ABSTRACT
Plasmodium infection in human beings is often associated with complications. Complications such as cerebral malaria, acute respiratorydistress syndrome, acute kidney injury and cardiac complications including myocarditis, pericarditis and hypoglycaemia may be seen in infection by Plasmodium falciparum. However, these complications have rarely been reported with Plasmodium vivax infections. Myopericarditis complicating P. vivax malaria is particularly rare and only a few cases have been reported so far. We report on a case ofmyopericarditis due to P. vivax malaria to add to the literature.
LEARNING POINTS
- Complications like myopericarditis do occur in P.vivax infections, though they are very rare. Only a few cases of myopericarditis due to P.vivax are reported in literature till date.
- In a relevant clinical setting, prompt diagnosis and management of this life-threatening complication can be life-saving.
- Myopericarditis due to P. Vivax infection is reversible with no long term sequel.
KEYWORDS
Plasmodium vivax, malaria, myocarditis
INTRODCTION
Malarial fever continues to be an important public health problem in India. India contributes about 70% ofthe total reported cases of malaria in Southeast Asia.More than two-thirds of the Indian population live in zones where malaria is endemic. Plasmodium vivax accounts for nearly 50% of all malarial cases. Plasmodium falciparum infections are occasionally associated with complications like cerebral malaria, acute kidney injury, acute respiratory distress syndrome, severe anaemia, lactic acidosis, jaundice and hypoglycaemia. Myocarditis has also been reported. However, cardiac involvement in P. vivax infections is very rare[1-3]. We hereby report the case of a young female, 7 months pregnant, who developed myopericarditis along withacute kidney injury due to P. vivax infection.
CASE REPORT
A 27-year-old woman, 3 months pregnant, presented to us with a history of high-grade fever associatedwith rigors for 10–12 days previously. There was a history of fever spike every third day with response to antipyretics. She gave a history of yellowishdiscoloration of the eyes and high coloured urine for the last 7–8 days, generalised body swelling for the last 4–5 days, and decreased urine output andcola-coloured urine for the last 2 days. There was no history of altered mentation, convulsions, bleeding from any site or decreased foetal movements.The patient had no history of any similar illness, hypertension, diabetes or cardiac disease in the past. Two previous pregnancies had been uneventful.Onexamination, the patient was conscious, oriented and febrile (temperature 39.2°C) with BP 110/74 mmHg and pulse rate 92 beats/min. She was pale andicteric with facial puffiness and bilateral pedal oedema. Jugular venous pressure was 11 cm H2O.
On systemic examination, cardiac examination revealed a pericardial rub with holosystolic murmurs inmitral and tricuspid areas, suggestive of mitral regurgitation (MR) and tricuspid regurgitation (TR), respectively. Abdominal examination revealedcongestive hepatomegaly and a splenomegaly of 4 cm below the right costal margin, and uterus 26–28 weeks, relaxed with normal foetal heart sounds. Therest of the systemic examination was unremarkable.
On workup, her haemoglobin was 81 g/l, total leukocyte count 4,300 cells/cm3, platelet count 64,000 cells/cm3, blood urea nitrogen 19.7 mmol/l, serum creatinine 468.5 µmol/l, sodium 138 mmol/l, potassium 3.9 mmol/l and serum bilirubin 159µmol/l with a direct fraction of 122.4. Serum glutamic-pyruvic transaminase was 5.16 µkat/l and serum glutamic oxaloacetic transaminase 0.96 µkat/l. Peripheralsmear showed ring and schizont stages of P. vivax malaria. Blood and urine cultures were sterile. A Widal test and Leptospira slide macroagglutination test (MAT) were also negative. Viral serology for adenovirus, cytomegalovirus,coxsackievirus and echovirus was negative. Urinalysis revealed 12–15 red blood cells per high power field (HPF) and 2–3 pus cells/HPF with granular casts.Serum lactate dehydrogenase was raised, being 15.8 µkat/l. Arterial blood gas analysis was normal. A chest X-ray done with an abdominal shield suggestedcardiomegaly.
