ABSTRACT
The case of a 25-year-old expedition doctor who developed high altitude pulmonary oedema (HAPE) while climbing in the Swiss Alps is presented, with reference to the literature. The patient's symptoms of HAPE were typical. Less typical was the fact that the doctor had previously been to similar altitudes uneventfully. The only differentiator is that on this expedition he developed a mild lower respiratory tract infection (LRTI) 2 days prior to travel. There has been limited, conflicting evidence regarding LRTI as a risk factor for HAPE and high quality research has not focused on this area. LRTI is not commonly recognised as being a risk in high altitude environments, which may be resulting in lethal consequences. This report aims to inform, provide a clinical question for future high altitude research expeditions, and encourage consideration by expedition and high altitude doctors.
LEARNING POINTS
- Lower respiratory tract infection (LRTI) may be a significant risk factor in the development of high altitude pulmonary oedema (HAPE).
- The diagnosis of HAPE is clinical as investigations have been shown to be unreliable.
- The Lake Louise HAPE criteria provide a reasonable identification framework but may miss the early stages.
KEYWORDS
High altitude pulmonary oedema; oedema; infection; respiratory; risk
INTRODUCTION
High altitude pulmonary oedema (HAPE) is a non-cardiogenic pulmonary oedema. It is generally agreed that the cause is pulmonary vasoconstriction causing pulmonary hypertension[1–4]. Publications on infection as a risk in the development of altitude illnesses are few and conflicting[5,6]. Risk factors are predominantly identified as congenital or genetic[7], which is surprising as we know that lower respiratory tract infections (LRTIs) impair gas diffusion[8]. The author has been unable to discover any publications in which a subject has ascended to high altitude repeatedly with different effects.
The incidence of HAPE ranges from 0.2% to 15.0%[9]. However, the disease burden is poorly described and can be lethal or require dangerous rescues. Recognition of potential risk factors is therefore important.
CASE DESCRIPTION
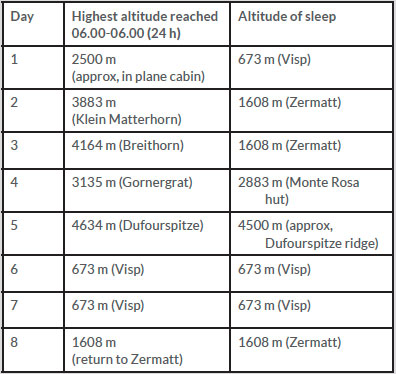
The patient planned to ascend Monte Rosa (elevation 4634 m) in the Swiss Alps. He had previously made several trips following itineraries with similar acclimatisation profiles (Table 1, Fig.1).
Two days previously, he developed a mild LRTI, producing some yellow sputum. He commenced acetazolamide as planned, as a prophylactic against acute mountain sickness. The cough settled on day 3, and he remained asymptomatic until day 5, when after 4 h (altitude 3500 m), he began experiencing subjectively decreased exercise tolerance. He was found to have normal respiratory and heart rates, and did not meet the Lake Louise HAPE criteria[10]. It was felt his experience represented a normal response to altitude. After 8 h (altitude 4200 m), the patient had dyspnoea at rest, cough, decreased exercise performance, and was tachycardic. A provisional diagnosis of HAPE was made and nifedipine commenced[11].
Descent would mean crossing a crevasse field at night, so a decision was made to continue on to a hut with communications and supplementary oxygen. At 17 h (altitude 4500 m), a rope became stuck so the patient bivouacked until morning. His respiratory rate reached 50–60 bpm, with significant orthopnoea (Fig. 2). Exercise tolerance was 10 yards. At 29 h, the patient was evacuated (to 673 m) providing significant symptomatic improvement.
Figure 1. Graph of ascent profile, sleep profile and partial pressure of oxygen against time
Figure 2. The patient (right) and climbing partner after a cold night at approximately 4500 m
INVESTIGATIONS
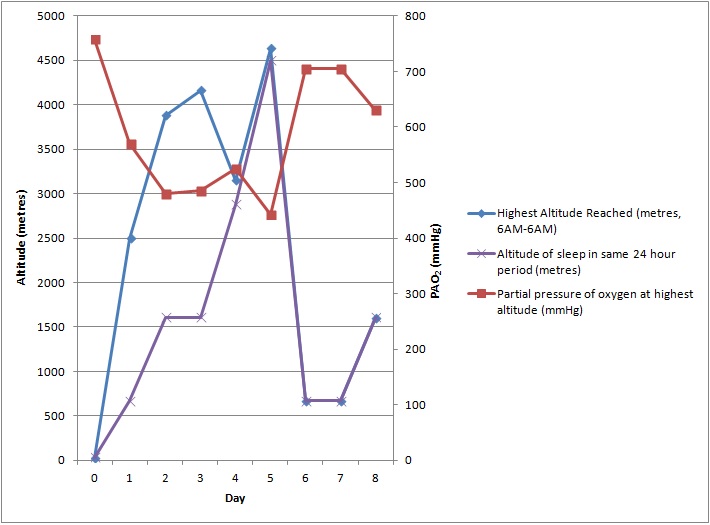
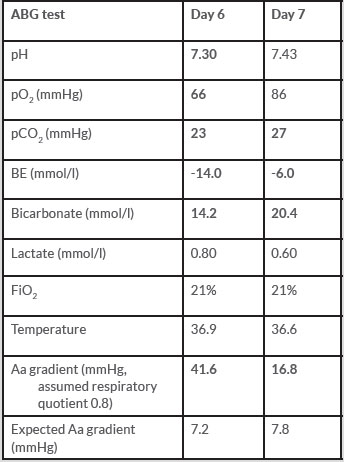
Arterial blood analysis demonstrated a metabolic acidosis (a recognised side effect of acetazolamide[12], extracellular fluid depletion[13] and ketogenesis[14]) and type 1 respiratory failure. Significant improvement was demonstrated at 24 h (Tables 2, 3).
