ABSTRACT
Introduction: Chest wall masses are caused by various entities and have diverse aetiologies. A careful history and physical examination are crucial to establish the correct diagnosis.
Case report: A 77-year-old man presented with depressive mood, anorexia (weight loss of 20 kg) and a 1-month history of a non-painful breast lump with well-defined contours, which was about 6 cm in diameter. There was no history of trauma. Computed tomography of the thorax revealed a collection of liquid in the left anterior thoracic wall, associated with discontinuity of the 4th left costal cartilage, and upper left lobe cavitation, suggesting pulmonary tuberculosis. The patient was started on quadruple therapy with anti-tuberculosis drugs and discharged after a negative smear.
Conclusion: In this case, the indolent onset of unspecific symptoms made it difficult to reach a diagnosis of pulmonary tuberculosis, which was confirmed by positive culture and imaging. A breast lump in an elderly patient with unspecific clinical manifestations is an unusual presentation of pulmonary tuberculosis. It is important to be aware of rib invasion and exclude tuberculosis in a patient with a chest wall mass. As tuberculosis is treatable, early diagnosis is vital as diagnostic delay can lead to contagion.
LEARNING POINTS
- Chest wall tuberculosis is a rare complication of pulmonary tuberculosis.
- As smears and acid-fast bacilli cultures are often negative, polymerase chain reaction and imaging should be performed.
- Tuberculosis should be treated with first-line drugs; the role of surgery is still controversial.
KEYWORDS
Tuberculosis, breast lump, infectious disease, geriatric medicine
CASE REPORT
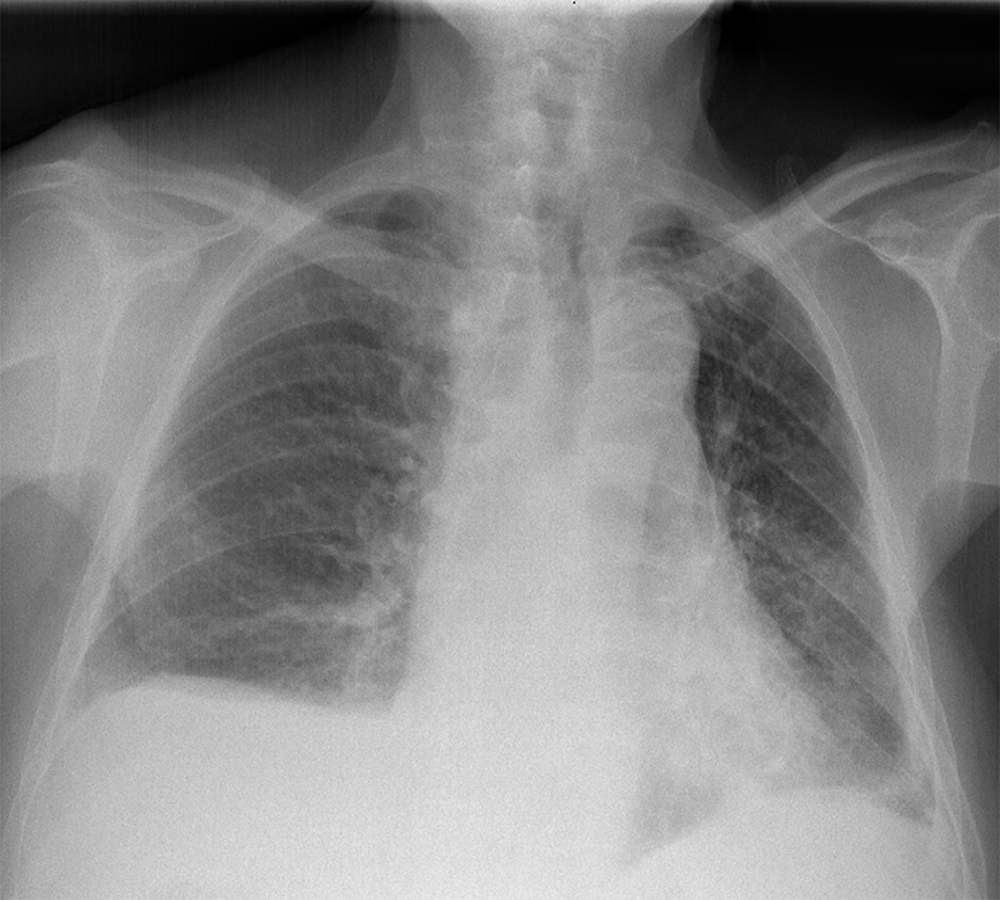
A 77-year-old man presented with depressive mood, asthenia, anorexia and weight loss of 20 kg. He also had a 1-month history of an enlarging and non-painful breast lump (Fig. 1). He did not have fever, night sweats, cough or breathlessness. He denied trauma or contact with tuberculosis. Physical examination revealed a firm and elastic mass in the internal quadrants of the left breast with well-defined contours, about 6 cm in diameter. Local temperature was normal and the overlying skin and nipple were intact. There was no evident neck or axillary palpable adenopathy. Laboratory tests showed a white blood cell count within normal limits, haemoglobin of 12.1 g/dl and C-reactive protein of 5.42 mg/dl; all other blood chemistry results were within normal limits. Radiography showed no obvious lesions (Fig. 2). Mammary ultrasound revealed in the inner quadrants of the left breast a thick-walled cystic formation measuring 69×20 mm, with detritus in the region of greatest slope. Fine needle aspiration cytology (FNAC) of a white fluid revealed a necrotic background with granulomas without neoplastic cells.
