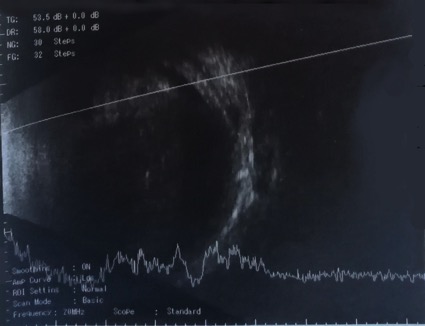
A 75-year-old woman presented with an 8-day history of pain, eye tearing and loss of vision in the right eye. There was no history of trauma or ocular surgery. On examination, there was periorbital oedema and erythema, exuberant chemosis, the cornea was transparent and a haemorrhage was seen in the anterior chamber. Right ocular echography revealed dense echoes with low mobility in the vitreous cavity (Fig. 1). The patient was admitted for aetiological study of endophthalmitis and began antibiotic therapy with ceftazidime and ophthalmic ciprofloxacin. There was progressive clinical improvement with topical and systemic antibiotics, ophthalmic dexamethasone, timolol, dorzolamide and methylprednisolone. The fasting blood sugar was 82 mg/dl, while retroviral and autoimmune screening was negative. Systemic infection was excluded and cultures yielded no growth. Due to the inconclusive aetiological study of the endogenous endophthalmitis, the patient was referred for consultations with Internal Medicine and Ophthalmology clinicians.
A few months later, the patient represented with asthenia, anorexia and night sweats. On examination, there was hepatomegaly with several palpable nodules. A computed tomography (CT) scan of the thorax, abdomen and pelvis revealed pulmonary metastasis and hepatomegaly with a metastatic lesion. A CT-guided liver biopsy was performed without complications. Histological examination revealed metastatic melanoma.
In view of the clinical evolution, the endogenous endophthalmitis and the metastatic melanoma, and after exclusion of other locations for this tumour, a presumptive diagnosis of stage IV ocular melanoma was made. The patient complained of irruptive pain, which was managed with fentanyl patches and oral fentanyl. Due to marked worsening of the patient’s general condition, it was not possible to administer palliative chemotherapy. The patient rejected a proposal to participate in a clinical trial.
DISCUSSION
Uveal melanomas are rare tumours that most frequently masquerade as inflammation[1]. The term masquerade syndrome first appeared in the ophthalmic literature in 1967 when it was used to describe conjunctival carcinoma presenting as chronic conjunctivitis[1]. Masquerade syndromes have since been defined as entities, including neoplastic processes, that mimic inflammatory conditions[1].
Haemorrhage in the anterior chamber may be the initial clinical sign of uveal melanoma[2,3]. As highlighted in this case, an intraocular haemorrhage and endogenous endophthalmitis suggest a neoplastic pathology (uveal melanoma). A non-invasive diagnosis can usually be made based on ultrasonographic and funduscopic findings[1,4]. In a case with a high suspicion of neoplastic pathology, a fine needle diagnostic biopsy must be performed to distinguish haemorrhage from ocular melanoma, metastatic tumour or other lesions[5]. This technique can also be employed for molecular prognostic testing and is useful for stratifying high-risk patients into clinical trials[4,5].
Without an early diagnosis and treatment, ocular melanoma may progress to metastatic stage IV. The most common initial sites of melanoma metastasis include the liver, lung, skin, soft tissue and bone[4]. At this stage, the principal role of the clinician is to improve the quality of life of patients by controlling their symptoms. Pain relief was administered in the described case. A multidisciplinary intervention with palliative and oncological input is necessary. Current therapy options are not curative and the patient should only participate in a clinical trial if it does not affect their quality of life[4].