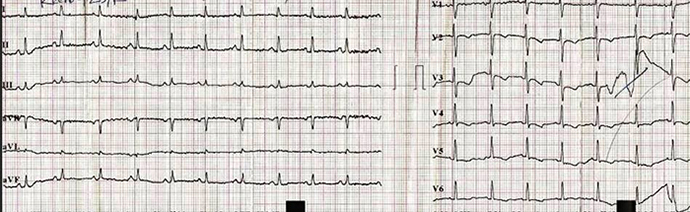
Electrocardiography (ECG) revealed sinus tachycardia with ST depression and T-wave inversion in V2–6. (Fig. 1) Echocardiography showed mildly dilated left and right ventricles, left ventricular ejection fraction of 45%,with minimal pericardial effusion, and moderate MR and TR suggestive of myopericarditis. Cardiac enzymes were sought after echocardiography and werenegative (CK-MB and Trop-T).
Artesunate-based antimalarial treatment was initiated. Fever responded and the patient improvedclinically. Laboratory parameters gradually returned to normal.
Fig. 1 - ECG showing sinus tachycardia with ST depression and T-wave inverion in V2-6
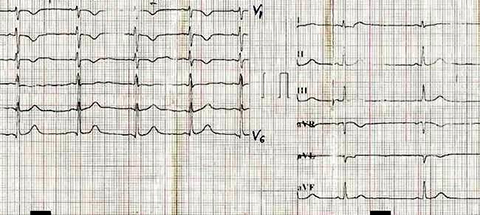
A repeat echocardiography done after 7 days showed normal cardiac chambers with ejection fraction of 55%and no pericardial effusion. A repeat ECG done on the same day showed mild residual T-wave changes in V2–3 (Fig. 2).
Fig. 2 - A repeat ECG done on the 7th day showing mild residual T-wave changes in V2-3
DISCUSSION
The mechanism of cardiac involvement in malaria is not yet fully understood, but some theories have beenproposed. It could be due to mechanical clogging of capillaries by parasitized red blood cells (PRBCs); severe acidosis may impair cardiac function. Polypeptideslike tumour necrosis factor (TNF) are also implicated in the pathophysiological process[4]. TNF-like polypeptides enhance the secretion of thrombospondin,which causes sequestration of knob-bearing PRBCs. P. vivax has been demonstrated to cause both sequestration-related as well as non-sequestration-related complications of severe malaria[5].
In our case, infection by P. vivax was confirmed by a peripheral smear, which is considered the gold standard for diagnosis of malaria and byclinical response to the treatment. The patient developed severe complications including hepatitis, acute kidney injury and severe anaemia within 4–5 days ofinitiation of fever.In view of pericardial rub and holosystolic murmurs in the mitral and tricuspid areas, echocardiography was performed and was suggestiveof myocardial involvement, along with evidence of pericarditis. Since myocarditis was not thought of earlier, cardiac enzymes were done only afterthe echocardiography and this could be the reason for the results being within normal limits. Repeat echocardiography after treatment showed reversal of thechanges observed earlier.
In a gravid female, peripartum cardiomyopathy could be thought of as a differential diagnosis.However, this rare condition more commonly occurs in the last month of pregnancy and up to five months postpartum; it is associated with multiplepregnancies in women aged >30 years. In a 7-month gravid female with a single pregnancy in the setting of uneventful previous pregnancies, with improvementin cardiac functions after antimalarial treatment, the possibility of peripartum cardiomyopathy appears highly unlikely.
Keeping in mind the clinical presentation, other complications of Plasmodium infection and reversal of the cardiac involvement, a diagnosis ofP. vivax–induced myopericarditis was made. This case report emphasizes the need to consider thepossibility of myopericarditis in cases of P. vivax–induced sepsis, since timely detection can improve prognosis.