Figure 1. Enlarging and non-painful breast lump
Figure 2. Radiography did not show any lesions
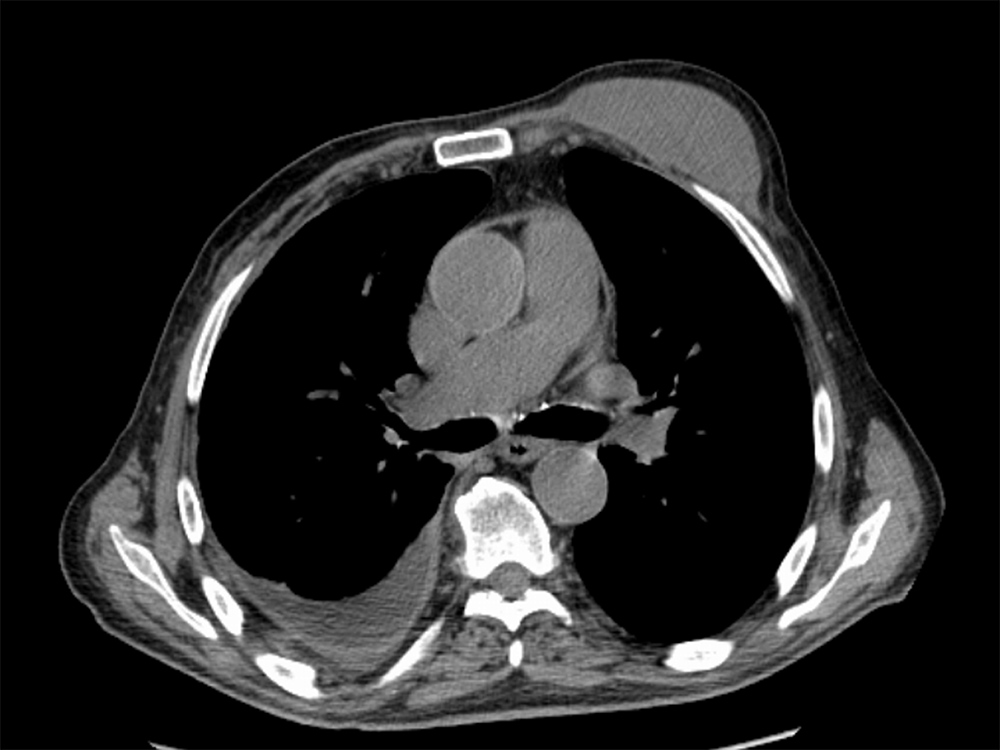
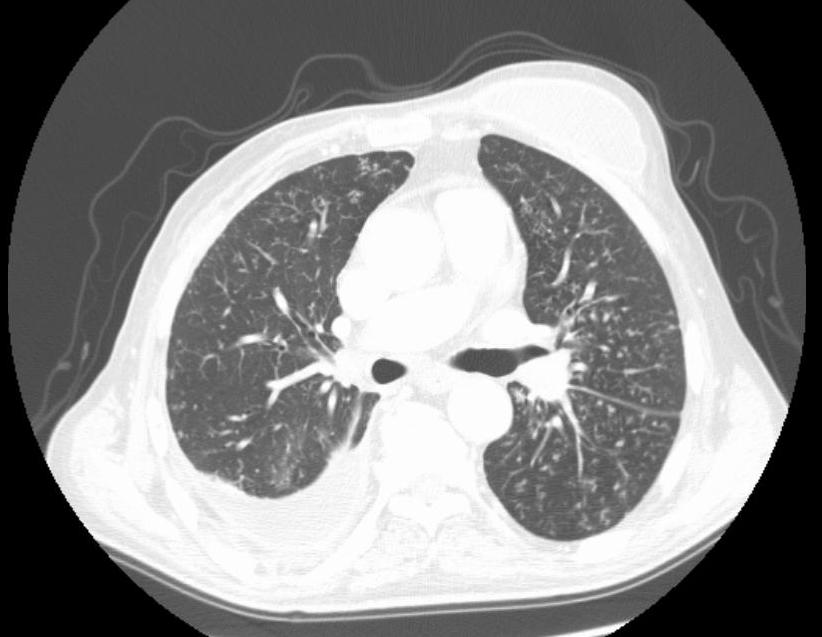
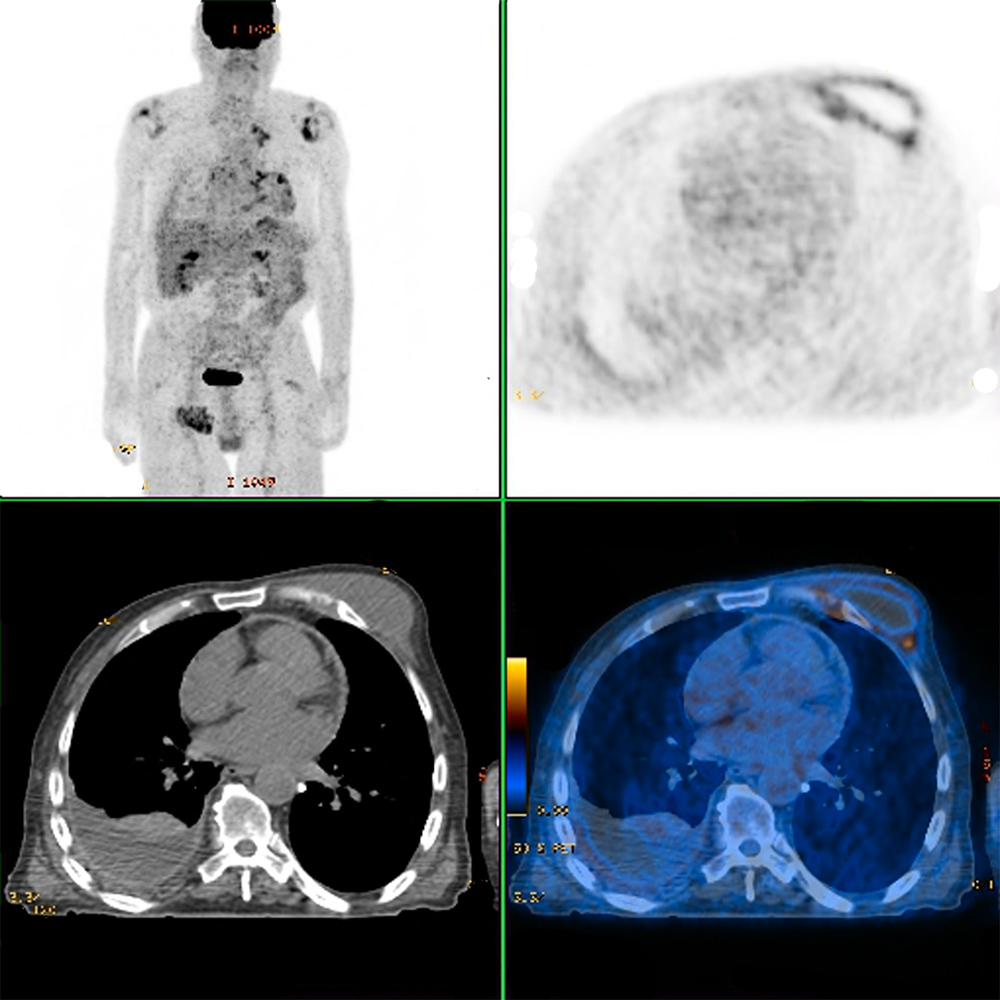
Polymerase chain reaction (PCR) and acid-fast bacilli stain of the aspirate were both positive for tuberculosis. Computed tomography (CT) of the thorax showed a liquid collection in the left anterior thoracic wall, measuring 31×80 mm, associated with irregularity and discontinuity of the 4th left costal cartilage, with a fistulous tract that crossed the cartilage into a small locus posterior to the left internal mammary artery; in the upper left lobe there was a cavitated nodule measuring 22 mm, compatible with an active tuberculous process (Figs. 3 and 4). Positron emission tomography (PET) showed a possible nodule in the left upper lobe and bilateral mediastinum-hilar adenopathy, with increased uptake of FDG-F18 (Fig. 5).