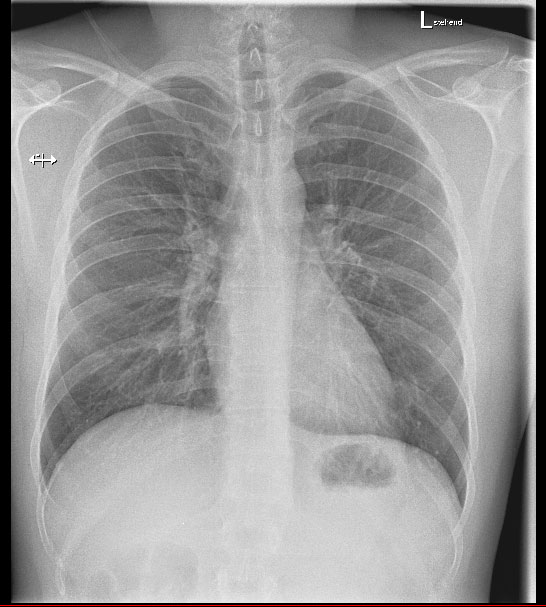
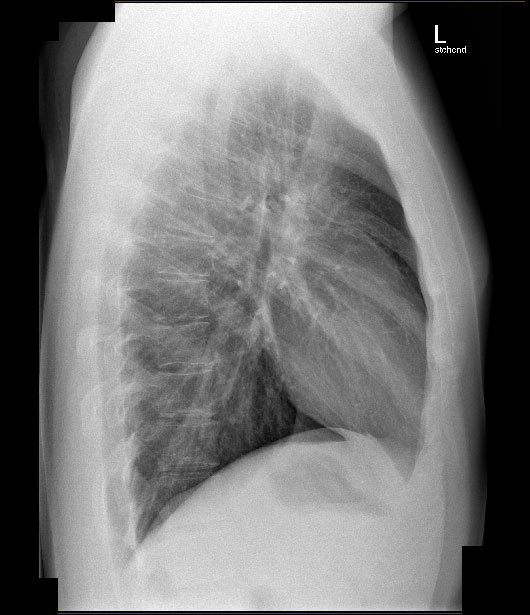
Interestingly, the chest radiograph did not demonstrate pulmonary oedema (Figs. 3, 4). It has been established that radiograph results do not correlate with pulmonary artery wedge pressure (PAWP), and that relying on the absence of radiographic findings can lead to inaccurate diagnosis[15]. Evidence for HAPE elevating PAWP is conflicting[16–18], but HAPE does produce extensive non-uniform pulmonary vasoconstriction[19], which would likely cause similar effects.
Table 2. Arterial blood gas analysis at 673 m (abnormal results in bold)
Table 3. Relevant haematology, biochemistry and urinalysis results (abnormal results in bold)
Figure 3. PA chest radiograph on arrival at the emergency department
Figure 4. Lateral chest radiograph on arrival at the emergency department
DIFFERENTIAL DIAGNOSIS
There are many causes of tachypnoea at altitude, but few cause such rapid onset and deterioration. There was no significant medical history, wheeze, smoking history, history of cardiac defect, radiographic findings, chest pain, anxiety, onset suggestive of pulmonary embolism, or findings consistent with deep vein thrombosis.
Key in the diagnosis of LRTI as a precipitating factor is that the patient had previous ascents to similar altitudes, following similar acclimatisation profiles.
The medical team made a diagnosis of:
1. HAPE
2. LRTI exacerbated by altitude.
TREATMENT
As with all cases of HAPE, the primary treatment was descent [20]. Treatment given consisted of salbutamol nebulisers (for subjective chest tightness and mucolysis), oral levofloxacin and fluid rehydration. Acetazolamide and nifedipine were discontinued due to improvement.
OUTCOME
Exercise tolerance improved to baseline over 14 days. The patient has since returned to similar altitudes without ill effect.