ABSTRACT
Multiple myeloma (MM) is a plasmocytic malignant proliferation of a single clone resulting in an overabundance of monoclonal immunoglobulins. MM commonly presents with bone disorders, renal failure, anaemia and hypercalcaemia. Hyperviscosity syndrome is rare, as are vaso-occlusive symptoms. The authors report a dramatic case of an 80-year-old woman admitted to the emergency department with full-blown distal gangrene. The culprit turned out to be a MM, unusually presenting with symptomatic hyperviscosity and peripheral occlusive ischaemia. This catastrophic and particularly dramatic presentation is almost unprecedented, with only a few cases reported worldwide.
LEARNING POINTS
- New onset of peripheral vessel occlusion, especially when overlapping with symptomatic hyperviscosity, should prompt investigation for underlying haematological and/or auto-immune disorders.
- Treatment may require plasma exchange therapy, along with combination chemotherapy and corticosteroids.
- Atypical manifestations of multiple myeloma may delay the diagnosis and, thus, are associated with poorer outcomes.
KEYWORDS
Multiple myeloma, hyperviscosity, gangrene
INTRODUCTION
A multiple myeloma (MM) is a plasmocytic malignant proliferation of a single clone resulting in an overabundance of monoclonal immunoglobulins. Because MM is a multi-systemic disorder, the symptoms and signs vary greatly, but the most frequent manifestations are bone pain or fracture, renal failure, anaemia and hypercalcaemia – also known by the mnemonic CRAB: C = calcium (elevated), R = renal failure, A = anaemia and B = bone lesions. CRAB symptoms and proliferation of monoclonal plasma cells in the bone marrow are part of the diagnostic criteria of plasma cell myeloma [1].
Hyperviscosity syndrome refers to the clinical manifestations of increased serum viscosity that result from pathological changes of either the cellular or plasmatic components of the blood (Table 1).
| Author and referencesGenderAge (years) | ||
|---|---|---|
Changes in the plasmatic composition
|
Increased cellular component
|
Others
|
Table 1 - High blood viscosity causes
Classically, the syndrome is a result of increased amounts of immunoglobulin M (IgM) in Waldenstrom macroglobulinaemia. Less commonly, symptomatic blood hyperviscosity has been described in certain cases of MM, especially when abnormal polymers of IgA, IgG or kappa light chains are produced[2].
Hyperviscosity results in vascular stasis, reduced microcirculatory flow, haemostasis disorders and subsequent organ hypoperfusion. The clinical spectrum is broad, including the following:
- Mucosal bleeding to life-threatening gastrointestinal haemorrhage.
- Central nervous system involvement (Bing–Neel syndrome: hearing loss, tinnitus, vertigo, seizures, cognitive impairment).
- Cardio-respiratory symptoms.
- Clinical manifestations related to peripheral vessel occlusion: dilated retinal veins, retinal haemorrhages, purpura lesions, acrocyanosis, Raynaud phenomena and dystrophic manifestationsuntil the formation of torpid ulcers and gangrene[3,4].
CASE PRESENTATION
An 80-year-old woman was admitted to the emergency department (ED) presenting with distal quadrigangrene of the limbs and nose and variable signs of severe peripheral ischaemia and necrosis. She had a medical history of ischaemic heart disease, atrial fibrillation and vertiginous syndrome. She had been medicated accordingly and had been anticoagulated with warfarin for several years. Despite limited information, the authors learnt that, just a few months back, the patient was mentally adequate, requiring only some help with her household chores. About 2 months earlier, she started complaining of acrocyanosis, painful cold fingers of both hands and feet, and severe intermittent Raynaud phenomena, accompanied by worsening vertigo and blurred vision. She then sought private medical assistance: she was prescribed with oral corticosteroids, as warfarin was replaced with enoxaparin. No further investigations were conducted. However, the initial clinical picture rapidly unravelled to severe vaso-occlusive phenomena, resulting in peripheral ischaemic lesions/ulcerations, distal necrosis and progressive mental deterioration, ultimately sending her to our hospital's ED.
On arrival, she was stuporous, shivering, moaning and not responsive to interrogation. She was severely dehydrated, pale, cachectic, but otherwise haemodynamically stable, and had no tachypnoea, fever or lymphadenopathy. Cardiopulmonary auscultation: arrhythmia (HR around 80); basal bilateral fine crackles. Nonexudative gangrene (mummification) was observed on all four distal limbs and the nasal pyramid (Fig. 1).
Fig. 1 - Complete mummification of the fifth finger of both hands, both first toes and gangrenated tip of the nose.
Several areas of peripheral erosive lesions and livedo reticularis were also observed on the forearms, forelegs and auricles. Distal pulses were filiform, but the Doppler ultrasound showed vascular permeability. Significant laboratory findings are shown in Table 2.
| Laboratory findings |
|---|
|
Table 2 - Laboratory findings
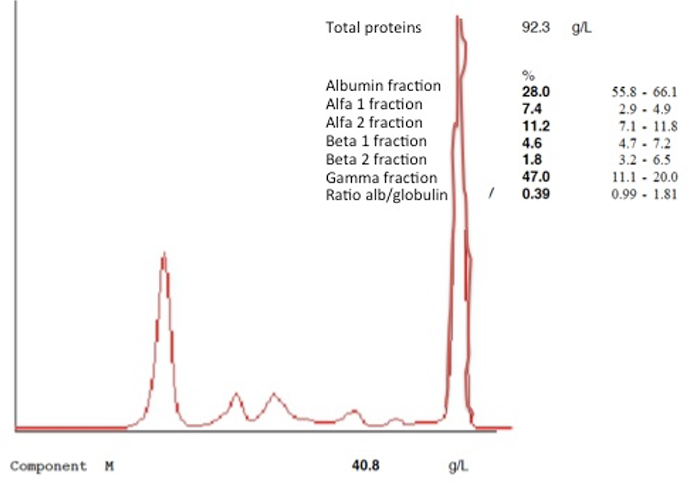
Serum protein electrophoresis and immunofixation (Fig. 2) demonstrated monoclonal gammopathy with a globulin gap of 7.18, kappa light chains of 1580 mg/dl (normal range: 170–370) and kappa/lambda ratio of 36 (normal: 1.35–2.65).
Confirmation of MM was obtained by bone marrow aspirate, which also revealed plasmacytic infiltrate of 21%.
Within the first 6 h of admission, the patient underwent prompt treatment with plasmapheresis, steroids and broad-spectrum antibiotics. At that point, there was no indication for urgent amputation, but as a safeguard for imminent need, surgical consent was obtained from her next of kin. Diagnostic confirmation did not delay the initial treatment and once myeloma was substantiated, the patient was prepared to begin combination chemotherapy. However, despite the immediate aggressive treatment, the outcome was fatal only 96 h after admission, rendering further investigation impossible.
DISCUSSION
Plasma cell myeloma is one of the most common haematological malignancies, accounting for 0.8% of all cancers worldwide[5]. However, hyperviscosity manifestations are rare, and this catastrophic and particularly dramatic form of presentation is almost unprecedented, with only a few cases reported worldwide. Mild hyperviscosity complaints, like vertigo and headache, were probably downplayed for years, however the initial vaso-occlusive phenomena should have triggered further investigation. Concurrently, the rapid progression of the disease precluded an early diagnosis.
Unfortunately, cryoglobulin testing was not performed because the correct testing conditions, such as storage, blood volume and experienced laboratory personnel, were not possible within this short time frame.
Similar case reports are remarkably scarce in the literature, ascertaining the oddity of this MM clinical presentation and compelling the authors to share their knowledge.