Figure 3. Computed tomography (CT) of the thorax
Figure 4. Computed tomography (CT) of the thorax showing pulmonary tuberculosis lesions
Figure 5. Positron emission tomography (PET) showing a nodule in the left upper lobe and bilaterally mediastinum-hilar adenopathy
Peripheral uptake of FDG-F18 was noted as well in a hypodense mass in the left anterior thoracic wall. An interferon-gamma release assay (IGRA) was positive and HIV serology was negative. A sputum smear was positive for acid-fast bacilli (AFB) which was also positive by Ziehl–Neelsen staining. Sputum culture was positive for Mycobacterium tuberculosis complex that was sensitive to all tested drugs. The final diagnosis was pulmonary tuberculosis (PT) with a tuberculous mass in the left anterior chest wall, as a result of direct extension from underlying pleural and pulmonary disease.
Quadruple therapy with anti-tuberculosis drugs was started: isoniazid (300 mg), rifampicin (450 mg), ethambutol (800 mg) and pyrazinamide (1500 mg). The mass did not improve with medical treatment and so was drained. The patient was discharged home following 26 days in hospital after he had improved clinically, gained weight, and three sputum smears were negative.
DISCUSSION
This case was an unusual presentation of PT, which manifested as a breast lump. Breast masses in male patients are generally caused by gynaecomastia. However, although rare, breast cancer should always be excluded[1,2]. Chest wall tuberculosis (CWT), a rare cause of breast lumps, results in destruction of bone or costal cartilage, and the formation of soft tissue masses, with or without pulmonary disease[3]. Extrapulmonary tuberculosis accounts for 10% and musculoskeletal tuberculosis for only 1–2% of all cases of tuberculosis[4,5]. The most common site is the spine, while the chest wall is affected in only 1–5% of cases of musculoskeletal tuberculosis, which corresponds to 1–2% of tuberculosis cases overall[6]. CWT is eight times more frequent in men than in women and, contrary to our case, more frequent in young and immunocompromised adults[7]. According to Tanaka et al., a risk factor for CWT could be a past history of tuberculosis, as reported in 70–80% of the participants in their study. Active tuberculosis was also present in 20–60% of their patients, as also seen in our case[8].
Three mechanisms for infection of the chest wall by mycobacteria have been proposed: direct invasion, haematogenous dissemination and lymphatic dissemination. There are few case reports of PT associated with local rib destruction (as described here), maybe because of the insidious onset and unspecific symptoms. However, paleopathological studies have found that rib lesions are more common in individuals who died of tuberculosis than in those who died of other causes, which may mean that this entity is underdiagnosed[9,10].
CWT usually manifest as a solitary, progressively enlarging, painful mass, that can be mistaken for a breast tumour[11]. Elderly patients may present with atypical clinical features, and co-morbidities can make diagnosis difficult. The elderly population is at high risk for tuberculosis and is the largest reservoir of this infection, even in developed countries[12,13].
The diagnosis of CWT can be challenging, as smears or AFB cultures are often negative. FNAC may be helpful and it is important to exclude neoplastic disease. PCR has higher sensitivity[14].
CT scanning of the chest can be valuable and typically shows osseous and cartilaginous destruction and a soft tissue mass. It is important to evaluate the lung parenchyma, extent of the mass, and rib status[15,16]. PET can be useful in the diagnosis of CWT, as the lesions have increased FDG uptake in active regions of granulomatous inflammation.
There is still no consensus regarding treatment of CWT. Medical treatment with anti-tuberculosis drugs is the first line therapy. The WHO recommends 6-month regimens, but the duration of treatment can be longer (9–12 months), depending on the clinical presentation and response to therapy[17]. Drainage and debridement seems to be the next step when medical therapy fails.
The role of surgery is not yet clear. Some reports in the literature suggest that excision helps to prevent bone and joint destruction. Kim et al. conclude that recurrence of the mass is lower when complete surgical resection is performed[18]. On the other hand, Ursavaş et al. state that surgery should be performed only if there is severe joint deformation after adequate medical therapy[19].
This case report describes an unusual presentation of PT—a breast lump in an elderly patient with unspecific clinical manifestations. The indolent clinical evolution made it difficult to achieve the diagnosis of PT, which was confirmed by positive culture and imaging. As PT is treatable, an early diagnosis is very important to cure the disease and prevent contagion.
the literature to support it. As mediastinal metastases of colon cancer are rare, the treatment strategy has yet to be established[17]. Although there are few reported cases of mediastinal metastasis from colorectal cancer, physicians should be aware of these less common locations and consider the possibility of mediastinal lymph node metastasis as a differential diagnosis. Patients should have a close follow-up in order to avoid the development of unresectable metastases, since surgery, when applicable, can lead to a better prognosis.